Abstract
Medical devices, being life-saving tools, are considered to be a boon for healthcare system. However, in addition to their therapeutic effects, there are several ill consequences that are caused by these devices. An effective cohort vigilant system was needed to manage such adverse effects. This had led to the introduction of materiovigilance. Materiovigilance is the study and follow-up of occurrences that arise as a result from the usage of the medical equipment. It not only manages adverse events (AE) but also creates harmonization among countries. Keeping these objectives in focus, the principles, perspectives, and practices with regard to materiovigilance that are followed in the USA, Europe, China, Japan, Australia, Canada, and India are being compared. Such a comparison is essential, which will help us to understand the gaps in the current regulatory systems in the above-mentioned countries and furthermore will provide a comprehensive picture to the regulatory authorities to amend any existing laws if required. These amendments may ensure optimal patient safety by providing them a benign experience from the use of medical devices.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
History of medical devices
Basic medical devices like wooden splints to keep fractured bones in position, improvised crutches, or handmade stretchers to hold the sick have undeniably existed from time immemorial. Archeological sites and various ancient literatures have provided ample evidence for their use. For example, the use of medical instruments related to dentistry has been predominantly recorded by the ancient Egyptians and Etruscans. The use of exaggerated medical promises concerning mechanical and electrical instruments could be traced back to John Graham of England, who in 1745 advertised the “celestial bed” which was connected by electric coils and was employed as a cure for sterility. In the 1700s, the best-known experimental instruments were probably those used by Franz Anton Mesmer, who had arrived in Paris in February 1778. Mesmer argued that “animal magnetism” was the main agent of nature, and it was the basis of all well-being (Hutt and HuttII 1984). According to Mesmer, the ill could be treated by recharging them with animal magnetism using magnets and, later, large tubs in which iron rods were mounted, binding patients to specially magnetized water jars. The Royal Commission convened by the medical elite, composed of influential scientists such as Antoine Lavoisier and Benjamin Franklin, carried out experiments and concluded in 1784 that Mesmer’s cure was unsuccessful. It was Dr Elisha Perkins who created the first renowned bogus medical device to be sold in the USA towards the end of 1700s. Perkins produced two brass and iron poles, about 3 in long, dubbed “Perkins” Patent Tractors. He sold them all over the world and said that they can remove any disease from the body. It was revealed as a hoax after 10 years. Throughout the 1800s, media and political attention in the USA centered on the need for laws to regulate the adulteration and misbranding of food and medications, but not medical equipment. Miscellaneous medical devices flourished during this time (Hutt and HuttII 1984). A 1916 article published by the American Medical Association, dedicated exclusively to “cures” for deafness, reported on many useless instruments. One of the most common misleading instruments of this period was the Abrams “dynamizer” computer. By inserting a blood sample in the system, Abrams argued that he could diagnose the particular disease what the person had contracted and also locate the exact tissue inside the body where the disease had its focus. By the time Abrams died in 1924, his machine had already been revealed as a scam (Hutt and HuttII 1984).
Considering all these evidence, it could be easily concluded that faulty medical devices and their ill consequences have existed in history for hundreds of years. Various case reports were brought to limelight in the twenty-first century. A global investigation found that several medical devices were still being sold in global markets even after these equipment were marked unsafe. Such unsafe medical devices have caused more than 1.7 million reported injuries worldwide, and along with it more than 83,000 deaths have been reported in the last 12 years arising from such use (Healthcare IT news 2018). Breast implants, pacemakers, contraceptives, incubators, and artificial hips grafted into patients’ bodies are some of the most prevalent and dangerous medical equipment that have triggered adverse outcomes.
In 2002, an extremely rare case of implantable cardioverter defibrillator malfunction was reported in a 60-year-old man. He received his very first implantable cardioverter defibrillator (ICD) in 2002 but later in 2012 changed the device model without any complications (Assaad et al. 2016). After 6 months, during his routine checkup in wireless interrogations, it was noticed that all communication with the ICD were lost. The patient experienced multiple shocks via electrocardiogram telemetry each time the doctors tried to communicate with the ICD. Though the patient recovered eventually, a new generator had to be placed which was connected to lead (Assaad et al. 2016).
Similarly, in 2010, a major incident took place when a reputed pharmaceutical company, “Johnson and Johnson,” had to backload all their ASR XL Acetabular hip replacement systems (metal-on-metal). Patients had to undergo repeated surgeries due to the release of metallic debris into the bloodstream, especially in the case of metal implants. Another issue faced by patients was the friction caused by the wearing of both prosthetic ball and socket (Ramesh 2019). With the unstemmed rise in the number of similar cases, the authorities took the decision for a worldwide recall. In India, 4700 similar ASR implants were recalled due to faulty function. One such effect of this faulty medical device was observed in a 44-year-old man, who had suffered from vision issues, irregular heartbeats, and difficulty in walking (Healthcare IT news 2018). It was claimed that all these events were the result of an implanted replacement hip from Johnson and Johnson drug company. As the number of cases was rising at an alarming rate, the Health Ministry of India set up an expert committee in 2017 to evaluate and examine all the issues that were reported due to the implants (Healthcare IT news 2018).
In 2014, a case was reported of a 45-year-old patient who was seeking help after years of suffering. His doctor assured him of a medical system that would ease his discomfort. The doctor had claimed that although it would not repair the nerve damage in his mangled arm, but a spinal-cord stimulator would help mask his discomfort. However, the stimulator failed shortly after it was implanted. During the surgery, the patient reported having been stunned several times that he could not sleep and even fell down the stairs. The patient now could hardly move and is a captive in his own room.
Medical equipment makers and physicians have stated for years that stimulators for spinal cord are a miracle for crores of people distressed from a varied range of painful conditions. These devices are marketed as an alternative to drug addiction and for chronic pain relief in the elderly. But the number of injury cases accounts for the third-highest number of medical condition incidents. The FDA has been reported with more than 80,000 such accidents since 2008. According to FDA reports, patients have indicated that they have been shocked or burnt or have suffered paraplegia. Metal hip replacements and insulin pumps were the two instruments that have reported more accident cases. There are more than 500 cases of people who died from spinal cord stimulators, but specifics are sparse (Weiss and Mohr 2018).
Similar to the recall of Johnson and Johnson hip implants, one such recall was made by FDA of implantable cardioverter defibrillators (ICDs) (U.S. Food and Drug Administration 2019a, b, c). Due to the fault in the manufacturing process, the aluminum wires were partially exposed causing electrical failures. The wires that were not properly insulated were prone to electrical malfunction of the capacitor. This led to issues in the delivery of high voltage therapy. Before the recall occurred in 2016, this device was being used by 350,000 patients globally. One fatal case involving an implantable defibrillator was recorded in the USA, where the family of a 27-year-old woman filed a litigation after an implantable defibrillator that was later called back by St. Jude Medical for battery difficulties failed to re-start her heart, resulting in her death (Healthcare IT news 2018).
Another shocking incident took place in Mumbai, India on 29 May 2017 where 4 infants died when a short circuit ignited a fire in the incubator. Reportedly, the infants were said to have been severely charred after a fire started out in the incubator (India.com 2017). To reduce fatality and severity rates, all these incidents led to a major call for action in India. Similar incidents of unsafe medical device use took place in India and were mostly seen in the cities of Meerut, Delhi, Hyderabad, and Mumbai. In Meerut, two babies including a newborn and a 3-month-old baby were severely burned after an incubator caught fire due to a short circuit. The 3-month-old infant succumbed to his injuries. Another newborn girl got 25% burn injuries (Bhatia 2015).
Penalties for device failure
In the USA, where the drug and equipment suppliers are required to report for compensation to physicians, the 10 biggest medical device firms had so far reimbursed more than $600 million to doctors or their clinics to fund consultation services, testing, travel, and entertainment expenses (Weiss and Mohr 2018).
