Abstract
The obesity rate in Chicago has increased up to more than 30% in the last two decades. Obesity is a major problem in Chicago, where 36% of the city’s high school students and 61% of adults in the metropolitan area are overweight or obese. Simultaneously, Chicago remains highly segregated by race—a phenomenon that begs for spatial analysis of health. Extant work exploring associations between the food retail environment and obesity has provided mixed findings, and virtually, none of this work has been done with the effects of the interaction between racial segregation and the food retail environment on obesity, where obesity rates are among the highest in the segregation area for the city defined by racial segregation. This study explores whether being overweight or obese is associated with urban food environments, such as access to different types of food retail outlets, and how its associations interact with racial factors, at the community level. This study uses the 2016–2018 data from the Healthy Chicago Survey to investigate the spatial variations in obesity and their association with food environments in Chicago. Also, this study examines the moderating effects of racial segregation on associations between obesity and access to food retail outlets. Using spatial statistics and regression models with interaction terms, this study assesses how the urban food environment can interact with racial segregation to explain the spatial distribution of obesity. The results indicate that the obesity population is highly concentrated in the African American community. In Chicago, each additional convenience store in a community is associated with a 0.42% increase in the obesity rate. Fast food restaurant access is predictive of a greater obesity rate, and grocery store access is predictive of less obesity rate in a community with a higher percentage of African American population. Findings can be used to promote equitable access to food retail outlets, which may help reduce broader health inequities in Chicago.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
According to the US Department of Health and Human Services and the National Institutes of Health, obesity and overweight as the second leading cause of preventable death cause an estimated 300,000 annual deaths in the USA [1]. The high prevalence of obesity in the USA has been well documented in the literature since the obese population is of great concern for being at an increased risk for several acute and chronic diseases, such as diabetes, cardiovascular diseases, and coronavirus diseases [2,3,4,5,6,7,8].
Among the built environmental factors of obesity, researchers have paid much attention to the food environment [9,10,11,12,13,14,15]. The literature has examined the associations between the food environment and overweight and obesity. Studies provide evidence of a positive effect of supermarket availability and a negative effect of fast food availability on obesity. Xu et al. found that residents in a county with a stronger fast food presence are linked to higher odds of overweight and obesity in Utah [10]. Morland et al. found that the existence of grocery stores, convenience stores, or fast food restaurants was associated with a higher prevalence of obesity while the presence of supermarkets was associated with a lower prevalence of obesity at the census tract level [11, 12]. A similar finding was reported in a study in New Orleans where each additional supermarket in a neighborhood was predictive of lower obesity odds, and convenience store and fast food restaurant access were associated with an increased odds for obesity [13]. However, Mejia et al. and Huang et al. found opposite effects of grocery stores and convenience stores on obesity. Mejia et al. found that more convenience stores in a walkable distance of 400 m were associated with lower body mass index (BMI) among adults in Los Angeles County [14]. Dubowitz et al. found that an increase in grocery stores and supermarket outlet availability lowers BMI for women aged 50–79 years [15]. Positive effects of supermarket existence and negative effects of fast food presence have been consistently observed in a large number of studies [10, 11, 13], but the mixed and inconsistent findings are most common in assessing associations between obesity and access to grocery stores and convenience stores [11,12,13,14,15]. The majority of the literature has not shown a relationship between them [13, 16], while the remaining studies have shown the opposite effects of grocery stores or convenience stores on obesity [11, 12, 14, 15]. Besides, it is believed that moderating factors are needed to better understand the disparities in the prevalence of obesity in the USA and their associations with food environments [17]. Race is an important moderating factor contributing to the variation of obesity and its associations with food environments since African American communities with different access to food environments are found to have a higher prevalence of obesity [18, 19]. However, few studies have examined how food environment access interacts with the race of residents to affect obesity; further research is warranted.
The obesity rate in Chicago has increased up to more than 30% in the last two decades [20, 21]. Obesity is a major concern in Chicago, where 36% of the high school students in the city and 61% of adults in the metropolitan area are overweight or obese [22]. Simultaneously, Chicago remains highly segregated by race—a phenomenon that begs for spatial analysis of health. Extant work exploring the associations between the food retail environment and obesity has provided mixed findings, and virtually, none of this work has been done with the effects of the interaction between racial segregation and the food retail environment on obesity, where obesity rates are among the highest in the segregation area for a city defined by racial segregation. Research for moderating effects of racial segregation and food environments on obesity is needed. The city of Chicago has significant racial disparities in food access [23, 24], and the African American residents are facing challenges of racial segregation. Because of these conditions, Chicago was an especially appropriate setting for investigating the moderating effects of racial segregation and food environments on obesity.
