Abstract
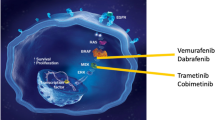
The mitogen-activated protein kinase (MAPK) pathway is a key driver in many histiocytic disorders, including Langerhans cell histiocytosis (LCH) and Erdheim–Chester disease (ECD). This has led to successful and promising treatment with targeted therapies, including BRAF inhibitors and MEK inhibitors. Additional novel inhibitors have also demonstrated encouraging results. Nevertheless, there are several problems concerning targeted therapy that need to be addressed. These include, among others, incomplete responsiveness and the emergence of resistance to BRAF inhibition as observed in other BRAF-mutant malignancies. Drug resistance and relapse after treatment interruption remain problems with current targeted therapies. Targeted therapy does not seem to eradicate the mutated clone, leading to inevitable relapes, which is a huge challenge for the future. More fundamental research and clinical trials are needed to address these issues and to develop improved targeted therapies that can overcome resistance and achieve long-lasting remissions.



Similar content being viewed by others
References
Emile JF, Abla O, Fraitag S, et al. Revised classification of histiocytoses and neoplasms of the macrophage-dendritic cell lineages. Blood. 2016;127(22):2672–81. https://doi.org/10.1182/blood-2016-01-690636.
Goyal G, Tazi A, Go RS, et al. International expert consensus recommendations for the diagnosis and treatment of Langerhans cell histiocytosis in adults. Blood. 2022;139(17):2601–21. https://doi.org/10.1182/blood.2021014343.
Tazi A, de Margerie C, Naccache JM, et al. The natural history of adult pulmonary Langerhans cell histiocytosis: a prospective multicentre study. Orphanet J Rare Dis. 2015;10:30. https://doi.org/10.1186/s13023-015-0249-2.
Vassallo R, Ryu JH, Schroeder DR, et al. Clinical outcomes of pulmonary Langerhans’-cell histiocytosis in adults. N Engl J Med. 2002;346(7):484–90. https://doi.org/10.1056/NEJMoa012087.
Makras P, Yavropoulou MP, Chatziioannou SN, et al. Efficacy of denosumab monotherapy among adults with Langerhans cell histiocytosis: a prospective clinical trial. Am J Hematol. 2023;98(7):E168–71. https://doi.org/10.1002/ajh.26936.
Makras P, Tsoli M, Anastasilakis AD, et al. Denosumab for the treatment of adult multisystem Langerhans cell histiocytosis. Metabolism. 2017;69:107–11. https://doi.org/10.1016/j.metabol.2017.01.004.
Cao XX, Li J, Zhao AL, et al. Methotrexate and cytarabine for adult patients with newly diagnosed Langerhans cell histiocytosis: a single arm, single center, prospective phase 2 study. Am J Hematol. 2020;95(9):E235–8. https://doi.org/10.1002/ajh.25864.
Chang L, Lang M, Lin H, et al. Phase 2 study using low dose cytarabine for adult patients with newly diagnosed Langerhans cell histiocytosis. Leukemia. 2024;38(4):803–9. https://doi.org/10.1038/s41375-024-02174-1.
Duan MH, Han X, Li J, et al. Comparison of vindesine and prednisone and cyclophosphamide, etoposide, vindesine, and prednisone as first-line treatment for adult Langerhans cell histiocytosis: a single-center retrospective study. Leuk Res. 2016;42:43–6. https://doi.org/10.1016/j.leukres.2016.01.012.
Goyal G, Abeykoon JP, Hu M, et al. Single-agent cladribine as an effective front-line therapy for adults with Langerhans cell histiocytosis. Am J Hematol. 2021;96(5):E146–50. https://doi.org/10.1002/ajh.26119.
Zinn DJ, Grimes AB, Lin H, et al. Hydroxyurea: a new old therapy for Langerhans cell histiocytosis. Blood. 2016;128(20):2462–5. https://doi.org/10.1182/blood-2016-06-721993.
Sakamoto K, Kikuchi K, Sako M, et al. Pilot study to estimate the safety and effectiveness of hydroxyurea and methotrexate recurrent Langerhans cell histiocytosis (LCH-HU-pilot). Medicine (Baltimore). 2022;101(50): e31475. https://doi.org/10.1097/md.0000000000031475.