It has been reported that the top four spinal-cord stimulation suppliers have invested more than $22 million since 2017 to impact supporting policies for the overall industry. However, companies that advertise goods for unapproved purposes and compensate for tests that assert their safety and efficacy have been fined heavily. In a 2016 lawsuit, Olympus Corporation of America agreed to pay $623.2 million to settle fraud proceedings and legal lawsuits related to a conspiracy to pay kickbacks to physicians and hospitals. Medtronic Inc. agreed to pay $2.8 million to resolve government allegations that claimed the corporation had harmed patients and defrauded public healthcare services by offering cash inducements to doctors which had turned them into salesmen for expensive procedures (Anson 2018).
It is commonly seen that, when a complaint regarding a specific medical device is not resolved, then immediate action has been taken against it by recalling the faulty product. The guidelines of GHTF along with MHRA define “recall” as a field safety corrective action (FSRA) to decrease the risk of any harm to patients. FDA has issued a list of such medical devices which had failed and were recalled. A chronological list of recent recalled medical devices is shown in Table 1 along with the reason of their withdrawal.
Depiction of medical devices and emergence of materiovigilance (MV)
A medical device, in accordance with the Food and Drug Administration (FDA), is defined as a machine, implement, instrument, implant, or an in vitro component that is used for the treatment, cure, diagnosis, and prevention of a particular disease (U.S. Food and Drug Administration 2018). Medical devices are also anticipated to impinge on the structure and body function of both humans and animals but are not dependent on being metabolized for the attainment of any of its primary anticipated purpose (U.S. Food and Drug Administration 2018). There is an immense rise in the use of medical devices. Due to this, it is mandatory to ensure their quality and efficiency. The device quality, however, varies and even the finest device might fail in medical practice. Moreover, these devices may also lead to safety issues that might unintentionally harm the patients. Therefore, to overcome these issues, post-marketing surveillance plays a vital role as it helps in evaluating the performance of devices and focuses on their safety (Shukla et al. 2020). Apart from post-marketing surveillance, harmonization of medical devices is also necessary. The main aim of harmonization is invigorating merging in regulatory practice associated to ensure the quality, effectiveness, performance, and safety of medical equipment, thereby stimulating international demand and scientific novelty (Dave et al. 2018). Harmonization is an indispensable effort which reduces the time duration in marketing of these medical devices and thereby helps in cutting the cost that is required to market a device. Apart from this, it works on enhancing the efficacy and safety of the device and, thus, lifting the faith and confidence of consumers.
Pharmacovigilance (PV) is a branch of pharmaceutical sciences that deals with the identification, assessment, monitoring, and management of adverse drug reactions (ADR) or adverse events (AE) related to respective pharmaceutical products. In 2011, the International Medical Device Regulators Forum (IMDRAF) was established for monitoring adverse events related to medical equipment. It aimed to accelerate convergence and harmonization of international medical device regulatory. This international organization comprised 10 countries that include Japan, China, India, EU, USA, and South Korea (Yoon et al. 2019) which led to the introduction of materiovigilance (MV).
MV is defined as the study and follow-up of incidents that might have resulted from the usage of medical devices. MV detects adverse events associated with medical equipment, as all such equipment might have certain risks and may also cause complications under unambiguous circumstances. Monitoring of the devices would enable the perilous devices to be withdrawn from the market, and apart from withdrawing, the company could also work on elimination of the faults. This would improve the quality of devices, thus, providing safety to patient and consumers (Kumar et al. 2016).
Different countries possess different guidelines and regulations. To achieve consistency between regulatory systems of medical device at national level and to achieve effectiveness and safety, 5 nations joined the Global Harmonization Task Force (GHTF)in 1992; USA, Canada, Japan, Europe, and Australia (Gupta et al. 2010). Medical devices are defined differently in each country, but according to the GHTF, a medical device is an equipment, implement, instrument, calibrator, substance, or software that is planned to be used for one of the stated purposes by the producer for an envisioned usage in humans. This also consisted of medical support systems like supporting or sustaining life, conception and control, prevention, diagnosis and monitoring of injury or disease, and disinfection of medical equipment. Moreover, the Therapeutic Goods and Administration (TGA) has included hospitals, commercial grade disinfectants, tampons, and households in its definition, whereas, the Medicines and Healthcare Products Regulatory Agency (MHRA) has left out several elements that are used to disinfect medical devices. Surprisingly, India has long considered medical equipment to be “drugs.” Interestingly, India has been still regarding medical devices to be “drugs.”
Regulations on medical instruments scarcely existed in most of the countries, and the regulatory restrictions were very limited to discourage the usage of low-quality equipment. As a result, there was a significant desire to design effective medical device legislation policies in order to assess their efficacy, safety, and efficiency. Fortunately, since the early 1980s, the regulatory landscape for medical devices has drastically transformed. With the implementation of numerous laws, there was also a need for harmonization of countries or regions on medical equipment regulations to curb the regulatory hurdles and to speed up the access to medical instruments. Keeping this objective in focus, regulations across the world may be reviewed and compared with semi regulated countries. Comparisons could help to understand the gaps in the global regulatory practices and will provide a vision to regulatory authorities to amend the laws accordingly for a safer and efficacious medical device.
Classification of medical devices
There exists a wide diversity in the classification system of medical devices worldwide, and there is a need to facilitate the process of global harmonization while classifying the medical devices. The global classification of medical devices has been compared in Table 2.
Materiovigilance across the globe
USA
In the USA, medical devices fall below the US Federal Drug and Administration (USFDA). It is mandatory that the device should be sanctioned by the Food and Drug Administration (FDA) to be efficient as well as safe for the intended purpose before being officially presented into the marketplace. Manufacturers are expected to submit or present only the data necessary to demonstrate device efficacy and safety in the USA, according to the “least burdensome approach.” The FDA’s Center for Devices and Radiological Health supervise re-labeling, manufacturing, importing, exporting, and packing medical devices (U.S. Food and Drug Administration 2020a).
Acceptance criteria for devices in the USA
In the USA, 3 regulatory pathways are being used for device approval. The pre-marketing notification (PMN), pre-market approval (PMA), and humanitarian device exemption (HDE) pathways are among them.
Pre-marketing Notification Pathway (PMN)
Every organization that wishes to market devices in the USA that are intended for human use does not require PMA (post approval application). They need to submit a 510(K) form to FDA unless the equipment has been exempted from 510(K) requirements of the Federal Food, Drug, and Cosmetic Act (FD&C Act). Before marketing a medical device, the person submitting an application must receive an order from the FDA, which approves and states that the device is substantially equivalent (SE) and may be marketed in the US market.
A premature submission to the FDA is made by submitting a 510(K) form to indicate that the medical device that will be sold is efficient and safe, and that it is substantially equivalent to a legitimately marketed device. It is advised that applicants equate their medical device with one that is comparable and has been lawfully marketed and that they back up their substantial equivalence claims. A legitimately marketed device is one that is SE and has gone through the 510(K) procedure and had been lawfully marketed before 28 May 1976, or one that has been classified again from class-3 to class-2 or class-1. The predicate is the lawfully marketed device to which an equivalence is drawn. As a predicate, any lawfully marketed device can be utilized (U.S. Food and Drug Administration 2020b).
The FD&C and regulation 510(K) does not specifically mention who needs to submit a 510(K). This should be submitted by domestic manufacturers who are going to introduce a device in the marketplace. The completed device manufacturers are bound to submit a 510(K) if they fabricate a device in accordance with their own specifications and, subsequently, marketplace the same in the USA. Accouterments to the completed devices sold to consumers are largely considered as finished devices. Conversely, manufacturers of device’s components are not actually required to submit 510(K) unless such components are being promoted for trade. Furthermore, contract manufacturers are free from filing a 510(K) because they produce devices under contract to someone else’s standards (U.S. Food and Drug Administration 2020b).