To fill the gap, this study uses spatial statistics to examine the spatial distribution of obesity and its association with racial segregation. Also, this study develops regression models with interaction terms to assess how urban food environments interact with racial segregation to affect obesity. It is hypothesized that the number of supermarkets and grocery access would be negatively associated with a prevalence of obesity while the number of convenience stores and fast food restaurants would be positively associated with a prevalence of obesity. It is also hypothesized that racial composition is a moderator of the relationship between obesity and access to different types of food retail outlets.
Methods
Study Sample
Respondents’ sample data are from the Healthy Chicago Survey collected by the Chicago Department of Public Health between 2016 and 2018. The Healthy Chicago Survey is an annual telephone survey launched in 2014 by the Chicago Department of Public Health to better understand the health of Chicagoans, which collects information on chronic health conditions including obesity data [25]. A random-digit-dial method was used in this survey—an adult aged 18 years or older in each household was randomly selected to be interviewed. Body mass index (BMI) was calculated for adults aged 18 years or older who reported height and weight. Individuals with a BMI of 30 or greater are obese. The adult obesity rate in a community is the estimated number of adults aged 18 years or older who are obese divided by the estimated number of adults in a community, expressed as a percent, which is weighted to represent the population from which the sample was drawn, the household population of adults aged 18 years or older in the city of Chicago [26]. The survey sample size is 662,000, accounting for about 25% of the total population in Chicago. [52]
Food Store Database and Neighborhood Food Environment
Data on food stores are from the Dun & Bradstreet database. The food outlets’ information in this database includes each retailer’s location, annual sales, and the industry code under the North American Industry Classification System (NAICS) [27]. This study uses NAICS codes to identify each type of food store outlet. Retailers are classified into four types of food outlets according to NAICS codes and sales: supermarkets (code: 445110), grocery stores (code: 445110), convenience stores (code: 445120), and fast food restaurants (code: 722513). Supermarkets and grocery stores have the same industry code—both are primarily engaged in retailing a general line of food, so this study distinguishes supermarkets from grocery stores based on sales: stores with the industry code 445110 and annual sales greater than or equal to 1 million dollars are defined as supermarkets while stores with the same industry code and annual sales less than 1 million dollars are defined as grocery stores.
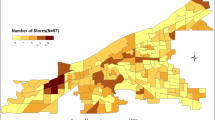
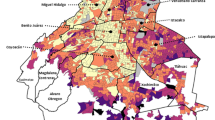
Chicago is 607 sq. km.in size [28], consisting of 77 community areas. This study uses a community buffer boundary to define the extent of a neighborhood food environment. To resolve the boundary problem, half a mile external buffer outside the boundary of each community was constructed to account for stores since half a mile is a reachable distance for an average person’s 10-min walking. Based on the spatial distribution of the number of food stores shown in Fig. 1 and the spatial distribution of the number of food stores per capita shown in Fig. 2, the North Side of Chicago has the highest store concentration while the South Side of Chicago has the highest store per capita concentration. The number of each type of food stores per capita is used to consider spatial heterogeneous populations within the city since more population lives in the North Side than the South Side and the North Side has a much higher population density than the South Side, so each type of food store access is measured by the number of each type of food store and the number of each type of food store per capita within a community buffer boundary.