Goyal G, Shah MV, Call TG, et al. Clinical and radiologic responses to cladribine for the treatment of Erdheim-Chester disease. JAMA Oncol. 2017;3(9):1253–6. https://doi.org/10.1001/jamaoncol.2017.0041.
Haroche J, Amoura Z, Trad SG, et al. Variability in the efficacy of interferon-alpha in Erdheim-Chester disease by patient and site of involvement: results in eight patients. Arthritis Rheum. 2006;54(10):3330–6. https://doi.org/10.1002/art.22165.
Goyal G, Heaney ML, Collin M, et al. Erdheim-Chester disease: consensus recommendations for evaluation, diagnosis, and treatment in the molecular era. Blood. 2020;135(22):1929–45. https://doi.org/10.1182/blood.2019003507.
Haroche J, Charlotte F, Arnaud L, et al. High prevalence of BRAF V600E mutations in Erdheim-Chester disease but not in other non-Langerhans cell histiocytoses. Blood. 2012;120(13):2700–3. https://doi.org/10.1182/blood-2012-05-430140.
Badalian-Very G, Vergilio JA, Degar BA, et al. Recurrent BRAF mutations in Langerhans cell histiocytosis. Blood. 2010;116(11):1919–23. https://doi.org/10.1182/blood-2010-04-279083.
Chakraborty R, Hampton OA, Shen X, et al. Mutually exclusive recurrent somatic mutations in MAP2K1 and BRAF support a central role for ERK activation in LCH pathogenesis. Blood. 2014;124(19):3007–15. https://doi.org/10.1182/blood-2014-05-577825.
Durham BH, Lopez Rodrigo E, Picarsic J, et al. Activating mutations in CSF1R and additional receptor tyrosine kinases in histiocytic neoplasms. Nat Med. 2019;25(12):1839–42. https://doi.org/10.1038/s41591-019-0653-6.
Berres ML, Lim KP, Peters T, et al. BRAF-V600E expression in precursor versus differentiated dendritic cells defines clinically distinct LCH risk groups. J Exp Med. 2014;211(4):669–83. https://doi.org/10.1084/jem.20130977.
Chen J, Zhao AL, Duan MH, et al. Diverse kinase alterations and myeloid-associated mutations in adult histiocytosis. Leukemia. 2022;36(2):573–6. https://doi.org/10.1038/s41375-021-01439-3.
Brown NA, Furtado LV, Betz BL, et al. High prevalence of somatic MAP2K1 mutations in BRAF V600E-negative Langerhans cell histiocytosis. Blood. 2014;124(10):1655–8. https://doi.org/10.1182/blood-2014-05-577361.
Nelson DS, van Halteren A, Quispel WT, et al. MAP2K1 and MAP3K1 mutations in Langerhans cell histiocytosis. Genes Chromosomes Cancer. 2015;54(6):361–8. https://doi.org/10.1002/gcc.22247.
Haroche J, Cohen-Aubart F, Amoura Z. Erdheim-Chester disease. Blood. 2020;135(16):1311–8. https://doi.org/10.1182/blood.2019002766.
Lee LH, Gasilina A, Roychoudhury J, et al. Real-time genomic profiling of histiocytoses identifies early-kinase domain BRAF alterations while improving treatment outcomes. JCI Insight. 2017;2(3): e89473. https://doi.org/10.1172/jci.insight.89473.
Mourah S, How-Kit A, Meignin V, et al. Recurrent NRAS mutations in pulmonary Langerhans cell histiocytosis. Eur Respir J. 2016;47(6):1785–96. https://doi.org/10.1183/13993003.01677-2015.
Nelson DS, Quispel W, Badalian-Very G, et al. Somatic activating ARAF mutations in Langerhans cell histiocytosis. Blood. 2014;123(20):3152–5. https://doi.org/10.1182/blood-2013-06-511139.
McClain KL, Bigenwald C, Collin M, et al. Histiocytic disorders. Nat Rev Dis Prim. 2021;7(1):73. https://doi.org/10.1038/s41572-021-00307-9.
Solit DB, Rosen N. Resistance to BRAF inhibition in melanomas. N Engl J Med. 2011;364(8):772–4. https://doi.org/10.1056/NEJMcibr1013704.