Requirement of 510(k): Anyone wishing to sell a device in the USA after 28 May 1976 must first submit a 510(K) application. It must be submitted at least 90 days before the device is offered for sale. Apart from this, if there is any alteration to the legitimately marketed equipment and if such a variation could easily alter the effectiveness, and safety of the said medical device should submit a 510(K). Any changes being made should be in agreement with the 21CFR820 quality regulation and must be documented in the master record of the device. It is also said that a justification should also be recorded in change control records describing why or why not a new 510(K) was submitted (U.S. Food and Drug Administration 2020b).
Pre-market Approval Pathway (PMA)
It is the FDA’s regulatory and scientific evaluation procedure for determining the efficacy and safety of Class-3 medical devices. Class-3 devices are the ones that either sustain human health or pose an undue risk of injury or illness. Because of the significant risk associated with Class-3 medical devices, FDA has stated that specific and general restrictions are not adequate to ensure their effectiveness and safety. As a result, in order to get marketing approval, these devices must submit a PMA application under section 515 of the Act FD&C (U.S. Food and Drug Administration 2019a). As a result, anyone wishing to commercialize a device in the USA without a PMA must submit a 510K form to the FDA.
Requirement of PMA: This is the most stringent regulation category for medical equipment, and it applies to Class-3 devices. The CFR includes a regulation digit for Class-3 products that were promoted prior to the 1976 Medical Device Amendment. PMA is required by the CFR for Class-3 devices, which specifies that the device is present in Class-3 and gives an operating date of the necessity for PMA (U.S. Food and Drug Administration 2019a).
PMA frequently focuses on novel concepts, and most of these new concepts are not commercialized prior to the medical equipment regulations. As a result, there is no classification restriction within CFR for these novel notions. In such circumstances, the product categorization database, which specifies the device description and product code, will be used. In some circumstances, it is unclear whether unclassified devices require a PMA. In such cases, we search for the product using a three-letter product code in the PMA database or the 510(K) Pre-market Notification Database. These databases are often accessed by hypertext links just at the head of the product classification system web page. In the product code box, type in the three-letter code. When the new device is approximately similar to previously approved devices, the applicant must file a 510(k) application (K). Furthermore, as previously stated, a new type of equipment may not be included in the product classification databases. If a device is regarded to be a high-risk device, that is, if it sustains human life, is significantly important in preventing human health damage, and has promise but is not a SI, it must have an approved PMA before being commercialized in the USA (U.S. Food and Drug Administration 2019a).
Humanitarian Device Exemption (HDE) pathway
A rare disease is defined as a disorder that affects less than 200,000 people in the USA, as defined under the Orphan Drug Act (ODA) of 1984. Only a small percentage of the 7000 recognized rare diseases in the USA have approved therapies. Rare diseases are described as illnesses that affect a limited number of people. As a result, meeting the FDA’s safety and assurance standards is tough. To address this issue, the US Congress enacted a provision in the Safe Medical Device Act that establishes a new regulatory pathway for goods intended for use in conditions that impact only a small number of people. A medical device introduced for this, termed as Humanitarian Use Device (HUD) (U.S. Food and Drug Administration 2019b), is intended to benefit patients in the diagnosis and treatment of rare diseases. For this, a marketing application for HUD came into limelight which was termed as Humanitarian Device Exemption program (HDE).
Under the FDC Act, a HUD is authorized to be sold only in the market after approval from HDE, if the device is planned for diagnosis and management of the ailment which arises in pediatric population and the device is categorized for its usage in pediatric patients. Another condition is that, if it occurs in adults and does not arise in pediatric patients, and when in such numbers the device improvement for such pediatric population is not possible or hazardous. HDE applicants whose devices meet one of the eligibility criteria as mentioned above and wish to sell it for profit should submit enough supportive documents in original to the FDA HDE application. HDE holders who did not submit the request in the original application of HDE but desire to vend their devices for profit might submit an appendage and provide sufficient documents to exhibit that the HUD meets the admissibility criteria (U.S. Food and Drug Administration 2019c).
Reporting of adverse events in medical devices
The Federal Food, Drug, and Cosmetic Act, under the Section 519, grants permission to the FDA to require medical device reports from manufacturers, device user facilities, and importers (U.S. Food and Drug Administration 2020c). In addition, they are obliged to report to the FDA certain adverse outcomes that occur as a result of medical devices. Aside from obligatory reporters, the FDA is also interested in hearing from others. Patients, consumers, and healthcare professionals are encouraged to report major adverse events, as well as quality issues of product, errors, and treatment failures, to the FDA on a voluntary basis. All these reports together help in improving the patient safety (U.S. Food and Drug Administration 2020d).
Obligatory medical device reporting requirements
The 21 CFR Part 803, reporting of medical device consists of some mandatory requirements for importers, manufacturers, device users’ amenities to report certain product problems including device linked adverse outcomes to the FDA.
-
Manufacturers—When they discover that one of their devices has resulted in death or serious harm, they notify the FDA. They must also notify the authorities if they discover if the device has crashed and is causing or contributing to a major injury or death.
-
Importers—If they see one of the devices has caused death or serious harm, they notify it to the manufacturer or the FDA. Importers, on the other hand, must only report malfunction devices to the manufacturers.
-
Device user facilities—Hospitals, nursing homes, outpatient diagnostic facilities, and surgical institutions, to name a few, fall within this group. These consumer facilities should be designed to notify adverse incidents with medical devices to the producer or the FDA. If a medical equipment producer is unknown, the consumer facilities must notify the FDA, or else each serious case using a medical device would be reported to the manufacturers. A consumer facility is really not required to disclose a device malfunction, but that can willingly report such problems to the FDA using MedWatch Form FDA 3500 as part of the adverse event reporting program (U.S. Food and Drug Administration 2020d).
The various types of reporting and their time frames are presented in Table 3 below.
Europe
In Europe, harmonization with the European Union (EU) guidelines are being followed for approval of medical devices. The procedure for medical device regulatory relies upon the MDD (Medical Device Directives) which consists of 3 principal directives that are mainly revised for marketing and regulation of medical devices in a safe manner. These are:
-
Directive 90/385/EC (European commission) regulates implanted devices
-
The 93/42/EC directive regulates numerous additional devices
-
The directive 98/99/EC regulates diagnostic devices
According to Directive 93/42/EC, a medical device is any apparatus, tool, material, or equipment, used in combination or alone, that is intended to be used by humans for diagnosis, monitoring, prevention, or alleviation of diseases, treatment, compensation for an injury, or conception control, but that will not attain its primary expected action on the human through immunological, pharmacological, or some other means.
Europe consists of a total of 50 NB, and these are private organizations that sign the contract with producers of medical devices and charge a payment for medical device certification. The pharmaceutical company is allowed to select a NB according to its will for reviewing a specific class of medical devices. The main work of a NB is to inspect the application very carefully and to fulfill the EC regulation. If all the supervisory provisions are met by the medical devices, it will issue a CE mark on the devices. The devices with CE marks are then ready to be vended in any nation within Europe. This shows that the medical device/any product complies with the relevant safety legislation. This action of NB is known as “conformity assessment” in the Europe. Once the medical devices are sanctioned under the mark of CE, no other evaluation is required. However, a novel regulation of 2010 made some strict rules for sanction of medical devices in characteristic of similarities between new devices to that of the predicate devices, the one that are already present in the market. Following steps show the decentralized approval process of medical devices in Europe (Dave et al. 2018).
-
Step-1: Identification of the type of device followed by suitable addition of this device in one of the classes. This is followed by selection of the suitable evaluation procedure.
-
Step-2: Implementation of the quality management system.