Independent Variables
The community socio-demographic data and travel behavior data are extracted from the 2014–2018 American Community Survey and the Chicago Metropolitan Agency for Planning (CMAP) [29, 30]. These socio-demographic data include race, gender, age, income, educational attainment, and household size. The travel behavior data include the mode of travel to work and annual vehicle miles traveled per household. Since both the African American population and Latino population have a higher prevalence of obesity than other racial populations [13, 17], two race variables are the African American percentage of the population and the Latino percentage of the population, respectively, for a community. The female population has a higher obesity prevalence than the male population [13, 17, 31], so the gender variable measures the female percent of the total population in a community. Age was grouped into five categories: under 19, 20–34, 35–49, 50–64, and 65 and older. The youngest age cohort is a reference group. Education includes six levels: less than high school, high school graduate, some college, associate degree, bachelor’s degree, and graduate or professional degree. Less than high school is a reference group. Besides household median income, annual household income is grouped into six classes: less than $25,000, $25,000 to $49,999, $50,000 to $74,999, $75,000 to $99,999, $100,000 to $149,999, and $150,000 and over. Less than $25,000 is a reference group. There are four types of household size: 1-person household, 2-person household, 3-person household, 4-or-more person household. A 4-or-more person household is a reference group. There are five modes of work travel: work at home, drive alone, carpool, transit, walk or bike, and others. The mode “walk or bike” is a reference group. There are four means of transportation to work by vehicles available: no vehicle available, one vehicle available, two vehicles available, and three or more vehicles available. No vehicle available is a reference group. Total park acres data measuring the built environment are from the CMAP 2013 land use inventory [30].
Statistical Analysis and Regression Modeling with Interaction Term
Spatial statistics, local Getis-Ord G, are used to identify local clusters of hotspots and coldspots of obesity. ArcGIS is used to perform and visualize the results of local spatial statistics. This study also uses ordinary least squares regression models to assess the effects of food store access on obesity prevalence. To investigate the moderating effects of racial segregation and food store access on obesity, the interaction terms between each type of food store access and the African American percent are added to the analysis model. This study develops regression models with interaction terms to assess how urban food environments interact with racial segregation to affect obesity. The backward method is used to filter variables to include only statistically significant ones.
Results
As shown in Table 1, the overall obesity prevalence of the sample is 31%. The largest racial group of the sample is African American, accounting for 37% of the sample participants. Figure 3 shows the obesity hotspots and coldspots and the African American percent distribution. As shown in Fig. 3, obesity hotspots are the African American communities. The obesity population is highly concentrated in the African American community. Besides, most of the participants are female. More than 65% of the respondents are aged between 30 and 64. Twenty-three percent of the respondents live at or below the poverty line. Those with higher obesity rates include African Americans, females, and middle-aged respondents. Individuals at or below the poverty line have higher rates as well.
Table 2 shows the descriptive statistics on the food retail environment. Households have many more grocery stores and fast food restaurants in their communities than supermarkets and convenience stores. Figure 1 shows the number of each type of food store by the community. Twenty-eight out of 77 communities are African American communities, accounting for 29% of the total population in Chicago [42]. African American communities’ access to each type of food store is below the average among communities. The mean number of supermarkets in a community is 4.27. Five communities have no access to supermarkets, and 1 out of these communities is African American communities. Fifty-two communities have access to one to four supermarkets, below the average, and 25 out of these communities are African American communities. The mean number of grocery stores is 71. Forty-five communities have access to less than or equal to 71 grocery stores, below the average, and 40% of them are African American communities, which are higher than African American population percent. Similarly, the percentage of African American communities with access to the number of convenience stores below the average is 46%, and the percentage of African American communities with access to the number of fast food restaurants below the average is 51%—both are higher than African American population percentages.
Table 3 depicts the relationship between the food retailer access variables and obesity prevalence. Model results indicate that more convenience stores are significantly associated with higher obesity prevalence while more convenience stores per capita are significantly associated with lower obesity prevalence. Each additional convenience store in a community is associated with a 0.42% increase in the obesity rate. The number of convenience stores and the number of convenience stores per capita have opposite associations with obesity prevalence in that the North Side of Chicago has the highest store concentration while the South Side of Chicago has the highest store per capita concentration. High concentrations of convenience stores in the North Side of Chicago cause surplus access to less healthy foods in the North Side because convenience stores provide greater spatial access than traditional food stores, such as supermarkets and grocery stores. [50, 51] Comparatively, high concentrations of convenience stores per capita in the South Side of Chicago show that access to healthy food matters because convenience stores are the key food environment influence on nutrients available, representing healthy foods availability in household food supplies among limited resource residents. [36] Also, according to the model coefficients, the magnitude of association of convenience stores with obesity is 2-fold higher than grocery stores, which indicates the greater influence of convenience stores on obesity than grocery stores. This further confirms the key role of convenience stores in the food environment among limited resource residents. And the magnitude of the difference in convenience stores and grocery stores is consistent with the results in Dubowitz et al. that the effect size for the availability of different types of food stores are different. [15]
The interaction terms between food store access and African American population indicate that more grocery stores are significantly associated with lower obesity prevalence when African American population percent increases. The interaction terms also indicate that more fast food restaurants are significantly associated with higher obesity prevalence when African American population percent increases. In the model, other socio-demographic factors associated with obesity prevalence are age and educational attainment. The elderly population is associated with a higher obesity rate while the population with bachelor’s degrees is associated with a lower obesity rate.
