Abstract
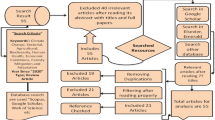
Climate variations cause public health problems, but the literature is still scarce on studies involving health interventions against climate-sensitive diseases. The objective of this review was to identify health interventions for the prevention of such diseases. We conducted a scoping review using the JBI Methodology. Six large research databases were searched (PubMed, Scopus, Web of Science, Lilacs, Embase, and Cochrane). The following inclusion criterion was used: studies addressing health interventions to prevent climate-sensitive diseases or consequences of climate on people’s health. The exclusion criteria consisted of thesis, dissertations, conference proceedings, studies with unclear information/methodology, and studies not addressing climate-related health interventions. No language or date restrictions were applied. Of 733 studies identified and screened by title and abstract, 55 studies underwent full-text screening, yielding 13 studies for review. The health interventions identified were classified into three levels of management. The macro level included the use of epidemiological models, renewable energy, and policies sensitive to climate change. The meso level comprised interventions such as the creation of environmental suitability maps, urban greening, chemoprophylaxis, water security plans, and sanitation projects, among other measures. Some interventions are at the intersection, such as educational campaigns and the modification of artificial larvae sites. Finally, the micro level contained interventions such as the inspection of window screens and the use of light-colored clothing and repellents. The health interventions at the macro, meso, and micro levels and the intersection may serve as a basis for public managers to implement appropriate interventions against climate-sensitive diseases.


Similar content being viewed by others
References
World Health Organization. Quantitative risk assessment of the effects of climate change on selected causes of death, 2030s and 2050s. Published 2014. https://apps.who.int/iris/bitstream/handle/10665/134014/9789241507691_eng.pdf. Accessed November 10 2021.
Pan American Health Organization. Agenda for the Americas on health, environment, and climate change 2021–2030. Published 2021. https://iris.paho.org/bitstream/handle/10665.2/54816/PAHOCDECE210004_eng.pdf?sequence=9&isAllowed=y. Accessed November 10 2021.
Callaghan M, Schleussner CF, Nath S, et al. Machine-learning-based evidence and attribution mapping of 100,000 climate impact studies. Nature climate change. 2021;11(11). https://doi.org/10.1038/s41558-021-01168-6.
Ogden NH. Climate change and vector-borne diseases of public health significance. FEMS microbiology letters. 2017;364(19). https://doi.org/10.1093/femsle/fnx186.
World Health Organization. International classification of health interventions — ICHI Beta 2017. Published 2017. https://mitel.dimi.uniud.it/ichi/. Accessed November 10 2021.
Vos T, Allen C, Arora M, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. The Lancet. 2016;388(10053). https://doi.org/10.1016/S0140-6736(16)31678-6
Brazilian Ministry of Health. Doenças infecciosas e parasitárias: guia de bolso [Infectious and parasitic diseases: pocket guide]. Published 2010. https://bvsms.saude.gov.br/bvs/publicacoes/doencas_infecciosas_parasitaria_guia_bolso.pdf. Accessed November 10 2021.
Sousa TCM, Amancio F, Hacon S de S, Barcellos C. Doenças sensíveis ao clima no Brasil e no mundo: revisão sistemática. Revista Panamericana de Salud Pública. 2018;42. https://doi.org/10.26633/RPSP.2018.85.
Ajumobi O, Uhomoibhi P, Onyiah P, et al. Setting a Nigeria national malaria operational research agenda: the process. BMC Health Serv Res. 2018;18(1). https://doi.org/10.1186/s12913-018-3224-5.
Chen K, Breitner S, Wolf K, et al. Projection of temperature-related myocardial infarction in Augsburg, Germany: moving on from the Paris Agreement on climate change. Deutsches Ärzteblatt International. 2019;116. https://doi.org/10.3238/arztebl.2019.0521
Park S, Kario K, Chia YC, et al. On behalf of the HOPE Asia Network. The influence of the ambient temperature on blood pressure and how it will affect the epidemiology of hypertension in Asia. J Clin Hypertens. 2020;22. https://doi.org/10.1111/jch.13762
Watts N, Amann M, Arnell N, et al. The report of The Lancet Countdown on health and climate change: ensuring that the health of a child born today is not defined by a changing climate. Lancet. 2019;2019:394. https://doi.org/10.1016/S0140-6736(19)32596-6.