-
Step-3: Preparation of a file that presents a vital legal requirement along with other appropriate directive compliance.
-
Step-4: An authorized representative is then elected in Europe. The name and address of that representative should be clearly mentioned on the medical device label.
-
Step-5: Europe’s declaration of conformity is being prepared.
-
Step-6: Hiring of notified body is required that will judicially examine the manufacturer’s quality management. Afterwards, it is designed as per the requirements, and eventually, the filing of dossier is done.
-
Step-7: After verification of the aforementioned requirements, the manufacturer is issued with the European CE certificate.
-
Step-8: CE is printed on the medical device, and the device is ready to be marketed legally (U.S. Food and Drug Administration 2020d).
Reporting of medical device
In accordance with the European medical device vigilance system, any adverse events related to a medical device must be reported by the manufacturer or European authorized representative (Wright and Datlof 2010). MEDDEV 2.12-1rev.6 defines incident as a malfunction in the performance of a medical device along with any inadequacy in labeling that may have resulted in the patient’s death or serious health problems. It was released in January 2013 and provides market surveillance recommendations for medical devices. Even with the implementation of the new EU MDR, it serves as a fundamental guideline document for reporting (Oriel STAT A Matrix 2020).
Medical device related reporting in Europe is mainly done by manufacturers to the National Competent Authority (NCA), whereas healthcare professionals report the incidents to both the NCA and to the manufacturers. A manufacturer is required to report a serious case within 2 calendar days and no later than that. When a manufacturer develops a connection between a medical device and an incidental death or any type of health worsening, the information should be notified within 10 days. Any other incident, which is considered to be non-serious should be reported within 30 calendar days (Oriel STAT A Matrix 2020).
China
In China, a device must be listed with the SFDA (State Food and Drug Administration) (now known as China Food and Drug Administration (CFDA)) before selling the same in the market. In China, 2 regulations are being followed: Measures for Administration of Medical Device Registration (2004) and Regulation for the Supervision and Administration of Medical Devices (2000). Earlier, registration of medical devices was valid for only 4 years. Now, it is valid for up to 5 years, and this is only necessary for Class-2 and Class-3 devices as they are considered to be having higher risks. While Class 1 devices are not required to be registered but they are mandatory to be filled.
Now, China’s National Medical Product Administration (NMPA) has expanded its registration of medical device pilot project. This pilot project previously began in a free trade zone, and now covers 21 provinces to help the NMPA to ensue better experience with the registration system of medical devices. The main reason of running this program is to establish an advanced medical device industry in China (Taylor 2019). The pilot project can improvise the usage of resources by enabling effective outsourcing by increasing the usage of the quality management system. Therefore, if a medical device manufacturing company wants to participate in a pilot project, then it must possess operations in one of the provinces and must also have few of the listed capabilities. The NMPA requires applicants to have full-time staff members who possess experience in post-marketing, regulatory bodies/affairs, and quality management system. Moreover, the staff members should be prepared to take responsibility for safety and quality of medical devices. In addition, the NMPA also wants the device lifecycle (i.e., from research and development to materiovigilance) to be monitored and traced properly (Taylor 2019).
If the medical device is not manufactured in China, then the company must first submit medical device samples to the NMPA for analysis. Class-2 and Class-3 devices need to be submitted along with their records indicating the evidence that those devices are already approved in the country where they have been manufactured. Apart from this, all the information related to devices, i.e., packaging and labeling, should also be translated in Mandarin. Lastly, all the foreign manufacturers are required to submit an additional data of clinical trials during the registration of Class-2 and 3 medical devices (Taylor 2019). Manufacturers from overseas might also require a Chinese-based agent to register their products that are manufactured outside China. The role of an agent is to provide technical services and maintenance support, management of adverse events, and regulation of clinical trials.
Apart from registration, some medical devices might also require Chinese Compulsory Certification (CCC). The CCC mark is controlled by the administration of supervision, quality, inspection, and quarantine which is the Chinese Quality and Quarantine Authority (AQSIQ).
Approval process of medical devices in China
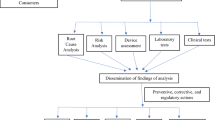
Various steps that are required to approve a medical device in China are shown in Figure 1 (U.S. Food and Drug Administration 2020d).
Reporting of medical devices
The CFDA oversees China’s post-approval surveillance system, which is carried out at regional levels by the department of health. The fact that this surveillance system works in tandem with the central approach is one of its distinguishing features (Kramer et al. 2014). When an adverse event related to medical device occurs, regulatory authorities and health department will act as first liners. Although the responsibility of collecting adverse event reports and to report them timely to regulatory authorities is of the Ministry of Health (MOH) and CFDA. The places in China without a provisional structure have their regional departments to serve with the same role as that of CFDA and MOH.
The CFDA’s National Centre for ADR Monitoring is in charge of collecting and analyzing adverse event reports from all regions and provinces. Every region, as well as provinces, has an ADR institution with better data access than the national ADR center; however, the ADR institutions are less capable analytically.
Injury reports must be filed to local institutions of monitoring in 15 days. As a result, it is up to these institutions to report death-related reports to National Centre for ADR. The submission of reports to the Ministry of Health and the Canadian Food and Drug Administration (CFDA) is considered complete now. Once per quarter, all the injury related reports must be only submitted to MOH and the CFDA (Pharma to Market 2020). However, all distributors, manufacturers of medical devices can bypass the step of submitting reports to the regional institutions first and can directly submit them to the national level authorities. However, they should notify the regional institutions as well. By the end of January each year, producers of Class-2 and 3 devices submit adverse event reports for the previous year to local institutions of monitoring. Then, the institutions will forward the reports to MOH and the CFDA by the end of March the same year.
On the 3rd of April 2020, the China NMPA had released adverse events reporting guidance for medical devices. The requirements that were decided in decisions on medical equipment adverse tracking and re-evaluation were included in the guidelines. These were issued so as to improvise the medical device monitoring system and to control the risk associated in post-marketing of medical devices (Pharma to Market 2020). The purpose of these guidelines was to set up protocols for a monitoring system that included department designation, emergency care in the case of a serious event, and device management.
In May 2020, an updated document was published that contained guidelines on adverse event monitoring for medical devices, and it comprised all the new regulations that were being made in this document. Table 4 comprises the new regulations that were included in document (Qual Tech 2020).
Japan
In Japan, medical device regulation is a hybrid of European and American regulatory methods. The Pharmaceutical Medical Device Act (PMDA) oversees approving and reviewing medical device processes. The act of effectiveness, safety, and quality of medical equipment, pharmaceuticals, cosmetics, and cell therapy products is also known as this act (Pacific Bridge Medical 2018). This Act impediments all the characteristics of registration of Japanese medical products, including the certification processes, quality assurance systems, and licensing. The PMD act came to effect on 25 November 2014, and it replaced the erstwhile Pharmaceutical Affairs Law (PAL) (Pacific Bridge Medical 2018). Some of the significant features of this regulation are:
-
All the medical software programs are regulated independently.
-
It is important for the manufacturers to get registered first.
-
Whole of the quality management system (QMS) is streamlined. The inspection of QMS is directed on marketing authorization holder.
The medical devices that fall in the category of Class-1 are considered to be of extremely low risk, and this class of medical devices requires submission of a marketing requirement known as “Todokeda,” which states that, certification for approval of devices is not needed. Whereas Class-2 devices along with Class-3 should have compliances that are directly interrelated to the standards and norms that are mandatory for agreement certification. The term “Ninsho” refers to a medical device application that will be submitted. The registered authority, who are suggested by the Ministry of Health, Labor and Welfare (MHLW), will assess this. The PMDA conducts a review evaluation of Class-2 and Class-4 devices, and the MHLW grants permission. Submission applications for these medical devices are termed as “Shonin.”
