Abstract
Background
Branch duct-intraductal papillary mucinous neoplasms (BD-IPMNs) are the most common pancreatic cystic tumors and have a low risk of malignant transformation. Features able to early identify high-risk BD-IPMNs are lacking, and guidelines currently rely on the occurrence of worrisome features (WF) and high-risk stigmata (HRS).
Aim
In our study, we aimed to use a magnetic resonance imaging (MRI) radiomic model to identify features linked to a higher risk of malignant degeneration, and whether these appear before the occurrence of WF and HRS.
Methods
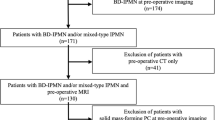
We retrospectively evaluated adult patients with a known BD-IPMN who had had at least two contrast-enhanced MRI studies at our center and a 24-month minimum follow-up time. MRI acquisition protocol for the two examinations included pre- and post-contrast phases and diffusion-weighted imaging (DWI)/apparent diffusion coefficient (ADC) map. Patients were divided into two groups according to the development of WF or HRS at the end of the follow-up (Group 0 = no WF or HRS; Group 1 = WF or HRS). We segmented the MRI images and quantitative features were extracted and compared between the two groups. Features that showed significant differences (SF) were then included in a LASSO regression method to build a radiomic-based predictive model.
Results
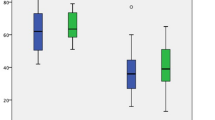
We included 50 patients: 31 in Group 0 and 19 in Group 1. No patients in this cohort developed HRS. At baseline, 47, 67, 38, and 68 SF were identified for pre-contrast T1-weighted (T1-W) sequence, post-contrast T1-W sequence, T2-weighted (T2- W) sequence, and ADC map, respectively. At the end of follow-up, we found 69, 78, 53, and 91 SF, respectively. The radiomic-based predictive model identified 16 SF: more particularly, 5 SF for pre-contrast T1-W sequence, 6 for post-contrast T1-W sequence, 3 for T2-W sequence, and 2 for ADC.
Conclusion
We identified radiomic features that correlate significantly with WF in patients with BD-IPMNs undergoing contrast-enhanced MRI. Our MRI-based radiomic model can predict the occurrence of WF.




Similar content being viewed by others
References
Klöppel G, Basturk O, Schlitter AM, Konukiewitz B, Esposito I (2014) Intraductal neoplasms of the pancreas. Semin Diagn Pathol 31(6):452–466. https://doi.org/10.1053/j.semdp.2014.08.005
Grazzini G, Danti G, Cozzi D, Lanzetta MM, Addeo G, Falchini M, Masserelli A, Pradella S, Miele V (2019) Diagnostic imaging of gastrointestinal neuroendocrine tumours (GI-NETs): relationship between MDCT features and 2010 WHO classification. Radiol Med 124(2):94–102. https://doi.org/10.1007/s11547-018-0946-8
Danti G, Flammia F, Matteuzzi B, Cozzi D, Berti V, Grazzini G, Pradella S, Recchia L, Brunese L, Miele V (2021) Gastrointestinal neuroendocrine neoplasms (GI-NENs): hot topics in morphological, functional, and prognostic imaging. Radiol Med 126(12):1497–1507. https://doi.org/10.1007/s11547-021-01408-x
Chiti G, Grazzini G, Flammia F, Matteuzzi B, Tortoli P, Bettarini S, Pasqualini E, Granata V, Busoni S, Messserini L, Pradella S, Massi D, Miele V (2022) Gastroenteropancreatic neuroendocrine neoplasms (GEP-NENs): a radiomic model to predict tumor grade. Radiol Med 127(9):928–938. https://doi.org/10.1007/s11547-022-01529-x