Staudinger JZJ, Burgess R, Elledge SJ, Olson EN. PICK1: a perinuclear binding protein and substrate for protein kinase C isolated by the yeast two-hybrid system. J Cell Biol. 1995;128(3):263–71. https://doi.org/10.1083/jcb.128.3.263.
Cheung LW, Hennessy BT, Li J, et al. High frequency of PIK3R1 and PIK3R2 mutations in endometrial cancer elucidates a novel mechanism for regulation of PTEN protein stability. Cancer Discov. 2011;1(2):170–85. https://doi.org/10.1158/2159-8290.CD-11-0039.
Héritier S, Saffroy R, Radosevic-Robin N, et al. Common cancer-associated PIK3CA activating mutations rarely occur in Langerhans cell histiocytosis. Blood. 2015;125(15):2448–9. https://doi.org/10.1182/blood-2015-01-625491.
Kobayashi M, Tojo A. Langerhans cell histiocytosis in adults: advances in pathophysiology and treatment. Cancer Sci. 2018;109(12):3707–13. https://doi.org/10.1111/cas.13817.
Aubart FC, Roos-Weil D, Armand M, et al. High frequency of clonal hematopoiesis in ErdheimChester disease. Blood. 2021;137(4):485–92. https://doi.org/10.1182/blood.2020005101.
McGinnis LM, Nybakken G, Ma L, et al. Frequency of MAP2K1, TP53, and U2AF1 mutations in BRAF-mutated Langerhans cell histiocytosis: further characterizing the genomic landscape of LCH. Am J Surg Pathol. 2018;42(7):885–90. https://doi.org/10.1097/pas.0000000000001057.
Yokokawa Y, Taki T, Chinen Y, et al. Unique clonal relationship between T-cell acute lymphoblastic leukemia and subsequent Langerhans cell histiocytosis with TCR rearrangement and NOTCH1 mutation. Genes Chromosomes Cancer. 2015;54(7):409–17. https://doi.org/10.1002/gcc.22252.
Poulikakos PI, Zhang C, Bollag G, et al. RAF inhibitors transactivate RAF dimers and ERK signalling in cells with wild-type BRAF. Nature. 2010;464(7287):427–30. https://doi.org/10.1038/nature08902.
Diamond EL, Durham BH, Haroche J, et al. Diverse and targetable kinase alterations drive histiocytic neoplasms. Cancer Discov. 2016;6(2):154–65. https://doi.org/10.1158/2159-8290.CD-15-0913.
Tan ACS, Yzer S, Atebara N, et al. Three cases of Erdheim-Chester disease with intraocular manifestations: imaging and histopathology findings of a rare entity. Am J Ophthalmol. 2017;176:141–7. https://doi.org/10.1016/j.ajo.2017.01.017.
Baumann M, Cerny T, Sommacal A, et al. Langerhans cell histiocytosis with central nervous system involvement–complete response to 2-chlorodeoxyadenosine after failure of tyrosine kinase inhibitor therapies with sorafenib and imatinib. Hematol Oncol. 2012;30(2):101–4. https://doi.org/10.1002/hon.1005.
Lito P, Rosen N, Solit DB. Tumor adaptation and resistance to RAF inhibitors. Nat Med. 2013;19(11):1401–9. https://doi.org/10.1038/nm.3392.
Haroche J, Cohen-Aubart F, Emile JF, et al. Dramatic efficacy of vemurafenib in both multisystemic and refractory Erdheim-Chester disease and Langerhans cell histiocytosis harboring the BRAF V600E mutation. Blood. 2013;121(9):1495–500. https://doi.org/10.1182/blood-2012-07-446286.
Haroche J, Cohen-Aubart F, Emile JF, et al. Reproducible and sustained efficacy of targeted therapy with vemurafenib in patients with BRAF(V600E)-mutated Erdheim-Chester disease. J Clin Oncol. 2015;33(5):411–8. https://doi.org/10.1200/jco.2014.57.1950.
Hyman DM, Diamond EL, Vibat CR, et al. Prospective blinded study of BRAFV600E mutation detection in cell-free DNA of patients with systemic histiocytic disorders. Cancer Discov. 2015;5(1):64–71. https://doi.org/10.1158/2159-8290.CD-14-0742.
Heidorn SJ, Milagre C, Whittaker S, et al. Kinase-dead BRAF and oncogenic RAS cooperate to drive tumor progression through CRAF. Cell. 2010;140(2):209–21. https://doi.org/10.1016/j.cell.2009.12.040.