On 31 July 2017, MHLW proposed a new regulatory framework scheme that is known as “fast-break” scheme to expedite the patient accessibility for new medical devices. This scheme was made to collect some organized data that is necessary for the approval of devices in Japan (Dave et al. 2018). This scheme is only available for novel medical devices, and they should fulfill the following requirements:
-
No alternative medical device should be there until and unless there is an acceptable probability that it will be of greater efficacy, safety as that of the one which is already present.
-
The disease for which the new medical device will be used is either a serious one or should be life threatening.
-
Clinical evidence should be present in support of medical devices.
-
Post-marketing commitment with a suitable collection of rigorous real-world evidence.
-
A proper justification should be provided if new potential clinical trials are not being conducted.
Figure 2 shows the comparison between the “fast-break” scheme process and the traditional approval process. The figure evidently specifies that additional clinical information is required in traditional approval, whereas “fast-break” scheme requires less data to approve new medical devices.
Comparison of medical device approval process in Japan (U.S. Food and Drug Administration 2020d)
Reporting of medical devices
In Japan, as soon as an adverse event occurs, it is captured by the MAH. Then, within 15 days, the MAH reports AE15, i.e., an ADR that caused death or any serious health damage to the patient which is not listed elsewhere. Any foreign death event or serious case that is already listed is denoted as AE30, and it is reported within 30 days by the MAH (Handa et al. 2015).
Australia
In Australia, the Therapeutic Goods Act (TGA) established a legal framework for coherent regulations over goods and devices, used in illness diagnosis, prevention, and treatment nationally in 1989. In 2002, Australia accepted the GHTF framework, along with the key principles, to promote national-level uniformity in medical device regulatory systems and to improve the safety and effectiveness of medical devices. Being a part of the GHTF, Australia also follows the harmonized definition for medical devices being proposed. TGA, being the regulatory agency, has excluded few devices (tampons, hospital, and household disinfectants) from the proposed definition.
Reporting of medical devices
TGA has classified the medical devices into 4 classes:
-
Class I—low risk,
-
Class II a—low-medium risk,
-
Class II b—medium-high risk and,
-
Class III—high risk.
Reporting of these devices is done accordingly by the manufacturers as well as the sponsors to the TGA in Australia. For reporting, online medical device reporting form is provided by the TGA. The reporting of devices is as follows:
-
The sponsor or manufacturer must notify all the serious reports, i.e., death cases to the TGA in 10 days in total.
-
The sponsor or manufacture shall report a case on form MDIR01.
-
Events that are non-serious are supposed to be reported within 30 calendar days.
-
The one that requires prompt remedial actions should be reported within 48 h.
Once the product is being manufactured, and due to its risks, if the reporting is being done, then the record of these reports should be maintained by the TGA for up to 5 years. The record should consist of the full-fledged history of all the batches, ingredients used, and the risks caused by the compound. The record of reports received regarding the problem of the device should be maintained also by the sponsor (Gupta et al. 2010).
Canada
Canada is considered as a well-established and a profitable market for medical devices at global level. It comprises one-fifth population of Brazil but still tends to spend maximum on healthcare every year (RAMS 2019). The regulating authority for medical devices in Canada is “Health Canada.” Under the Food and Drug Act, Health Canada regulates the effectiveness as well as the safety of medical devices that are marketed in Canada. Regulation is done by a combination of compliance, monitoring, review of devices at both pre-marketing and post-marketing phases. During the pre-marketing phase, the regulatory authority regulates manufacturers, distributors, and importers by 2 licensing regimes, i.e., licensing of medical devices along with licensing of establishments. Before issuing any license to the company, Health Canada thoroughly evaluates the information that is being provided by the manufacturers about the devices. Generally, the information provided to the manufacturer is in regard to the medical device’s risk. If a high-risk device has been modified, then the authority authorizes the change. As a result, the Health Canada reviews the application of license for both new and modified devices. Whereas, in case of post-marketing, it is impossible to predict all the deformities due to medical devices. To work upon this, Health Canada along with the industries thoroughly monitor it and assess the safety of the medical devices, to protect the health of their citizens. Health Canada receives the reports of all the deformities by manufacturer and consumers. The authority assesses the severity and acts accordingly (RAMS 2019).
Canadian citizens usually rely on a particular range of medical devices that could be re-used to diagnose, treat a disease, and prevent a disease and other conditions. These devices might exhibit some adverse reactions, too. For this, the regulatory authority has divided the medical devices as lowest, low, moderate, and high-risk medical devices. The reporting of these medical devices is also done in accordance with the category it belongs to. Any adverse event caused by the medical device is reported by the consumer or the sponsor by completing the mandatory medical device reporting form (for industries) and consumer medical device report form (for consumers). A serious case or a death case is reported to the Health Canada within 10 calendar days. Whereas a non-serious case is to be reported within 30 calendar days to Health Canada (RAMS 2019).
India
There was previously no system in place for recording adverse outcomes related to medical instruments, and the Indian Drugs and Cosmetic Act was used to regulate them. Later, with a significant increase in the number of cases of hospitalization and death caused by poor quality devices, such as cardiac stents and faulty hip implants, Indian health ministry took stringent action to reduce the ADRs related to these devices. The health ministry permitted Indian Pharmacopoeia Commission (IPC) to serve as the National Coordination Center (NCC) for the creation of a materiovigilance program in July 2015 (Shukla et al. 2020; Indian Pharmacopoeia Commission 2018). The National Health System Resource Center (NHSRC), New Delhi was appointed as a technical support partner and in Thiruvananthapuram, Sree Chitra Tirunal Institute for Medical Science and Technology (SCTIMST) acted as the National Collaborating Centre (IPC 2018). The Central Drugs Standard Control Organization (CDSCO) in New Delhi supported the Materiovigilance Program of India (MvPI) as a national regulator. The CDSCO, which is part of the Ministry of Health’s Directorate General of Health Services, is responsible for approving the labeling, import, export, and sale of medical devices (Shukla et al. 2020). Later in 2017, medical device rules were issued by the Government of India for the regulation of medical devices in use across the nation (Bhave 2018), and the rules came into effect on 1 January 2018.
MvPI’s main aim was to compile data based on adverse events caused by medical devices. The data must be congregated scientifically and systematically to scrutinize them to aid in regulatory recommendations and decisions (Kumar et al. 2016). This is done to make safer use of medical devices by using data generated from India. Apart from this, it aims to spread awareness among the healthcare professionals about the vital role that the Medical Device Associated Adverse Events (MDAE) play in our society, as well as to assess and manage the benefit-risk ratio of medical equipment. It also generates autonomous and fact-based recommendations for the safe usage of medical devices, which it subsequently disseminates to all relevant stakeholders.
In addition, MvPI aims to set vigilance system in harmony with GHTF members as:
-
It encourages convergence at global level in the regulatory system evolution for devices to preserve all the rights of contributing members in order to address public health protection (World Health Organization 2020a). India collaborates with the GHTF as (World Health Organization 2020b) this will facilitate access to information on some main regulatory systems for medical devices.
-
It will help in adopting a single nomenclature for medical devices.
-
Approval of devices will be from highly regulated markets.
-
There will be a vast network for post-marketing vigilance.
The medical equipment including in vitro devices are classed according to the risk characteristics that are described in Table 1 and also based on health hazard. Medical device hazards are divided into 3 types as below (Singh and Associates 2018).
-
Type-1: There is a good chance that using the recall device will have catastrophic health repercussions, including death.
-
Type-2: A situation in which utilization of medical device may cause temporary adverse health consequences.
-
Type-3: A situation in which usage of recall medical device does not lead to any adverse health consequences. Therefore, such hazard-based classification system can be formulated in the countries which are intended to start post-marketing surveillance programs for medical devices (Singh and Associates 2018).
