Abstract
Background
Internists commonly perform invasive procedures, but serious deficiencies exist in procedure training during residency.
Objective
Evaluate a comprehensive, inpatient procedure service rotation (MPS) to improve Internal Medicine residents’ comfort and self-perceived knowledge in performing lumbar puncture, abdominal paracentesis, thoracentesis, arthrocentesis, and central venous catheterization (CVC).
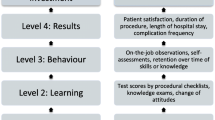
Design
The MPS comprised 1 faculty physician and 1–3 residents rotating for 2 weeks. It incorporated lectures, a textbook, instructional videos, supervised practice on mannequins, and inpatient procedures directly supervised by the faculty physician. We measured MPS impact using pre- and post-MPS rotation surveys, and surveyed all residents at academic year-end.
Measurements and Main Results
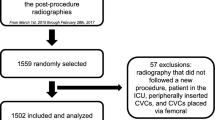
Thirty-nine categorical Internal Medicine residents completed the required rotation and surveys over the 2004–2005 academic year, performing 325 procedures. Post-MPS, the percentage of residents reporting comfort performing procedures rose 15–36% (p < .05 except for arthrocentesis, and CVC via internal jugular and femoral veins). The fraction desiring more training fell 26–51% (all p < .05). After the MPS rotation, self-rated knowledge increased in all surveyed aspects of the procedures. The year-end survey showed that improvements persisted. Comfort at year-end, for all procedures except abdominal paracentesis, was significantly higher among residents who rotated through the MPS than among those who had not. Self-reported compliance with recommended antiseptic measures was 75% for residents who completed the MPS, and 28% for those who had not (p < 0.001).
Conclusions
A comprehensive procedure service rotation of 2 weeks duration substantially improved residents’ comfort and self-perceived knowledge in performing invasive procedures. These benefits persisted at least to the end of the academic year.


Similar content being viewed by others
References
Policies and procedures for certification. Philadelphia: American Board of Internal Medicine; 1998.
Wigton RS, Alguire P. The declining number and variety of procedures done by general internists: a resurvey of members of the American College of Physicians. American College of Physicians Ann Intern Med. 2007;146(5):355–60.
Wigton RS. Measuring procedural skills. Ann Intern Med. 1996;125(12):1003–04.
Wickstrom GC, Kelley DK, Keyserling TC, Kolar MM, Dixon JG, Xie SX, et al. Confidence of academic general internists and family physicians to teach ambulatory procedures. J Gen Intern Med. 2000;15(6):353–60.
Hicks CM, Gonzalez R, Morton MT, Gibbons RV, Wigton RS, Anderson RJ. Procedural experience and comfort level in internal medicine trainees. J Gen Intern Med. 2000;15(10):716–22.
Sherertz RJ, Ely EW, Westbrook DM, Gledhill KS, Streed SA, Kiger B, et al. Education of physicians-in-training can decrease the risk for vascular catheter infection. Ann Intern Med. 2000;132(8):641–48.
Huang GC, Smith CC, Gordon CE, Feller-Kopman DJ, Davis RB, Phillips RS, et al. Beyond the comfort zone: residents assess their comfort performing inpatient medical procedures. Am J Med. 2006;119(1):71.e17–71.e24.
Wigton RS, Blank LL, Nicolas JA, Tape TG. Procedural skills training in internal medicine residencies. A survey of program directors. Ann Intern Med. 1989;111(11):932–38.
Anastakis DJ, Regehr G, Reznick RK, Cusimano M, Murnaghan J, Brown M, et al. Assessment of technical skills transfer from the bench training model to the human model. Am J Surg. 1999;177(2):167–70.
Martin M, Scalabrini B, Rioux A, Xhignesse M. Training fourth-year medical students in critical invasive skills improves subsequent patient safety. Am Surg. 2003;69(5):437–40.
Oxentenko AS, Ebbert JO, Ward LE, Pankratz VS, Wood KE. A multidimensional workshop using human cadavers to teach bedside procedures. Teach Learn Med. 2003;15(2):127–30.
Velmahos GC, Toutouzas KG, Sillin LF, Chan L, Clark RE, Theodorou D, et al. Cognitive task analysis for teaching technical skills in an inanimate surgical skills laboratory. Am J Surg. 2004;187(1):114–19.
Kohis-Gatzoulis JA, Regehr G, Hutchinson C. Teaching cognitive skills improves learning in surgical skills courses: a blinded, prospective, randomized study. Can J Surg. 2004;47(4):277–83.
Ramakrishna G, Higano ST, McDonald FS, Schultz HJ. A curricular initiative for internal medicine residents to enhance proficiency in internal jugular central venous line placement. Mayo Clin Proc. 2005;80(2):212–18.
Proano L, Jagminas L, Homan CS, Reinert S. Evaluation of a teaching laboratory using a cadaver model for tube thoracostomy. J Emerg Med. 2002;23(1):89–95.
Centers for Disease Control and Prevention. Guidelines for the prevention of intravascular catheter-related infections. MMWR Morb Mortal Wkly Rep. 2002;51(RR-10):1–29.
Chen H, Lillemoe KD, Sonnenday CJ. (eds.) In: Manual of common bedside surgical procedures. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2000.
Wigton RS, Nicolas JA, Blank LL. Procedural skills of the general internist: a survey of 2500 physicians. Ann Intern Med. 1989;111(12):1023–34.
Wigton RS. Training internists in procedural skills. Ann Intern Med. 1992;116(12 Pt 2):1091–93.
Smith C, Gordon CE, Feller-Kopman D, Huang GC, Weingart SN, Davis RB, et al. Creation of an innovative inpatient medical procedure service and a method to evaluate house staff competency. J Gen Intern Med. 2004;19(5 Pt 2):510–13.
American Board of Internal Medicine. Internal Medicine Policies. Available at: http://www.abim.org/certification/policies/imss/im.aspx#procedures. Accessed January 8, 2008.
Goldstein LB, Hey LA, Laney R. North Carolina stroke prevention and treatment facilities survey. Statewide availability of programs and services. Stroke. 2000;31(1):66–70.
Fincher RM. Procedural competence of internal medicine residents: time to address the gap. J Gen Intern Med. 2000;15(6):432–33.
Acknowledgment
The authors are indebted to the following people for making it possible to perform this study: Drs. Lee Tai, Advocate Christ Medical Center, Oak Lawn, IL; Michael McFarlane, MetroHealth Medical Center, Cleveland, OH; Richard Christie, St. Vincent Charity Hospital, Cleveland, OH; and K. V. Gopalakrishna, Fairview Hospital, Cleveland, OH. There were no specific sources of financial support for this study.
Conflict of Interest Statement
None disclosed.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lenhard, A., Moallem, M., Marrie, R.A. et al. An Intervention to Improve Procedure Education for Internal Medicine Residents. J GEN INTERN MED 23, 288–293 (2008). https://doi.org/10.1007/s11606-008-0513-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-008-0513-4