Chua PL, Dorotan MM, Sigua JA, Estanislao RD, Hashizume M, Salazar MA. Scoping review of climate change and health research in the Philippines: a complementary tool in research agenda-setting. Int J Environ Res Publ Health. 2019;16(14). https://doi.org/10.3390/ijerph16142624.
Herlihy N, Bar-Hen A, Verner G, et al. Climate change and human health: what are the research trends? A scoping review protocol. BMJ Open. 2016;6(12). https://doi.org/10.1136/bmjopen-2016-012022.
Lenzen MJ, Reimer WJMS, Boersma E, et al. Differences between patients with a preserved and a depressed left ventricular function: a report from the EuroHeart Failure Survey. Eur Heart J. 2004;25(14). https://doi.org/10.1016/j.ehj.2004.06.006.
Hathaway J, Maibach EW. Health implications of climate change: a review of the literature about the perception of the public and health professionals. Curr Environ Health Rep. 2018;5(1). https://doi.org/10.1007/s40572-018-0190-3.
Humboldt-Dachroeden S, Rubin O, Sylvester Frid-Nielsen S. The state of One Health research across disciplines and sectors – a bibliometric analysis. One Health. 2020;10. https://doi.org/10.1016/j.onehlt.2020.100146
Gilson L. Health policy and systems research: a methodology reader. Geneva, Switzerland: World Health Organization. Published 2012. https://apps.who.int/iris/handle/10665/44803. Accessed April 12 2022.
Aromataris E, Munn Z. JBI manual for evidence synthesis. (Aromataris E, Munn Z, eds.). JBI. 2020. https://doi.org/10.46658/JBIMES-20-01
Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7). https://doi.org/10.7326/M18-0850
Muñoz ÁG, Chourio X, Rivière-Cinnamond A, et al. AeDES: a next-generation monitoring and forecasting system for environmental suitability of Aedes-borne disease transmission. Sci Rep. 2020;10(1). https://doi.org/10.1038/s41598-020-69625-4
Withanage GP, Viswakula SD, Nilmini Silva Gunawardena YI, Hapugoda MD. A forecasting model for dengue incidence in the District of Gampaha, Sri Lanka. Parasites & vectors. 2018;11(1). https://doi.org/10.1186/s13071-018-2828-2
Zaki R, Roffeei SN, Hii YL, et al. Public perception and attitude towards dengue prevention activity and response to dengue early warning in Malaysia. Plos One. 2019;14(2). https://doi.org/10.1371/journal.pone.0212497
Ebi KL, Kovats RS, Menne B. An approach for assessing human health vulnerability and public health interventions to adapt to climate change. Environ Health Perspect. 2006;114(12). https://doi.org/10.1289/ehp.8430
Confalonieri UE, Menezes JA, Souza CM. Climate change and adaptation of the health sector: the case of infectious diseases. Virulence. 2015;6(6). https://doi.org/10.1080/21505594.2015.1023985
Rother HA. Controlling and preventing climate-sensitive noncommunicable diseases in urban Sub-Saharan Africa. Sci Total Environ. 2020;722. https://doi.org/10.1016/j.scitotenv.2020.137772
Bouzid M, Hooper L, Hunter PR. The effectiveness of public health interventions to reduce the health impact of climate change: a systematic review of systematic reviews. Plos One. 2013;8(4). https://doi.org/10.1371/journal.pone.0062041
Schwerdtle PN, Irvine E, Brockington S, Devine C, Guevara M, Bowen KJ. Calibrating to scale: a framework for humanitarian health organizations to anticipate, prevent, prepare for and manage climate-related health risks. Glob Health. 2020;16(1). https://doi.org/10.1186/s12992-020-00582-3
Bouzid M, Brainard J, Hooper L, Hunter PR. Public health interventions for Aedes control in the time of Zikavirus – a meta-review on effectiveness of vector control strategies. PloS Negl Trop Dis. 2016;10(12). https://doi.org/10.1371/journal.pntd.0005176