In vitro Diagnostics (IVD) and medical devices that are presently synchronized in India include drug eluting stents, cardiac stents, orthopedic implants, intravenous cannulas, ablation devices, surgical dressings, umbilical tapes, blood sera, ligatures, scalp vein sets, hypodermic needles, internal prosthetic replacements, condoms, tubal rings, heart valves, staplers, hepatitis B surface antigens and hepatitis C, perfusion sets, and human immunodeficiency virus in vitro diagnosis test (Rehni et al. 2010).
In India, there is a detailed process of registration and regulatory approval of the above medical devices and in vitro diagnostics for manufacturing and importing them for sales and marketing. To begin the regulatory approval process, an applicant must bundle several medical devices with similar technologies or uses and submit them as a sole application. The medical device alliance was formed with the goal of submitting a sole request for a license to manufacture/import medical equipment in the future. These devices can be categorized as follows (Kumar et al. 2016):
-
Single—It is a medical device that does not fulfill the standards of family, IVD test kit, IVD group, and is sold as an individually packaged entity. It might be retailed in an assortment of bundle sizes. Example, condom package of 3 or 10.
-
Family—It is an assembly of medical devices in which individual device is from the single license owner, which has a common use, the same design, and is from the similar risk classification class and possesses similar process of manufacturing, for example, condoms with different texture, size, and color but are mass-produced from a common material having the same developing process. Such things are licensed under the family category.
-
System—These devices comprise a system where they belong to a similar license holder and are envisioned to be used in association for a mutual purpose and are retailed under a common proprietary name. Example—a system encompassing a test strip for monitoring glucose, glucose meter, solutions (linearity and central). They all can be qualified as single “system.”
-
In vitro diagnostic cluster—It comprises several in vitro diagnostic articles and reagents which fall under one license owner, are retailed under a common proprietary name, have a communal procedure, and are compatible enough when used as a testing kit.
-
In vitro diagnostic test kit—This device consists of articles or reagents from same licensor, is primarily meant to be used in conjunction to achieve a certain goal, is compatible to be used as a kit, and is supplied under a single proprietary test. Example, an ELISA test kit for the Human Immunodeficiency Virus (HIV) may include calibrators, controls, and washing buffers. All of them together are used to detect HIV and can thus be licensed as single testing kit.
-
Group—Two or more equipment collected, mainly provided in a single bundle by a licensor and are also retailed under a same/single proprietary group tag and used for a same purpose. Example—a kit used for first aid usually consists of devices that comprise gauze, drapes, bandage, and thermometers. These are gathered as single package, and this package is approved as a group (Singh and Associates 2018).
Apart from grouping the medical devices, their labeling also plays a vital role. Labeling instructions are written on the label, on the outer cover and on the shelf pack of the medical devices using ineffaceable ink. In case of small size medical devices, information required for product safety and identification are only printed. Some may need some special instructions.
During the export of medical devices, labeling requirements are exempted to follow definite requirements of the law of the nation where the device is being shipped. Some particulars like name of device, batch number, date of expiry wherever required, shall be printed with regard to the law of nation where device is being shipped. Also, a device being permitted for manufacturing, import, or sales shall abide inimitable device recognition and production identifier from 1 January 2022 (Singh and Associates 2018).
India’s approval process of medical devices
In India, medical devices usually require 6 steps for registration and are discussed below (Sanjana et al. 2016).
Determining whether a product requires registration
The first stage is to determine whether the medical equipment needs to be registered. Only medical devices that have already been listed in the Drugs and Cosmetic Act of 1940 are eligible for registration. Presently, only 22 medical devices are present in the Act. The devices that come under this are listed below:
-
Disposable hypodermic syringes
-
Blood grouping sera
-
Disposable perfusion sets
-
Ligatures, sutures, and staplers
-
Diagnostic testing kit for HIV (In vitro)
-
Intra uterine devices
-
Cardiac stents
-
Condoms
-
Drug eluting stents
-
Tubal rings
-
Catheters
-
Surgical dressings
-
Intra ocular lenses
-
Umbilical tapes
-
Bone cement
-
Heart valve
-
Orthopedic implants
-
Internal prosthetic replacements
-
Spinal needles
Devices that are not on the above list need to be registered with the CDSCO. This is usually only used in situations where the manufacturer is unsure of the regulatory status of its device in India. The Drug Controller General of India (DCGI) will analyze it and provide a no objection certificate in this situation. After reviewing the device’s details, the CDSCO will grant it regulatory approval.
Appointment of an authorized Indian agent (Sanjana et al. 2016)
An Indian agent is usually appointed in the case of a foreign manufacturer. The agent serves as a coordinator between both the manufacturer and the CDSCO, assisting with device registration and approval. A drug license in form 20B and 21B is held by the approved native agent.
Submission of regulatory dossier under form 40 (Sanjana et al. 2016)
To initiate the process of registration, the following documents must be prepared along with the dossier:
-
Form 40
-
Power of attorney
-
ISO 13485 certificate
-
CE design certificate
-
Free sale certificate
-
Other regulatory approvals
-
TR6 challan
-
Schedule D (I)
-
Full quality assurance certificate
-
Declaration of conformity
-
Certificate of marketability from GHTF countries
-
PMS report
-
Device master file
-
Plant master file
Form 40 must be correctly completed, signed, and validated by an Indian representative (in case of a foreigner manufacturer). After that, a medical device approval application to the DCGI must be submitted. If the device maker is new in the country, they must submit Form 45, a new drug licensing application, in addition to Form 40. The time taken to register a device is usually between 6 and 9 months.
Obtaining import license in Form 10
For the grant of an import license, the distributor may submit Form 10 to the CDSCO immediately. Application is made in Form 8, and Form 9 can be used to made application, and it provides the certificate number of the registration.
The application is typically processed in 4 to 12 weeks. If all of the information is correct and complete, the license would be granted within 3 months. It will be valid for 3 years unless the authority cancels or suspends it.
Obtaining registration certificate in Form 41
After the application has been submitted, it would be pre-screened using the CDSCO’s checklist. If the information is correct and full, the authorities will provide a certificate of registration using Form 41 within 9 months. Unless it is canceled or suspended, the certificate of registration is valid for 3 years.
Marketing in India
The product can be marketed in India when this registration is complete, and the license is provided. Any change, adverse events, or recall of the same device that is being marketed in India must be reported to the authorized Indian representative (Sanjana et al. 2016).
Reporting of adverse events from medical devices
Reporting of adverse events associated with medical devices is done by various mediums. Any serious, non-serious, frequent, rare, known, or unknown events can be reported, although it should have relevance with the ADR. Currently, India’s materiovigilance system has 26 dedicated monitoring centers for adverse outcome related to medical device that report incidents on a voluntary basis (Shukla et al. 2020). Additionally, around 270 adverse reaction monitoring centers created under the pharmacovigilance program in India have requested to submit the adverse events related to medical devices. Therefore, once any commission enrolls a hospital or a medical institute as a monitoring center, the available research associate will start collecting and sending the adverse events related to medical devices to the commission. The research associate’s responsibility will be to liaise between the patient and consumer, record, validate the reported incident/s and report the case to commission, and inform the manufacturer of the medical device. There is a MDAE (Medical Device Adverse Event) reporting form in which reporting of any medical device associated adverse events may be reported (Kalaiselvan et al. 2015). This form consists of initial description, details of the adverse event occurred, and associated risks to the patient. It can be downloaded from the website of the IPC. Adverse events can also be reported by PvPI (Pharmacovigilance Program of India) helpline number (Kalaiselvan et al. 2014). The healthcare professionals, patients can duly report the MDAE form to either NCC or SCTIMST. Any suspected serious adverse events must be reported to CDSCO and commission within 15 calendar days from the occurring of an event. After filling the MDAE form, it can be directly submitted to either the SCTIMST or the NCC. At the commission, each report that is being received is first segregated into initial, final, and a follow-up report. The reports are allotted with a unique reference number. Until a conclusion is made, the commission seeks additional information from the patient or reporter. These reports are evaluated by professionally trained staff members present at the panel to ensure that the data is comprehensive, valid, and of high quality. They are further evaluated by external subject expert group, and then it is forwarded to the core technical committee to prepare any necessary recommendations. The recommendations being made are then forwarded to the CDSCO for any regulatory action. After forwarding it to CDSCO, it is then forwarded to WHO-UMC (Uppsala Monitoring Center), where its entry is done in “vigiflow.” If the data is determined to be missing, the report is forwarded to the reporter or monitoring center, along with any relevant comments, so it can be completed and amended accordingly. The confidentiality of patients is strictly safeguarded while examining and evaluating case reports.