Hatzivassiliou G, Song K, Yen I, et al. RAF inhibitors prime wild-type RAF to activate the MAPK pathway and enhance growth. Nature. 2010;464(7287):431–5. https://doi.org/10.1038/nature08833.
Shi H, He H, Cui L, et al. Transcriptomic landscape of circulating mononuclear phagocytes in Langerhans cell histiocytosis at the single-cell level. Blood. 2021;138(14):1237–48. https://doi.org/10.1182/blood.2020009064.
Delord JP, Robert C, Nyakas M, et al. Phase I dose-escalation and -expansion study of the BRAF inhibitor encorafenib (LGX818) in metastatic BRAF-mutant melanoma. Clin Cancer Res. 2017;23(18):5339–48. https://doi.org/10.1158/1078-0432.Ccr-16-2923.
Wada F, Hiramoto N, Yamashita D, et al. Dramatic response to encorafenib in a patient with Erdheim-Chester disease harboring the BRAF(V600E) mutation. Am J Hematol. 2021;96(8):E295–8. https://doi.org/10.1002/ajh.26232.
Aaroe A, Kurzrock R, Goyal G, et al. Successful Treatment of non-Langerhans cell histiocytosis with the MEK inhibitor trametinib: a multicenter analysis. Blood Adv. 2023. https://doi.org/10.1182/bloodadvances.2022009013.
Diamond EL, Durham BH, Ulaner GA, et al. Efficacy of MEK inhibition in patients with histiocytic neoplasms. Nature. 2019;567(7749):521–4. https://doi.org/10.1038/s41586-019-1012-y.
Gao Y, Chang MT, McKay D, et al. Allele-specific mechanisms of activation of MEK1 mutants determine their properties. Cancer Discov. 2018;8(5):648–61. https://doi.org/10.1158/2159-8290.CD-17-1452.
Ahronian LG, Sennott EM, Van Allen EM, et al. Clinical acquired resistance to RAF inhibitor combinations in BRAF-mutant colorectal cancer through MAPK pathway alterations. Cancer Discov. 2015;5(4):358–67. https://doi.org/10.1158/2159-8290.Cd-14-1518.
Hazar-Rethinam M, Kleyman M, Han GC, et al. Convergent therapeutic strategies to overcome the heterogeneity of acquired resistance in BRAF(V600E) colorectal cancer. Cancer Discov. 2018;8(4):417–27. https://doi.org/10.1158/2159-8290.Cd-17-1227.
Gilmartin AG, Bleam MR, Groy A, et al. GSK1120212 (JTP-74057) is an inhibitor of MEK activity and activation with favorable pharmacokinetic properties for sustained in vivo pathway inhibition. Clin Cancer Res. 2011;17(5):989–1000. https://doi.org/10.1158/1078-0432.Ccr-10-2200.
Mizuno S, Ikegami M, Koyama T, et al. High-throughput functional evaluation of MAP2K1 variants in cancer. Mol Cancer Ther. 2023;22(2):227–39. https://doi.org/10.1158/1535-7163.MCT-22-0302.
Hanrahan AJ, Sylvester BE, Chang MT, et al. Leveraging systematic functional analysis to benchmark an in silico framework distinguishes driver from passenger MEK mutants in cancer. Cancer Res. 2020;80(19):4233–43. https://doi.org/10.1158/0008-5472.CAN-20-0865.
Shah NP, Kasap C, Weier C, et al. Transient potent BCR-ABL inhibition is sufficient to commit chronic myeloid leukemia cells irreversibly to apoptosis. Cancer Cell. 2008;14(6):485–93. https://doi.org/10.1016/j.ccr.2008.11.001.
Papapanagiotou M, Griewank KG, Hillen U, et al. Trametinib-induced remission of an MEK1-mutated langerhans cell histiocytosis. JCO Precis Oncol. 2017;1:1–5. https://doi.org/10.1200/po.16.00070.
Roeser A, Jouenne F, Vercellino L, et al. Dramatic response after switching MEK inhibitors in a patient with refractory mixed histiocytosis. J Hematol. 2022;11(5):185–9. https://doi.org/10.14740/jh1030.