Besides, built environment and travel behavioral factors reflecting lifestyle options influence obesity prevalence. Regarding the built environment, more total park acres are associated with a lower obesity rate. This implies the significance of parks in lowering the obesity rate since people access to parks for physical fitness activities. An active lifestyle may be curbing this public health epidemic by encouraging physical activity in parks with recreational facilities since it is found that there is a consistent correlation between convenient access to recreational facilities and physical activity [43, 44]. Besides, compared to walk or bike mode, the modes of working at home, drove alone, carpool, and transit are associated with a higher obesity rate. Among these modes, working at home is associated with the highest obesity rate. The findings provide evidence of the link between adult obesity levels and travel behavior, which is consistent with what Gordon-Larsen et al. and Bassett et al. found that active travel, i.e., walking and cycling, could lower obesity rates by increasing levels of physical activity [45, 46]. Also, the association of working at home with the highest obesity rate echoes Kipke et al.’s finding that a sedentary lifestyle may be fueling the obesity epidemic [47]. Besides, households with two vehicles are associated with a higher obesity rate while households with three or more vehicles are associated with a lower obesity rate, compared to households without vehicles. The results indicate that heavy dependence on passive forms of transportation could explain greater inactivity leading to an increase in the prevalence of obesity. Bell et al. found motorized forms of transportation promoting obesity in China. Comparatively, the USA has less variation in the type of transportation among the population since 82% of trips are vehicle trips and vehicle ownership is close to 90% [48, 49]. Thus, households with one vehicle are not significantly associated with a lower obesity rate. However, two vehicles in a household could create increasingly sedentary time by driving more trips. So, it could be an effective obesity prevention strategy to discourage heavy dependence on vehicle uses.
Discussion
Obesity in Chicago demonstrated a North-South gradient: the North Side is the least obese, the least African American population, and the greatest food store access while the South Side is the most obese, the most African American population, and the least food store access. A similar obesity gradient is found in Seattle, which is segregated by income and education [32]. By contrast, the Chicago North-South obesity gradient is consistent with racial segregation, so regarding the influence of the community-built environment, the cross-level interactions of the race with each type of food store access are emphasized in Chicago.
This research found the opposite associations of convenience stores with obesity—more convenience stores are associated with a higher prevalence of obesity while more convenience stores per capita are associated with a lower prevalence of obesity. The findings provide evidence on the spatial variation of correlations between certain types of food retailer access and obesity prevalence. The evidence demonstrates that access to healthy food matters in the South Side of Chicago due to the absence of healthy foods while reductions of access to less healthy food matter in the North Side of Chicago due to the glut of less healthy foods. These findings are consistent with the results in the existing literature that convenience stores are the key food environment influence on healthy foods availability in household food supplies among limited-resource communities. [36, 50]
What is distinctive about this research is that race is identified as a moderator of the relation of food environments to obesity. Race has been found to moderate the relationship between changes in food environment access and BMI. The findings suggest that African American communities have different food environments and may result in their different behavioral responses to the food environments and exposures to different types of food stores. For example, it is found that in African American communities, fast food restaurant access and grocery store access are directly associated with obesity in opposite directions, which is expected as numerous studies have found [10, 11, 13]. But it is found for convenience stores in African American communities—greater access is associated with a lower obesity prevalence, which might appear to be counter-intuitive because both convenience stores and fast food restaurants offer energy-dense foods [33, 34]. However, different from fast food restaurants, convenience stores not only offer mostly prepared, highly processed, high-calorie foods, but also a limited choice of fresh produce [35]. Thus, convenience stores are relatively healthy compared to fast food restaurants. Further, due to the African American communities’ lack of access to healthy supermarkets and grocery stores in Chicago, convenience stores are easier to access than supermarkets and grocery stores in African American communities. This echoes Sharkey et al.’s findings that community and neighborhood retail food venues, such as convenience stores, are a frequent source of food items and might have a greater influence on household food supplies than supermarkets and groceries, especially for the minority population [36,37,38,39]. Besides, each type of food store might have diverse food quality and prices [40]. Le et al. provides evidence that children with access to higher quality food items, no matter what type of food store, had lower odds of obesity [41].