Table 5 shows the comparison of medical device regulations and the assigned timelines for various countries across the world.
Challenges in regulating medical devices
Mutual control is the foundation of the relationship between policy and creativity. Effective regulations clearly control the mechanism of innovation in a given area. Technical developments and improvements, on the other hand, have significant effects on regulation. This relationship must be seen as an effective tool in reforming the existing regulations. The adjustment of laws thoroughly affects the changes in the technological, social, and economic circumstances affecting it.
When it comes to medical devices and the regulatory changes that are now being debated, the focus should be on ensuring improved patient safety. In the context of determining compliance, this also reflects increased economic pressure on medical equipment manufacturers. The question now is whether such reforms will put a significant strain on small and midsize enterprises (which are indeed the primary innovators in the areas of pharmaceutical devices), to the point where development will be limited, or whether they will end up serving as a strong catalyst for more innovation, as several other examples of well-enforced legislation have done. Transparent innovation is a popular trend in a variety of industries, including the medical device industry. Open innovations have become the dominant model for connecting developing technologies and markets. In the field of medical equipment, the value of open innovations is proved, for example, by the fact that patients will provide impulses for long-term progress (Gupta 2015).
Another key difficulty is the sophistication of the motionless systems in this industry, which necessitates maximum productivity in all processes. User-led inventions, which are based on user ideas, in this example from patients and healthcare providers, are a key source of innovation. This type of technical strain, according to Bernstein and Singh (2006), is one of the grounds why businesses in this industry still require a completer and more integrated model of innovation processes. The Open Innovation Platform may be useful in providing a detailed perspective of how high-tech small companies (HTSFs) develop in healthcare. Several research studies and data show that demand for medical equipment will never plateau since it rises irrevocably in unison with improvements in other businesses and medical procedures, and these trends clearly suggest that successful solutions to this problem are required. Open invention frameworks add value by including numerous additional innovations through their integration into a range of external principles (Peter et al. 2020). As a result, technological potential is being used, with the promise of economic value growth. To streamline available procedures, increase performance, and maximize outcomes in every area, all organizational units must work together. This includes promoting a productive teamwork culture, openness to new knowledge, expertise exchange, and the desire for change, innovation, and new inventions in the workplace. The fact that the new guidelines are developed in the benefit of patient protection is, first and foremost, an issue that has the potential to qualitatively transform organizational growth. From the other side, it is obvious that changing the current regulations will increase an organization’s performance. With tens of thousands of crowns at stake, increasing the risks often suggests a larger need for testing and supervision (Peter et al. 2020).
Often very large expenses are incurred during the lifetime of a commodity in business danger class III. The most expensive item, clinical testing, would need to be often replicated with such medical products. The truth is that, in the past decade, many firms have debated how to address this transition, and this has sometimes been a divergent basis of prospect, particularly for small and midsize companies. The selection of budget-management alternatives involves modifying the medical equipment to drop into a lesser risk class to wholly alter the progression and developing factors (Peiffer 2019).
Overall, the area of legislation, science, and healthcare is a highly responsive area, with numerous research fields and human accomplishments overlapping, such as law, economics, and services related to health policies. For creativity and competition in this field, the partnership between developers of medical devices and national regulatory agencies is crucial. While, on one hand, such regulations suggest a decrease in action, however, on the other side, they provide an enticement for new practices to nurture and an opportunity for novelty. Compared to standardized products, the method of accepting new medical equipment is usually more troublesome.
The more creative new devices are, the harder it gets to establish their safety, evaluate their usability, assess their potential value to patients, and consider a slew of other factors. At the same time, the oppressive effect of legislation may be reduced under the principle of free innovation (Peter et al. 2020).
To effectively make the production of medical devices quicker and easier, open innovation may be used effectively. The stringent safety and dependability standards for medical equipment often require the exchange of integrative knowledge, although it is nearly difficult for any company to hold the scientific resources sufficient to obtain altogether core capabilities. If the information produced by scientists is more broadly disseminated through scientific fields, improved and cheaper medical instruments could be distributed more efficiently, improving the quality of life (Peter et al. 2020; Peiffer 2019).
Quality is indeed an ever-growing issue in the area of medical equipment/devices, pharmaceuticals, and medical diagnostics. This significantly affects negatively on manufactures along with the patients and the one who have invested in it, the sponsors. Reduction in the quality of medical devices will automatically result in numerous adverse events that include serious health injuries, death, prolonged hospitalization, congenital disability, and other forms of disabilities. To reduce this, reporting of adverse event plays a critical role in improving the quality and safety of medical devices. The major challenge being faced by all the countries in reporting adverse events of medical devices is that such events are being under reported. Regulations and guidelines are imposed by the regulatory authorities for manufacturers to manage the reporting process. Many companies fail to invest in this field due to which they lack quality in reporting adverse events to regulatory bodies, and thus, it creates a great impact on quality as well as on the safety of medical devices and patients (Med Device Online 2020). Additionally, if the medical device reports are submitted by manufacturers to regulatory authorities, they are often either misclassified or use ambiguous language that makes it impossible for the regulatory authorities to understand and approve it. When a MDR is submitted by industries, they should properly mention whether death or injury has happened. They often classify it as a mere malfunction even when a death has occurred, which leads to obscuring the true results of the event.
The main reasons of under-reporting adverse events are lack of knowledge, lack of ADR monitoring centers, and lack of investment by companies in reporting. People are still not aware of what reporting is and how it is been done, and most of the times they tend to ignore all those adverse events that occur among users. Not only patients, but many healthcare professionals, especially in less regulated or non-regulated countries are unaware of reporting an AE (Device Events 2020). Moreover, in many places, ADR monitoring centers are not located, and this leads to a lack in reporting of ADRs.
Conclusion and future perspectives
In the past few years, the usage of medical devices is seen to be very recurrent by the healthcare professionals globally. Materiovigilance programs by various countries are indeed good initiatives to ensure safety of medical devices being used. Its emphatic implementation has covered the safety of medical devices along with the well-being of patients. Medical device regulation plays a vital role in ensuring efficacy, safety, and performance of the device so that it is made accessible in the marketplace for refining community health. A safer and effective device will automatically lift the faith and confidence of customers over the device. As discussed in the review, devices are classified based on their risks, and thus, accordingly their reporting and regulation need to be carried out.
Some of the authors have already produced some fantastic work in the past. Chauhan et al. (2019) examined the risks involved with the use of various types of medical devices, as well as the necessity for a materiovigilance program, with a focus on medical device adverse event reporting. In addition, few papers (Meher 2018; Deshwal et al. 2020; Hoda et al. 2020) have summarized the concept and viewpoint of materiovigilance in India solely. Furthermore, Manu and Anand (2021) compared the medical device laws in India to those in the European Union. Mirel et al. (2014) conducted a study to see if Romania is harmonizing its medical device monitoring framework with European Directives. All the research described earlier in this thread lacked a global comparison, which is a vital prerequisite at this time to harmonize medical device laws around the world. Our article can be used as a comprehensive global guide to medical devices, which include the history of medical devices, their classification, marketing status, problems, and current regulatory issues encountered by developed countries around the world, with a focus on the regulatory position in India.