Lian T, Li C, Wang H. Trametinib in the treatment of multiple malignancies harboring MEK1 mutations. Cancer Treat Rev. 2019;81: 101907. https://doi.org/10.1016/j.ctrv.2019.101907.
Wagle N, Van Allen EM, Treacy DJ, et al. MAP kinase pathway alterations in BRAF-mutant melanoma patients with acquired resistance to combined RAF/MEK inhibition. Cancer Discov. 2014;4(1):61–8. https://doi.org/10.1158/2159-8290.CD-13-0631.
Durham BH, Hershkovitz-Rokah O, Abdel-Wahab O, et al. Mutant PIK3CA is a targetable driver alteration in histiocytic neoplasms. Blood Adv. 2023;7(23):7319–28. https://doi.org/10.1182/bloodadvances.2022009349.
Arceci RJ, Allen CE, Dunkel IJ, et al. A phase IIa study of afuresertib, an oral pan-AKT inhibitor, in patients with Langerhans cell histiocytosis. Pediatr Blood Cancer. 2017. https://doi.org/10.1002/pbc.26325.
Dumble M, Crouthamel MC, Zhang SY, et al. Discovery of novel AKT inhibitors with enhanced anti-tumor effects in combination with the MEK inhibitor. PLoS ONE. 2014;9(6): e100880. https://doi.org/10.1371/journal.pone.0100880.
Gianfreda D, Nicastro M, Galetti M, et al. Sirolimus plus prednisone for Erdheim-Chester disease: an open-label trial. Blood. 2015;126(10):1163–71. https://doi.org/10.1182/blood-2015-01-620377.
Pegoraro FMV, Peyronel F, Westenend PJ, Hendriksz TR, Roperto RM, Palumbo AA, Sieni E, Romagnani P, van Bommel EFH, Vaglio A. Long term follow up of mTOR inhibition for Erdheim-Chester disease. Blood. 2020;135(22):1994–7. https://doi.org/10.1083/jcb.128.3.263.
Abeykoon JP, Lasho TL, Dasari S, et al. Sustained, complete response to pexidartinib in a patient with CSF1R-mutated Erdheim-Chester disease. Am J Hematol. 2022;97(3):293–302. https://doi.org/10.1002/ajh.26441.
Goyal G, Parikh R, Richman J, et al. Spectrum of second primary malignancies and cause-specific mortality in pediatric and adult Langerhans cell histiocytosis. Leuk Res. 2023;126: 107032. https://doi.org/10.1016/j.leukres.2023.107032.
Papo M, Diamond EL, Cohen-Aubart F, et al. High prevalence of myeloid neoplasms in adults with non-Langerhans cell histiocytosis. Blood. 2017;130(8):1007–13. https://doi.org/10.1182/blood-2017-01-761718.
Bonnet P, Chasset F, Moguelet P, et al. Erdheim-Chester disease associated with chronic myelomonocytic leukemia harboring the same clonal mutation. Haematologica. 2019;104(11):e530–3. https://doi.org/10.3324/haematol.2019.223552.
Milne P, Bigley V, Bacon CM, et al. Hematopoietic origin of Langerhans cell histiocytosis and Erdheim-Chester disease in adults. Blood. 2017;130(2):167–75. https://doi.org/10.1182/blood-2016-12-757823.
Konstantinou MP, Lucas P, Uthurriague C, et al. Langerhans cell histiocytosis associated with chronic myelomonocytic leukaemia both harbouring the same BRAF V600E mutation: efficacy of vemurafenib. J Eur Acad Dermatol Venereol. 2021;35(2):e120–1. https://doi.org/10.1111/jdv.16850.
Abdel-Wahab O, Klimek VM, Gaskell AA, et al. Efficacy of intermittent combined RAF and MEK inhibition in a patient with concurrent BRAF- and NRAS-mutant malignancies. Cancer Discov. 2014;4(5):538–45. https://doi.org/10.1158/2159-8290.Cd-13-1038.
Yao Z, Gao Y, Su W, et al. RAF inhibitor PLX8394 selectively disrupts BRAF dimers and RAS-independent BRAF-mutant-driven signaling. Nat Med. 2019;25(2):284–91. https://doi.org/10.1038/s41591-018-0274-5.
Nordmann TM, Juengling FD, Recher M, et al. Trametinib after disease reactivation under dabrafenib in Erdheim-Chester disease with both BRAF and KRAS mutations. Blood. 2017;129(7):879–82. https://doi.org/10.1182/blood-2016-09-740217.