This study has some limitations. First, BMI is calculated from self-reported data, so it is unclear whether there is any systematic bias related to store access predictors. Second, its cross-sectional nature does not allow for examining any causal effects between obesity and the food environment. Third, spatial analyses at the aggregate level, community level, potentially have a boundary problem. The selection of the aggregation level is data-driven and needs to be tested. Fourth, obesity disparity might be attributable to unobserved neighborhood characteristics, such as crime and street design since these neighborhood features might affect the physical activity levels of respondents. This study controls for travel mode, but neighborhood walkability features are not included in the model due to the unavailability of data. Lastly, categorizing food outlets by the NAICS code is a crude way to classify complex consumer behavior, assuming that healthy food at affordable prices is available on the basis simply of the availability of broadly classified food stores, which could lead to misleading results [41]. Different dimensions of the food environment, including availability, price, and quality of foods, need to be examined for future research.
This study aims to provide answers to the following questions: What characteristics of the neighborhood food environment are associated with obesity in Chicago? Do African Americans have greater (or lesser) access to different types of food retailers? Convenience stores have opposite effects on obesity in Chicago: more convenience stores per capita are associated with lower obesity prevalence in the South Side while more convenience stores are associated with higher obesity prevalence in the North Side. Most importantly, African American communities have lesser access to all types of food retailers. The obesity prevalence in African American communities is positively associated with fast food restaurants but negatively associated with grocery stores. Interventions to provide more healthy options in grocery stores and convenience stores in African American neighborhoods may have favorable effects on African Americans’ weight outcomes. At the same time, interventions to reduce less healthy options in convenience stores in non-African American neighborhoods might help reduce obesity among non-African American communities.
References
U.S. Department of Health and Human Services. Overweight and obesity: a major public health issue. Prevention Report. 2001:16.
Morrill AC, Chinn CD. The obesity epidemic in the United States. J Public Health Policy. 2004;25(3/4):353–66.
Ogden CL, Yanovski SZ, Carroll MD, Flegal KM. The epidemiology of obesity. Gastroenterology. 2007;132(6):2087–102.
Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev. 2007;29(1):6–28.
Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295(13):1549–55.
Thompson D, Edelsberg J, Colditz GA, Bird AP, Oster G. Lifetime health and economic consequences of obesity. Arch Intern Med. 1999;159(18):2177–83.
Simonnet A, Chetboun M, Poissy J, Raverdy V, Noulette J, Duhamel A, et al. High prevalence of obesity in severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) requiring invasive mechanical ventilation. Obesity. 2020;28(7):1195–9. https://doi.org/10.1002/oby.22831.
Kalligeros M, Shehadeh F, Mylona EK, Benitez G, Beckwith CG, Chan PA, et al. Association of obesity with disease severity among patients with coronavirus disease 2019. Obesity. 2020;28(7):1200–4.
Michimi A, Wimberly MC. Associations of supermarket accessibility with obesity and fruit and vegetable consumption in the conterminous United States. Int J Health Geogr. 2010;9(1):49. https://doi.org/10.1186/1476-072X-9-49.
Xu Y, Wen M, Wang F. Multilevel built environment features and individual odds of overweight and obesity in Utah. Appl Geogr. 2015;60:197–203.
Morland KB, Evenson KR. Obesity prevalence and the local food environment. Health Place. 2009;15(2):491–5. https://doi.org/10.1016/j.healthplace.2008.09.004.
Morland K, Diez Roux AV, Wing S. Supermarkets, other food stores, and obesity: the atherosclerosis risk in communities study. Am J Prev Med. 2006;30(4):333–9.
Bodor JN, Rice JC, Farley TA, Swalm CM, Rose D. The association between obesity and urban food environments. J Urban Health. 2010;87(5):771–81. https://doi.org/10.1007/s11524-010-9460-6.
Mejia N, Lightstone AS, Basurto-Davila R, Morales DM, Sturm R. Neighborhood food environment, diet, and obesity among Los Angeles County adults, 2011. Prev Chronic Dis. 2015;12 https://doi.org/10.5888/pcd12.150078.