Addeo G, Beccani D, Cozzi D, Ferrari R, Lanzetta MM, Paolantonio P, Pradella S, Miele V (2019) Groove pancreatitis: a challenging imaging diagnosis. Gland Surg 8(Suppl 3):S178-s187. https://doi.org/10.21037/gs.2019.04.06
Moris M, Bridges MD, Pooley RA, Raimondo M, Woodward TA, Stauffer JA, Asbun HJ, Wallace MB (2016) Association between advances in high-resolution cross-section imaging technologies and increase in prevalence of pancreatic cysts from 2005 to 2014. Clin Gastroenterol Hepatol 14(4):585-593.e583. https://doi.org/10.1016/j.cgh.2015.08.038
Tanaka M, Fernández-Del Castillo C, Kamisawa T, Jang JY, Levy P, Ohtsuka T, Salvia R, Shimizu Y, Tada M, Wolfgang CL (2017) Revisions of international consensus Fukuoka guidelines for the management of IPMN of the pancreas. Pancreatology 17(5):738–753. https://doi.org/10.1016/j.pan.2017.07.007
Berland LL, Silverman SG, Gore RM, Mayo-Smith WW, Megibow AJ, Yee J, Brink JA, Baker ME, Federle MP, Foley WD, Francis IR, Herts BR, Israel GM, Krinsky G, Platt JF, Shuman WP, Taylor AJ (2010) Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J Am Coll Radiol 7(10):754–773. https://doi.org/10.1016/j.jacr.2010.06.013
Granata V, Grassi R, Fusco R, Setola SV, Palaia R, Belli A, Miele V, Brunese L, Petrillo A, Izzo F (2020) Assessment of ablation therapy in pancreatic cancer: the radiologist’s challenge. Front Oncol 10:560952. https://doi.org/10.3389/fonc.2020.560952
Goh BK, Thng CH, Tan DM, Low AS, Wong JS, Cheow PC, Chow PK, Chung AY, Wong WK, Ooi LL (2014) Evaluation of the Sendai and 2012 international consensus guidelines based on cross-sectional imaging findings performed for the initial triage of mucinous cystic lesions of the pancreas: a single institution experience with 114 surgically treated patients. Am J Surg 208(2):202–209. https://doi.org/10.1016/j.amjsurg.2013.09.031
Nguyen AH, Toste PA, Farrell JJ, Clerkin BM, Williams J, Muthusamy VR, Watson RR, Tomlinson JS, Hines OJ, Reber HA, Donahue TR (2015) Current recommendations for surveillance and surgery of intraductal papillary mucinous neoplasms may overlook some patients with cancer. J Gastrointest Surg 19(2):258–265. https://doi.org/10.1007/s11605-014-2693-z
Grassi R, Miele V, Giovagnoni A (2019) Artificial intelligence: a challenge for third millennium radiologist. Radiol Med 124(4):241–242. https://doi.org/10.1007/s11547-019-00990-5
Hassani C, Saremi F, Varghese BA, Duddalwar V (2020) Myocardial radiomics in cardiac MRI. AJR Am J Roentgenol 214(3):536–545. https://doi.org/10.2214/ajr.19.21986
Neri E, Coppola F, Miele V, Bibbolino C, Grassi R (2020) Artificial intelligence: who is responsible for the diagnosis? Radiol Med 125(6):517–521. https://doi.org/10.1007/s11547-020-01135-9
Scapicchio C, Gabelloni M, Barucci A, Cioni D, Saba L, Neri E (2021) A deep look into radiomics. Radiol Med 126(10):1296–1311. https://doi.org/10.1007/s11547-021-01389-x
Cusumano D, Meijer G, Lenkowicz J, Chiloiro G, Boldrini L, Masciocchi C, Dinapoli N, Gatta R, Casà C, Damiani A, Barbaro B, Gambacorta MA, Azario L, De Spirito M, Intven M, Valentini V (2021) A field strength independent MR radiomics model to predict pathological complete response in locally advanced rectal cancer. Radiol Med 126(3):421–429. https://doi.org/10.1007/s11547-020-01266-z
Santone A, Brunese MC, Donnarumma F, Guerriero P, Mercaldo F, Reginelli A, Miele V, Giovagnoni A, Brunese L (2021) Radiomic features for prostate cancer grade detection through formal verification. Radiol Med 126(5):688–697. https://doi.org/10.1007/s11547-020-01314-8
