Abstract
Purpose
To perform contrast analysis of the relationship between high-resolution computed tomography (HRCT) signs and new pathologic classification of small GGNs-like lung adenocarcinoma.
Materials and methods
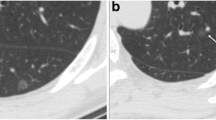
The HRCT data from 145 pathologically confirmed cases of small GGNs of lung adenocarcinoma were analysed retrospectively. The 145 cases of GGNs were divided into pre-invasive (PI) group (n = 46), micro-invasive adenocarcinoma (MIA) group (n = 48), and invasive adenocarcinoma (IAC) group (n = 51). HRCT imaging sign of GGNs in each group was assessed and compared.
Results
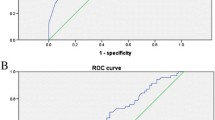
Significant differences in GGN size were found among the three groups (P < 0.05). The presence of a tumour–lung interface in the MIA and IAC groups was significantly higher than that in the PI group (P < 0.05), but no significant difference was found between the MIA and IAC groups. The presence of a pleural indentation sign in the IAC group was significantly higher than that in the other two groups (P < 0.05), but no significant difference was noted between the latter two groups. Significant differences were found in the lobulated and spicule signs among the three groups (P < 0.05). The presence of a microvascular sign in the MIA and IAC groups was significantly higher than that in the PI group (P < 0.05). No significant difference was found in the GGN density, vacuole sign, air bronchus sign and notch sign among the three groups.
Conclusions
The HRCT signs of GGNs could be used to differentiate among pre-invasive lesions, micro-invasive lesions and invasive lung adenocarcinoma.





Similar content being viewed by others
References
Godoy MC, Naidich DP (2012) Overview and strategic management of subsolid pulmonary nodules. J Thorac Imaging 27:240–248
Lee HY, Choi YL, Lee KS et al (2014) Pure ground-glass opacity neoplastic lung nodules: histopathology, imaging, and management. AJR Am J Roentgenol 202:W224–W233
Kodama K, Higashiyama M, Yokouchi H et al (2001) Prognostic value of ground-glass opacity found in small lung adenocarcinoma on high-resolution CT scanning. Lung Cancer 33:17–25
Goo JM, Park CM, Lee HJ (2011) Ground-glass nodules on chest CT as imaging biomarkers in the management of lung adenocarcinoma. AJR 196:533–543
Travis WD, Brambilla E, Noguchi M et al (2011) International association for the study of lung cancer/american thoracic society/european respiratory society international muhidisciplinary classification of lung adenocarcinoma. J Thorac Oncol 6:244–285
Yoshizawa A, Motoi N, Riely GJ et al (2011) Impact of proposed IASLC/ATS/ERS classification of lung adenocarcinoma: prognostic subgroups and implications for further revision of staging based on analysis of 514 stage I cases. Mod Pathol 24:653–664
Travis WD, Brambilla E, Riely GJ (2013) New pathologic classification of lung cancer: relevance for clinical practice and clinical trials. J Clin Oncol 31:992–1001
Lee SM, Park CM, Goo JM et al (2013) Invasive pulmonary adenocarcinomas versus preinvasive lesions appearing as ground-glass nodules: differentiation by using CT features. Radiology 268:265–273
Kazerooni EA (2001) High-resolution CT of the lungs. AJR 177:501–519
Min JH, Lee HY, Lee KS et al (2010) Stepwise evolution from a focal pure pulmonary ground-glass opacity nodule into an invasive lung adenocarcinoma: an observation for more than 10 years. Lung Cancer 69:123–126
Tsutani Y, Miyata Y, Nakayama H et al (2014) Appropriate sublobar resection choice ground glass opacity–dominant clinical stage IA adenocarcinoma. Wedge resection or segmentectomy. Chest 145:66–71
Sakurai H, Asamura H (2014) Sublobar resection for early-stage lung cancer. Transl Lung Cancer Res 3:164–172
Cho KS, Kim SJ, Lee YJ et al (2014) Surgical resection of nodular ground-glass opacities without percutaneous needle aspiration or biopsy. BMC Cancer 14:838
Lim HJ, Ahn S, Lee KS et al (2013) Persistent pure ground-glass opacity lung nodules >/= 10 mm in diameter at CT scan: histopathologic comparisons and prognostic implications. Chest 144:1291–1299
Lee HY, Jeong JY, Lee KS et al (2012) Solitary pulmonary nodular lung adenocarcinoma: correlation of histopathologic scoring and patient survival with imaging biomarkers. Radiology 264:884–893
Eguchi T, Yoshizawa A, Kawakami S et al (2014) Tumor size and computed tomography attenuation of pulmonary pure ground-glass nodules are useful for predicting pathological invasiveness. PLoS ONE 9:e97867
Fan L, Liu SY, Li QC et al (2012) Multidetector CT features of pulmonary focal ground-glass opacity: differences between benign and malignant. Br J Radiol 85:897–904
Heo EY, Lee KW, Jheon S et al (2011) Surgical resection of highly suspicious pulmonary nodules without a tissue diagnosis. Jpn J Clin Oncol 41:1017–1022
Ichinose J, Kohno T, Fujimori S et al (2014) Invasiveness and malignant potential of pulmonary lesions presenting as pure ground-glass opacities. Ann Thorac Cardiovasc Surg 20:347–352
Nambu A, Araki T, Taguchi Y et al (2005) Focal area of ground-glass opacity and ground-glass opacity predominance on thin-section CT: discrimination between neoplastic and non-neoplastic lesions. Clin Radiol 60:1006–1017
Ito T, Murakawa T, Sato H et al (2012) Simple preoperative computed tomography image analysis shows good predictive performance for pathological vessel invasion in clinical stage IA non-small cell lung cancer. Interact CardioVasc Thorac Surg 15:633–638
Liang J, Xu XQ, Xu H et al (2015) Using the CT features to differentiate invasive pulmonary adenocarcinoma from pre-invasive lesion appearing as pure or mixed ground-glass nodules. Br J Radiol 88:20140811
Acknowledgements
We thank Mr. Zhang for the English revision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Meng, Y., Liu, CL., Cai, Q. et al. Contrast analysis of the relationship between the HRCT sign and new pathologic classification in small ground glass nodule-like lung adenocarcinoma. Radiol med 124, 8–13 (2019). https://doi.org/10.1007/s11547-018-0936-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-018-0936-x