Dubowitz T, Ghosh-Dastidar M, Eibner C, Slaughter ME, Fernandes M, Whitsel EA, et al. The Women’s Health Initiative: the food environment, neighborhood socioeconomic status, BMI, and blood pressure. Obesity. 2012;20(4):862–71.
Cobb LK, Appel LJ, Franco M, Jones-Smith JC, Nur A, Anderson CA. The relationship of the local food environment with obesity: a systematic review of methods, study quality, and results. Obesity. 2015;23(7):1331–44.
Oka M, Link CL, Kawachi I. Area-based variations in obesity are more than a function of the food and physical activity environment: area-based variations in obesity. J Urban Health. 2013;90(3):442–63. https://doi.org/10.1007/s11524-012-9715-5.
Powell LM, Chaloupka FJ, Bao Y. The availability of fast-food and full-service restaurants in the United States: associations with neighborhood characteristics. Am J Prev Med. 2007;33(4, Supplement):S240–5. https://doi.org/10.1016/j.amepre.2007.07.005.
Jones-Smith JC, Karter AJ, Warton EM, Kelly M, Kersten E, Moffet HH, et al. Obesity and the food environment: income and ethnicity differences among people with diabetes: the Diabetes Study of Northern California (DISTANCE). Diabetes Care. 2013;36(9):2697–705. https://doi.org/10.2337/dc12-2190.
Illinois Department of Public Health, Behavioral Risk Factor Surveillance System, 2000–2009
Chicago Department of Public Health, Healthy Chicago Survey, 2014–2018
Centers for Disease Control and Prevention, Community Profile: Chicago, Illinois. Accessed May 12, 2021. https://www.cdc.gov/nccdphp/dch/programs/communitiesputtingpreventiontowork/communities/profiles/both-il_chicago.htm
Kolak M, Bradley M, Block DR, Pool L, Garg G, Toman CK, et al. Urban foodscape trends: disparities in healthy food access in Chicago, 2007–2014. Health Place. 2018;52:231–9. https://doi.org/10.1016/j.healthplace.2018.06.003.
Kwate NOA, Loh JM. Fast food and liquor store density, co-tenancy, and turnover: vice store operations in Chicago, 1995–2008. Appl Geogr. 2016;67:1–13.
Chicago Department of Public Health, Healthy Chicago Survey. Accessed May 12, 2021. https://www.chicago.gov/city/en/depts/cdph/supp_info/healthy-communities/healthy-chicago-survey.html
Chicago Health Atlas, Adult Obesity. Accessed May 12, 2021. https://www.chicagohealthatlas.org/indicators/adult-obesity Accessed September 2020
U.S. Census Bureau, North American Industry Classification System. Accessed May 12, 2021. https://www.census.gov/naics/
U.S. Census Bureau, 2019 Gazetteer File. Accessed May 12, 2021 https://www.census.gov/geographies/reference-files/time-series/geo/gazetteer-files.2019.html
U.S. Census Bureau, Explore Census Data. Accessed May 12, 2021. https://data.census.gov/cedsci/
The Chicago Metropolitan Agency for Planning (CMAP), Accessed May 12, 2021. The CMAP Data Hub. https://datahub.cmap.illinois.gov/
Strauss RS, Knight J. Influence of the home environment on the development of obesity in children. Pediatrics. 1999;103(6):e85. https://doi.org/10.1542/peds.103.6.e85.
Huang R, Moudon AV, Cook AJ, Drewnowski A. The spatial clustering of obesity: does the built environment matter? J Hum Nutr Diet. 2015;28(6):604–12. https://doi.org/10.1111/jhn.12279.
Farley TA, Rice J, Bodor JN, Cohen DA, Bluthenthal RN, Rose D. Measuring the food environment: shelf space of fruits, vegetables, and snack foods in stores. J Urban Health. 2009;86(5):672–82.
Glanz K, Sallis JF, Saelens BE, Frank LD. Nutrition Environment Measures Survey in stores (NEMS-S): development and evaluation. Am J Prev Med. 2007;32(4):282–9.
Horowitz CR, Colson KA, Hebert PL, Lancaster K. Barriers to buying healthy foods for people with diabetes: evidence of environmental disparities. Am J Public Health. 2004;94(9):1549–54. https://doi.org/10.2105/AJPH.94.9.1549.