Chiloiro G, Cusumano D, de Franco P, Lenkowicz J, Boldrini L, Carano D, Barbaro B, Corvari B, Dinapoli N, Giraffa M, Meldolesi E, Manfredi R, Valentini V, Gambacorta MA (2022) Does restaging MRI radiomics analysis improve pathological complete response prediction in rectal cancer patients? A prognostic model development. Radiol Med 127(1):11–20. https://doi.org/10.1007/s11547-021-01421-0
Kumar V, Gu Y, Basu S, Berglund A, Eschrich SA, Schabath MB, Forster K, Aerts HJ, Dekker A, Fenstermacher D, Goldgof DB, Hall LO, Lambin P, Balagurunathan Y, Gatenby RA, Gillies RJ (2012) Radiomics: the process and the challenges. Magn Reson Imaging 30(9):1234–1248. https://doi.org/10.1016/j.mri.2012.06.010
Palatresi D, Fedeli F, Danti G, Pasqualini E, Castiglione F, Messerini L, Massi D, Bettarini S, Tortoli P, Busoni S, Pradella S, Miele V (2022) Correlation of CT radiomic features for GISTs with pathological classification and molecular subtypes: preliminary and monocentric experience. Radiol Med 127(2):117–128. https://doi.org/10.1007/s11547-021-01446-5
Gregucci F, Fiorentino A, Mazzola R, Ricchetti F, Bonaparte I, Surgo A, Figlia V, Carbonara R, Caliandro M, Ciliberti MP, Ruggieri R, Alongi F (2022) Radiomic analysis to predict local response in locally advanced pancreatic cancer treated with stereotactic body radiation therapy. Radiol Med 127(1):100–107. https://doi.org/10.1007/s11547-021-01422-z
Gillies RJ, Kinahan PE, Hricak H (2016) Radiomics: images are more than pictures they are data. Radiology 278(2):563–577. https://doi.org/10.1148/radiol.2015151169
Fusco R, Granata V, Mazzei MA, Meglio ND, Roscio DD, Moroni C, Monti R, Cappabianca C, Picone C, Neri E, Coppola F, Montanino A, Grassi R, Petrillo A, Miele V (2021) Quantitative imaging decision support (QIDS(TM)) tool consistency evaluation and radiomic analysis by means of 594 metrics in lung carcinoma on chest CT scan. Cancer Control 28:1073274820985786. https://doi.org/10.1177/1073274820985786
Kuwahara T, Hara K, Mizuno N, Okuno N, Matsumoto S, Obata M, Kurita Y, Koda H, Toriyama K, Onishi S, Ishihara M, Tanaka T, Tajika M, Niwa Y (2019) Usefulness of deep learning analysis for the diagnosis of malignancy in intraductal papillary mucinous neoplasms of the pancreas. Clin Transl Gastroenterol 10(5):1–8. https://doi.org/10.14309/ctg.0000000000000045
Cui S, Tang T, Su Q, Wang Y, Shu Z, Yang W, Gong X (2021) Radiomic nomogram based on MRI to predict grade of branching type intraductal papillary mucinous neoplasms of the pancreas: a multicenter study. Cancer Imaging 21(1):26. https://doi.org/10.1186/s40644-021-00395-6
Hanania AN, Bantis LE, Feng Z, Wang H, Tamm EP, Katz MH, Maitra A, Koay EJ (2016) Quantitative imaging to evaluate malignant potential of IPMNs. Oncotarget 7(52):85776–85784. https://doi.org/10.18632/oncotarget.11769
Rizzo S, Botta F, Raimondi S, Origgi D, Fanciullo C, Morganti AG, Bellomi M (2018) Radiomics: the facts and the challenges of image analysis. Eur Radiol Exp 2(1):36. https://doi.org/10.1186/s41747-018-0068-z
Sahora K, Mino-Kenudson M, Brugge W, Thayer SP, Ferrone CR, Sahani D, Pitman MB, Warshaw AL, Lillemoe KD, Fernandez-del Castillo CF (2013) Branch duct intraductal papillary mucinous neoplasms: does cyst size change the tip of the scale? A critical analysis of the revised international consensus guidelines in a large single-institutional series. Ann Surg 258(3):466–475. https://doi.org/10.1097/SLA.0b013e3182a18f48