Nazarian R, Shi H, Wang Q, et al. Melanomas acquire resistance to B-RAF(V600E) inhibition by RTK or N-RAS upregulation. Nature. 2010;468(7326):973–7. https://doi.org/10.1038/nature09626.
Chakraborty R, Burke TM, Hampton OA, et al. Alternative genetic mechanisms of BRAF activation in Langerhans cell histiocytosis. Blood. 2016;128(21):2533–7. https://doi.org/10.1182/blood-2016-08-733790.
Héritier S, Hélias-Rodzewicz Z, Chakraborty R, et al. New somatic BRAF splicing mutation in Langerhans cell histiocytosis. Mol Cancer. 2017;16(1):115. https://doi.org/10.1186/s12943-017-0690-z.
Zhang C, Spevak W, Zhang Y, et al. RAF inhibitors that evade paradoxical MAPK pathway activation. Nature. 2015;526(7574):583–6. https://doi.org/10.1038/nature14982.
Whittaker SR, Cowley GS, Wagner S, et al. Combined pan-RAF and MEK inhibition overcomes multiple resistance mechanisms to selective RAF inhibitors. Mol Cancer Ther. 2015;14(12):2700–11. https://doi.org/10.1158/1535-7163.Mct-15-0136-t.
Peng SB, Henry JR, Kaufman MD, et al. Inhibition of RAF isoforms and active dimers by LY3009120 leads to anti-tumor activities in RAS or BRAF mutant cancers. Cancer Cell. 2015;28(3):384–98. https://doi.org/10.1016/j.ccell.2015.08.002.
Jain P, Surrey LF, Straka J, et al. BRAF fusions in pediatric histiocytic neoplasms define distinct therapeutic responsiveness to RAF paradox breakers. Pediatr Blood Cancer. 2021;68(6): e28933. https://doi.org/10.1002/pbc.28933.
Desai J, Gan H, Barrow C, et al. Phase I, Open-label, dose-escalation/dose-expansion study of lifirafenib (BGB-283), an RAF family kinase inhibitor, in patients with solid tumors. J Clin Oncol. 2020;38(19):2140–50. https://doi.org/10.1200/jco.19.02654.
Okaniwa M, Hirose M, Arita T, et al. Discovery of a selective kinase inhibitor (TAK-632) targeting pan-RAF inhibition: design, synthesis, and biological evaluation of C-7-substituted 1,3-benzothiazole derivatives. J Med Chem. 2013;56(16):6478–94. https://doi.org/10.1021/jm400778d.
Gunderwala AY, Nimbvikar AA, Cope NJ, et al. Development of allosteric BRAF peptide inhibitors targeting the dimer interface of BRAF. ACS Chem Biol. 2019;14(7):1471–80. https://doi.org/10.1021/acschembio.9b00191.
Beneker CM, Rovoli M, Kontopidis G, et al. Design and synthesis of type-IV inhibitors of BRAF kinase that block dimerization and overcome paradoxical MEK/ERK activation. J Med Chem. 2019;62(8):3886–97. https://doi.org/10.1021/acs.jmedchem.8b01288.
Germann UA, Furey BF, Markland W, et al. Targeting the MAPK signaling pathway in cancer: promising preclinical activity with the novel selective ERK1/2 inhibitor BVD-523 (ulixertinib). Mol Cancer Ther. 2017;16(11):2351–63. https://doi.org/10.1158/1535-7163.Mct-17-0456.
Kopetz S, Grothey A, Yaeger R, et al. Encorafenib, binimetinib, and cetuximab in BRAF V600E-mutated colorectal cancer. N Engl J Med. 2019;381(17):1632–43. https://doi.org/10.1056/NEJMoa1908075.
Mitchell J, Kelly J, Kvedaraite E, et al. Foxp3(+) Tregs from Langerhans cell histiocytosis lesions co-express CD56 and have a definitively regulatory capacity. Clin Immunol. 2020;215: 108418. https://doi.org/10.1016/j.clim.2020.108418.
Egeler RM, Favara BE, van Meurs M, et al. Differential In situ cytokine profiles of Langerhans-like cells and T cells in Langerhans cell histiocytosis: abundant expression of cytokines relevant to disease and treatment. Blood. 1999;94(12):4195–201.