Sharkey JR, Dean WR, Nalty CC, Xu J. Convenience stores are the key food environment influence on nutrients available from household food supplies in Texas Border Colonias. BMC Public Health. 2013;13(1):45.
French SA, Shimotsu ST, Wall M, Gerlach AF. Capturing the spectrum of household food and beverage purchasing behavior: a review. J Am Diet Assoc. 2008;108:2051–8.
Sobal J, Bisogni CA. Constructing food choice decisions. Ann Behav Med. 2009;38(suppl_1):s37–46. https://doi.org/10.1007/s12160-009-9124-5.
Langellier BA. The food environment and student weight status, Los Angeles County, 2008-2009. Prev Chronic Dis. 2012;9:110191. https://doi.org/10.5888/pcd9.110191.
Griffiths C, Frearson A, Taylor A, Radley D, Cooke C. A cross sectional study investigating the association between exposure to food outlets and childhood obesity in Leeds, UK. Int J Behav Nutr Phys Act. 2014;11(1):138. https://doi.org/10.1186/s12966-014-0138-4.
Le H, Engler-Stringer R, Muhajarine N. Walkable home neighborhood food environment and children’s overweight and obesity: proximity, density or price. Can J Public Health. 2016;107(S1):42–7.
U.S. Census Bureau, American Community Survey. Accessed May 12, 2021. https://www.census.gov/programs-surveys/acs/
Sallis JF, Bauman A, Pratt M. Environmental and policy interventions to promote physical activity. Am J Prev Med. 1998;15(4):379–97.
Humpel N, Owen N, Leslie E. Environmental factors associated with adults’ participation in physical activity: a review. Am J Prev Med. 2002;22(3):188–99.
Gordon-Larsen P, Boone-Heinonen J, Sidney S, Sternfeld B, Jacobs DR Jr, Lewis CE. Active commuting and cardiovascular disease risk: the CARDIA Study. Arch Intern Med. 2009;169(13):1216–23. https://doi.org/10.1001/archinternmed.2009.163.
Bassett DR, Pucher J, Buehler R, Thompson DL, Crouter SE. Walking, cycling, and obesity rates in Europe, North America, and Australia. J Phys Act Health. 2008;5(6):795–814. https://doi.org/10.1123/jpah.5.6.795.
Kipke MD, Iverson E, Moore D, Booker C, Ruelas V, Peters AL, et al. Food and park environments: neighborhood-level risks for childhood obesity in East Los Angeles. J Adolesc Health. 2007;40(4):325–33.
F.H.W.A. (Federal Highway Administration). 2010 status of the nation’s highways, bridges, and transit: conditions & performance. In: Rep. to Congress. ; 2010. Accessed May 12, 2021. https://www.fhwa.dot.gov/policy/2010cpr/
Bureau of Transportation Statistics, US Department of Transportation. Household, Individual, and Vehicle Characteristics. Accessed May 12, 2021. https://www.bts.gov/archive/publications/highlights_of_the_2001_national_household_travel_survey/section_01
Sharkey HJR, S H, D H, J. C. Association between neighborhood need and spatial access to food stores and fast food restaurants in neighborhoods of Colonias. Int J Health Geogr. 2009;8(9)
Sharkey J, Horel S. Neighborhood socioeconomic deprivation and minority composition are associated with better potential spatial access to the food environment in a large rural area. J Nutr. 2008;138:620–7.
U.S. Census Bureau, QuickFacts: Chicago City, Illinois; United States. Accessed May 12, 2021. https://www.census.gov/quickfacts/fact/table/chicagocityillinois,US/PST045219
Acknowledgements
The author would like to acknowledge a grant from the Calamos Fund of the Lewis College of Science and Letters at the Illinois Institute of Technology. The author is grateful for the constructive comments from anonymous referees and the journal editor. The author is also grateful forthe helpful inputs of Dr. Steve N. Du Bois and Dr. Arlen Moller, and the excellent research assistance of Siyu Zhang. The author also would like to thank useful comments from participants at the 14th International Associatoin for China Planning Annual Conference.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, H. A Spatial Analysis of Obesity: Interaction of Urban Food Environments and Racial Segregation in Chicago. J Urban Health 98, 676–686 (2021). https://doi.org/10.1007/s11524-021-00553-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-021-00553-y