Innocenti T, Danti G, Lynch EN, Dragoni G, Gottin M, Fedeli F, Palatresi D, Biagini MR, Milani S, Miele V, Galli A (2022) Higher volume growth rate is associated with development of worrisome features in patients with branch duct-intraductal papillary mucinous neoplasms. World J Clin Cases 10(17):5667–5679. https://doi.org/10.12998/wjcc.v10.i17.5667
Attiyeh MA, Fernández-Del Castillo C, Al Efishat M, Eaton AA, Gönen M, Batts R, Pergolini I, Rezaee N, Lillemoe KD, Ferrone CR, Mino-Kenudson M, Weiss MJ, Cameron JL, Hruban RH, D’Angelica MI, DeMatteo RP, Kingham TP, Jarnagin WR, Wolfgang CL, Allen PJ (2018) Development and validation of a multi-institutional preoperative nomogram for predicting grade of dysplasia in intraductal papillary mucinous neoplasms (IPMNs) of the pancreas: a report from the pancreatic surgery consortium. Ann Surg 267(1):157–163. https://doi.org/10.1097/sla.0000000000002015
Hoffman DH, Ream JM, Hajdu CH, Rosenkrantz AB (2017) Utility of whole-lesion ADC histogram metrics for assessing the malignant potential of pancreatic intraductal papillary mucinous neoplasms (IPMNs). Abdom Radiol (NY) 42(4):1222–1228. https://doi.org/10.1007/s00261-016-1001-7
Tang TY, Li X, Zhang Q, Guo CX, Zhang XZ, Lao MY, Shen YN, Xiao WB, Ying SH, Sun K, Yu RS, Gao SL, Que RS, Chen W, Huang DB, Pang PP, Bai XL, Liang TB (2020) Development of a novel multiparametric mri radiomic nomogram for preoperative evaluation of early recurrence in resectable pancreatic Cancer. In: J Magn Reson Imaging, vol 52. vol 1. © 2019 The Authors. Journal of Magnetic Resonance Imaging published by Wiley Periodicals, Inc. on behalf of International Society for Magnetic Resonance in Medicine., United States, pp 231–245. doi:https://doi.org/10.1002/jmri.27024
Polk SL, Choi JW, McGettigan MJ, Rose T, Ahmed A, Kim J, Jiang K, Balagurunathan Y, Qi J, Farah PT, Rathi A, Permuth JB, Jeong D (2020) Multiphase computed tomography radiomics of pancreatic intraductal papillary mucinous neoplasms to predict malignancy. World J Gastroenterol 26(24):3458–3471. https://doi.org/10.3748/wjg.v26.i24.3458
Correa-Gallego C, Do R, Lafemina J, Gonen M, D’Angelica MI, DeMatteo RP, Fong Y, Kingham TP, Brennan MF, Jarnagin WR, Allen PJ (2013) Predicting dysplasia and invasive carcinoma in intraductal papillary mucinous neoplasms of the pancreas: development of a preoperative nomogram. Ann Surg Oncol 20(13):4348–4355. https://doi.org/10.1245/s10434-013-3207-z
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest.
Ethical approval
The research did not involve human and/or animal participants. Patients signed informed consent form. The study was approved by the Biomedical Research Ethics Committee of our institution (protocol number: 20256_oss) and conformed to the criteria of the Declaration of Helsinki on Ethical Principles and Good Clinical Practice.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Flammia, F., Innocenti, T., Galluzzo, A. et al. Branch duct-intraductal papillary mucinous neoplasms (BD-IPMNs): an MRI-based radiomic model to determine the malignant degeneration potential. Radiol med 128, 383–392 (2023). https://doi.org/10.1007/s11547-023-01609-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01609-6