Summary
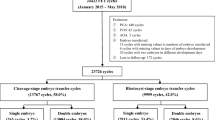
This study compared the clinical outcomes of the frozen-thawed cycles of high-quality cleavage embryos with low-quality blastocysts to provide a reference for the choice of frozen-thawed embryo transfer schemes and to improve clinical pregnancy rates. A retrospective analysis was performed on the clinical data of patients undergoing frozen-thawed embryo transfer at the Reproductive Medicine Center of Tongji Hospital of Tongji Medical College of Huazhong University of Science and Technology from 2016 to 2017. In total, 845 cases were divided into a high-quality cleavage embryo group (group A) and a low-quality blastocyst group (group B). Each group was further divided into subgroups based on the number of transplants. Group A was categorized into two subgroups comprising of 94 cases in subgroup A1 (1 high-quality 8-cell group) and 201 cases in subgroup A2 (2 high-quality 8-cell group). Group B was divided into four subgroups consisting of 73 cases in subgroup B1 (D53BC group), 65 cases in subgroup B2 (D54BC group), 110 cases in subgroup B3 (D63BC group), and 282 cases in subgroup B4 (D64BC group). The pregnancy outcomes and neonatal outcomes between the groups were compared. The clinical pregnancy rates (56.72% and 60.00%) and live birth rates (47.76% and 46.15%) in subgroups A2 and B2 showed no significant differences, but these rates were significantly higher in subgroups A2 and B2 than in the rest subgroups (P<0.05). The multiple birth rate (26.32%) in the subgroup A2 was significantly higher than that in the rest subgroups (P<0.05). There were no statistically significant differences in the abortion rates among all groups (P>0.05). In terms of neonatal outcomes, there were no statistically significant differences in the proportion of premature births, sex ratios, and birth defects among the low-weight and gigantic infants (P>0.05). Transplanting two high-quality cleavage embryos during the frozen-thawed embryo transfer cycles could significantly increase clinical pregnancy rates and live birth rates, but at the same time, it also increased the risks of multiple births and complications to mothers and infants. The D54BC subgroup had the most significant advantages among all groups (P<0.05). The rest low-quality blastocysts had clinical outcomes similar to the single high-quality cleavage embryo group.
Similar content being viewed by others
References
Martins WP, Nastri CO, Rienzi L, et al. Blastocyst vs cleavage-stage embryo transfer: systematic review and meta-analysis of reproductive outcomes. Ultrasound Obst Gyn, 2017,49 (5):583–591
Gharenaz NM, Movahedin M, Mazaheri Z. Effects of re-vitrification of mouse morula and early blastocyst stages on apoptotic gene expression and developmental potential. Cell J, 2018,19(4):614–619
Gardner DK, Lane M, Stevens J, et al. Blastocyst score affects implantation and pregnancy outcome: towards a single blastocyst transfer. Fertil Steril, 2000,73(6):1155–1158
Rienzi L, Cimadomo D, Delgado A, et al. Time of morulation and trophectoderm quality are predictors of a live birth after euploid blastocyst transfer: a multicenter study. Fertil Steril, 2019,112(6):1080–1093
Du T, Wang Y, Fan Y, et al. Fertility and neonatal outcomes of embryos achieving blastulation on Day 7: are they of clinical value? Hum Reprod, 2018,33(6):1038–1051
Ferreux L, Bourdon M, Sallem A, et al. Live birth rate following frozen-thawed blastocyst transfer is higher with blastocysts expanded on Day 5 than on Day 6. Hum Reprod, 2018,33(3):390–398
Devine K, Richter KS, Widra EA, et al. Vitrified blastocyst transfer cycles with the use of only vaginal progesterone replacement with Endometrin have inferior ongoing pregnancy rates: results from the planned interim analysis of a three-arm randomized controlled noninferiority trial. Fertil Steril, 2018,109(2):266–275
Tannus S, Cohen Y, Son WY, et al. Cumulative live birth rate following elective single blastocyst transfer compared with double blastocyst transfer in women aged 40 years and over. Reprod Biomed Online, 2017,35(6):S490–S490
Yang L, Cai S, Zhang S, et al. Single embryo transfer by Day 3 time-lapse selection versus Day 5 conventional morphological selection: a randomized, open-label, non-inferiority trial. Hum Reprod, 2018,33(5):869–876
Ren XL, Zhang HW, Liu Q, et al. Analysis of influencing factors of single blastocyst transplantation during resuscitation cycle. Acta Med Univ Sci Technol Huazhong (Chinese), 2011,40(06):742–745
Thompson SM, Onwubalili N, Brown K, et al. Blastocyst expansion score and trophectoderm morphology strongly predict successful clinical pregnancy and live birth following elective single embryo blastocyst transfer (eSET): a national study. J Assist Reprod Genet, 2013,30(12):1577–1581
Du SR, Lin YH, Lin DL, et al. Relationship between single blastocyst score and fertility outcome during the resuscitation cycle. China Maternal Child Health Care (Chinese), 2016,31(10):2144–2146
Du QY, Wang EY, Huang Y, et al. Blastocoele expansion degree predicts live birth after single blastocyst transfer for fresh and vitrified/warmed single blastocyst transfer cycles. Fertil Steril, 2016,105(4):910–919.e1
Ahlstrom A, Westin C, Wikland M, et al. Prediction of live birth in frozen-thawed single blastocyst transfer cycles by pre-freeze and post-thaw morphology. Hum Reprod, 2013,28(5):1199–1209
Lundin K. Association between blastocyst morphology and outcome of single-blastocyst transfer. Reprod Biomed Online, 2013,27(4):353–361
Sunkara SK, Siozos A, Bolton VN, et al. The influence of delayed blastocyst formation on the outcome of frozen-thawed blastocyst transfer: a systematic review and meta-analysis. Hum Reprod (Oxford, England), 2010,25(8):1906–1915
Guo N, Deng TR, Hua X, et al. Discussion on the clinical application value of blastocysts with different development speed in the single blastocyst freezing and thawing cycle. Maternal Child Health Care China (Chinese), 2019,34(08):1811–1515
Wu LM, Zou WW, Ji DM, et al. Analysis of pregnancy outcomes after freeze-thaw transplantation of blastocysts with different development days. Chinese J Reprod Contracep (Chinese), 2017,37(10):779–785
Yan FY, Li XJ, Lu Q, et al. Correlation between in vitro fertilization and blastocyst culture and D_2D_3 embryo blastomere number and fragment rating. J Pract Clin Med (Chinese), 2014,18(17):70–72
Wei YL, Zhu GJ, Ren XL, et al. Developmental Potential and Clinical Value of Embryos with Abnormal Cleavage Rate. Curr Med Sci, 2019,39(1):118–121
Acknowledgements
We acknowledge the contributions of whole staff of our reproductive medicine center.
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was supported by grants from National Key R&D Program of China (No. 2018YFC1002103) and Natural Science Foundation of China (No. 81801531).
Conflict of Interest Statement
The authors report no conflicts of interest in this study.
Rights and permissions
About this article
Cite this article
Wei, Yl., Huang, B., Ren, Xl. et al. High-quality Cleavage Embryo versus Low-quality Blastocyst in Frozen-thawed Cycles: Comparison of Clinical Outcomes. CURR MED SCI 40, 968–972 (2020). https://doi.org/10.1007/s11596-020-2254-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-020-2254-5