Polk LV, Green PM. Contamination: nursing diagnoses with outcome and intervention linkages. Int J Nurs Terminol Classif. 2007;18(2). https://doi.org/10.1111/j.1744-618X.2007.00048.x
Hongoh V, Campagna C, Panic M, et al. Assessing interventions to manage West Nile Virus using multi-criteria decision analysis with risk scenarios. Plos One. 2016;11(8). https://doi.org/10.1371/journal.pone.0160651
Kabir MI, Rahman MB, Smith W, Lusha MAF, Milton AH. Child centred approach to climate change and health adaptation through schools in Bangladesh: a cluster randomised intervention trial. Plos One. 2015;10(8). https://doi.org/10.1371/journal.pone.0134993
Reisen W, Brault AC. West Nile virus in North America: perspectives on epidemiology and intervention. Pest Manag Sci. 2007;63(7). https://doi.org/10.1002/ps.1325
Jagals P, Ebi K. Core competencies for health workers to deal with climate and environmental change. Int J Environ Res Publ Health. 2021;18(8). https://doi.org/10.3390/ijerph18083849
Sales DM, Assis WL, Fonseca BM. Clima urbano e saúde: elementos climáticos e doenças respiratórias observadas no município de Belo Horizonte (MG) entre 2013 e 2014 [Urban climate and health: climatic elements and respiratory diseases observed in the city of Belo Horizonte (MG) between 2013 and 2014]. Revista Brasileira de Climatologia. 2018;1. https://doi.org/10.5380/abclima.v1i0.61035
Hansen A, Xiang J, Liu Q, et al. Experts’ perceptions on China’s capacity to manage emerging and re-emerging zoonotic diseases in an era of climate change. Zoonoses and Publ Health. 2017;64(7). https://doi.org/10.1111/zph.12335
Intergovernmental Panel on Climate Change. Global warming of 1.5°C: an IPCC special report on the impacts of global warming of 1.5°C above pre-industrial levels and related global greenhouse gas emission pathways, in the context of strengthening the global response to the threat of climate change, sustainable development, and efforts to eradicate poverty. Published 2018. https://www.ipcc.ch/sr15/download/#full. Accessed March 8 2022.
Hambling T, Weinstein P, Slaney D. A review of frameworks for developing environmental health indicators for climate change and health. Int J Environ Res Publ Health. 2011;8(7). https://doi.org/10.3390/ijerph8072854
Nissan H, Ukawuba I, Thomson M. Climate-proofing a malaria eradication strategy. Malar J. 2021;20(1). https://doi.org/10.1186/s12936-021-03718-x
Andrade NF de, Prado EA de J, Albarado ÁJ, Sousa MF de, Mendonça AVM. Analysis of the prevention campaigns against dengue, zika and chikungunya arboviruses from the Ministry of Health from the health education and communication perspective. Saúde em Debate>. 2020;44(126). https://doi.org/10.1590/0103-1104202012621
Campbell-Lendrum DH, Corvalan CF, Prüss UA. How much disease could climate change cause. In: McMichael AJ, Campbell-Lendrum DH, Corvalan CF, Ebi KL, Githeko AK, Scheraga JD, Woodward A, editors. Climate change and human health: risks and responses. Geneva: World Health Organization; 2003. p. 133–58.
Shaman J, Knowlton K. The need for climate and health education. Am J Public Health. 2018;108(S2). https://doi.org/10.2105/AJPH.2017.304045
Acknowledgements
This study was supported by the Brazilian National Research Council (CNPq, Brazil, ordinance no. 402514/2021-1), and by the CAPES Foundation (Ministry of Education of Brazil, ordinance no. 216/2018).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Moreira, R.P., de Oliveira, F.B.B., de Araujo, T.L. et al. Health Interventions for Preventing Climate-Sensitive Diseases: Scoping Review. J Urban Health 99, 519–532 (2022). https://doi.org/10.1007/s11524-022-00631-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-022-00631-9