Mitchell J, Kvedaraite E, von Bahr GT, et al. Plasma signaling factors in patients with Langerhans cell histiocytosis (LCH) correlate with relative frequencies of LCH cells and T cells within lesions. Front Pediatr. 2022;10: 872859. https://doi.org/10.3389/fped.2022.872859.
Zeng K, Wang Z, Ohshima K, et al. BRAF V600E mutation correlates with suppressive tumor immune microenvironment and reduced disease-free survival in Langerhans cell histiocytosis. Oncoimmunology. 2016;5(7): e1185582. https://doi.org/10.1080/2162402X.2016.1185582.
Crowley E, Di Nicolantonio F, Loupakis F, et al. Liquid biopsy: monitoring cancer-genetics in the blood. Nat Rev Clin Oncol. 2013;10(8):472–84. https://doi.org/10.1038/nrclinonc.2013.110.
Schwentner R, Kolenova A, Jug G, et al. Longitudinal assessment of peripheral blood BRAFV600E levels in patients with Langerhans cell histiocytosis. Pediatr Res. 2019;85(6):856–64. https://doi.org/10.1038/s41390-018-0238-y.
Heritier S, Helias-Rodzewicz Z, Lapillonne H, et al. Circulating cell-free BRAF(V600E) as a biomarker in children with Langerhans cell histiocytosis. Br J Haematol. 2017;178(3):457–67. https://doi.org/10.1111/bjh.14695.
Evseev D, Kalinina I, Raykina E, et al. Vemurafenib provides a rapid and robust clinical response in pediatric Langerhans cell histiocytosis with the BRAF V600E mutation but does not eliminate low-level minimal residual disease per ddPCR using cell-free circulating DNA. Int J Hematol. 2021;114(6):725–34. https://doi.org/10.1007/s12185-021-03205-8.
Vemurafenib for refractory multisystem Langerhans cell histiocytosis in childrenan international observational study. J Clin Oncol. 37(31):2857–65. https://doi.org/10.1200/JCO.19.00456.
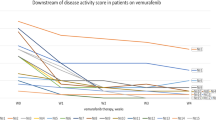
Cohen Aubart F, Emile JF, Carrat F, et al. Targeted therapies in 54 patients with Erdheim-Chester disease, including follow-up after interruption (the LOVE study). Blood. 2017;130(11):1377–80. https://doi.org/10.1182/blood-2017-03-771873.
Reiner AS, Durham BH, Yabe M, et al. Outcomes after interruption of targeted therapy in patients with histiocytic neoplasms. Br J Haematol. 2023. https://doi.org/10.1111/bjh.18964.
Bhatia A, Ulaner G, Rampal R, et al. Single-agent dabrafenib for BRAF(V600E)-mutated histiocytosis. Haematologica. 2018;103(4):e177–80. https://doi.org/10.3324/haematol.2017.185298.
Diamond EL, Subbiah V, Lockhart AC, et al. Vemurafenib for BRAF V600-mutant Erdheim-Chester disease and Langerhans cell histiocytosis: analysis of data from the histology-independent, phase 2, open-label VE-BASKET study. JAMA Oncol. 2018;4(3):384–8. https://doi.org/10.1001/jamaoncol.2017.5029.
Hazim AZ, Ruan GJ, Ravindran A, et al. Efficacy of BRAF-inhibitor therapy in BRAF(V600E)-mutated adult Langerhans cell histiocytosis. Oncologist. 2020;25(12):1001–4. https://doi.org/10.1002/onco.13541.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was supported by grants from institutional research funding provided by the Beijing Natural Science Haidian frontier Foundation (Grant no. L222081 to Cao XX) and the National High Level Hospital Clinical Research Funding (2022-PUMCH-A-193).
Conflict of interest
He Lin, Xin-xin Cao declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data, materials, and code
Not applicable.
Authors' contributions
H.L. and X.C. wrote the main manuscript text. H.L. prepared figures and tables. X.C. reviewed the manuscript and provided helpful comments. All authors read and approved the final manuscript.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lin, H., Cao, Xx. Current State of Targeted Therapy in Adult Langerhans Cell Histiocytosis and Erdheim–Chester Disease. Targ Oncol 19, 691–703 (2024). https://doi.org/10.1007/s11523-024-01080-x
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-024-01080-x