As of now, in some countries, the medical device adverse event reporting form is only available in English. But in future, this might be available in various languages. Especially, this problem is faced in a country like India, where there are diverse languages in use. So, to enhance the participation of patients in reporting, it should be available in all the spoken languages. In coming years, the focus will be shifted from cost to value, and this will not be just about the device. By 2030, medical devices will play an active role globally in bringing value by connecting with the patients and customers. This will probably require a change from treatment and cure to prevention by smart solutions as well as services that will bring down the cost and will improve outcomes.
Medical devices are subject to stringent legislation to ensure patient safety and to reduce, as often as possible, the health hazards involved with the use of goods that are also technologically advanced. The requirements for classifying the risk are grounded on the expected intent and usage of the medical equipment and ensuring that a greater degree of control is extended to high-risk devices, whereas comparatively low-risk devices are subject only to risk-proportionate regulations. Although manufacturers must identify their products within the required risk level, regulatory bodies function as a mediator in interpreting the conditions imposed on a specific product. Global regulators and national legislatures influence nearly all facets of the production and manufacturing of medical devices; from development and design, preclinical, and national legislation process. The stakeholders are expected to consider the macroeconomic context with variables in terms of supply and usage while determining the degree of venture effectiveness and returns on investment in modernization in the medical devices market. The inclusion of the medical product into the proper risk class may assist the provider in defining & setting up discrete company procedures or in planning for any future restrictions, laws, and regulations that need to be followed. All such policies will optimize the process of design and production and help create an economic success of the business along with a competitive growth. At the beginning of the design and production of a medical product, the best strategy would be to demonstrate the fiscal budget of putting the device on the marketplace.
There is always room to improve patient and user safety by reducing the occurrence of adverse events, finding solutions for improving the use and efficiency of medical devices, and establishing a nationwide system to monitor patient safety. Like medicinal products, there is a requirement to scrutinize the benefit-risk ratio of the medical devices used and to converse safety data on the usage of medical devices to numerous stakeholders to reduce risks. Likewise, there should be a nationwide center of excellence for activities related to materiovigilance which can track and monitor the safety and efficiency of these medical equipment.
For a materiovigilance program to succeed, the manufacturers, regulatory authorities, healthcare professionals, and patients/caregivers need to work in close collaboration. Appropriate reporting of any device-related adverse events is crucial to the materiovigilance program and for establishing patient safety. The continuous collection of adverse reactions and signal detection process will help generate data about the risks and the benefits of the devices, and therefore, a benefit-risk ratio will be established. Since, materiovigilance is an ongoing process, the data generated over the years will help the healthcare professionals and patients make better informed decisions. The prescribers will have a better knowledge and understanding of the expected adverse reactions, thus, preventing repetition of such occurrences. This will reduce the burden of device-related morbidity and mortality on the healthcare system. The economic burden on the patients will be reduced as the adverse reaction will be mitigated efficiently.
The pool of data generated over the years will be helpful for the medical device manufacturers in making the devices safer and in the development of other related medical devices. As the manufacturers start to develop better medical devices, the patients will have more treatment choices. They will have greater sense of peace as they will be better informed about the devices they use. As a result, the patient compliance will increase, thus, improving the patient health and public health.
The communications between the regulatory authorities of different regions will have a major role to play in the success of materiovigilance. To strengthen the evidence on the risks and benefits, the regulatory authorities of different regions of the world will need to seamlessly communicate the information regarding the safety and efficacy of medical devices to strengthen evidence related to the benefit-risk of medical devices. With the streamlined exchange and collection of information, the marketing authorization holders will be able to develop better risk mitigation strategies to efficiently manage the risks of the devices. As more information becomes available, the regulatory authorities will be able to make better decision regarding the use of medical devices.
The future holds a lot for the medical device industry as medical device companies found different opportunities even during COVID’s early economic downturn. The biggest impact of the pandemic on the MedTech business, according to many industry insiders, has been the acceleration of trends that were already well advanced in previous years. Changes in working patterns and consumer behavior have facilitated the demand for remote technologies, and the interaction between patients and physicians has evolved as well. The medical device market is more than equipped to accommodate this demand for user-friendly diagnostics and monitoring equipment, as the COVID-19 epidemic proved. Rapid improvements in Artificial Intelligence, remote monitoring, device connectivity, and data collecting have allowed MedTech businesses to appropriately respond to the need for crucial products like personal protective equipment (PPE) and ventilators. The sector has played a key role in relieving pressure on overburdened healthcare systems by being able to quickly scale up R&D and manufacturing operations.
The sector’s main problem is now to figure out how to best use data to improve medical outcomes while still protecting patient privacy. Medical device makers and regulators must work together to develop infrastructure with agreed-upon expectations and boundaries if this aim is to be achieved.
Governments, too, have a significant role to play. The government of the UK, for example, has introduced incentives (such as the elimination of VAT and import levies on critical medical equipment) to help the country’s medical device sector throughout the pandemic. Beyond COVID, the UK aspires to be a global leader in medical device technology, with plans to invest tens of billions in the future years.
By 2025, the worldwide medical device business is anticipated to be worth $612.7 billion (£440.5 billion), with a 5.4% compound annual growth rate. We may expect substantial growth in product sectors such as wearable health technology, robotics nanotechnology, and extended reality gadgets, because of rising customer demand and technological innovation. Artificial intelligence is also allowing for the development of increasingly complex data-driven algorithms, such as autonomous diagnostics. Despite recent setbacks, medical device firms of all sizes have plenty of opportunity.
References
Anson P (2018) Faulty medical devices blamed for thousands of deaths. Pain News Network. https://www.painnewsnetwork.org/stories/2018/11/26/faulty-medical-devices-blamed-for-thousands-of-deaths#:~:text=Jim%20Taft%E2%80%99s%20doctor%20told%20him%20a%20spinal%20cord,sleeping%20and%20fell%20down%20a%20flight%20of%20stairs. Accessed 5 January 2021
Assaad M, Degheim G, Machado C (2016) The runaway defibrillator… A case of an implantable cardioverter-defibrillator that failed communication and deactivation with a magnet. HeartRhythm Case Rep 2(1):40–42
Bernstein B, Singh PJ (2006) An integrated innovation process model based on practices of Australian biotechnology firms. Technovation 26(5-6):561–572
Bhatia I (2015) Fire in nursing home’s incubator; one infant dead. Times of India. https://timesofindia.indiatimes.com/city/meerut/Fire-in-nursing-homes-incubator-one-infant-dead/articleshow/48794392.cms. Accessed 5 January 2021
Bhave A (2018) Indian Regulatory Update: January-December 2017. Perspect Clin Res 9(1):48–50. https://doi.org/10.4103/picr.PICR_176_17
Chauhan PR, Zarreen AA, Iqubal MK (2019) Current status of materiovigilance globally—an utter overview with clinical case perusal. Int J Pharm Pharm Sci 11(10):1–8
Dave V, Yadav S, Gulati B, Gupta N, Yadav R (2018) Current scenario of regulation and monitoring of medical devices in global realms of world. Asian Hospital & Healthcare Management. https://www.asianhhm.com/technology-equipment/current-scenario-regulation-monitoring-medical-devices. Accessed 05 January 2021
Deshwal M, Nagpal M, Dhingra GA, Aggarwal G (2020) An updated review on materiovigilance for safe use of medical devices. International Journal of Drug Regulatory Affairs 8(4):5–13
Device Events (2020). Information transparency challenges. https://www.deviceevents.com/industry-challenges/. Accessed 22 December 2020
Gupta SK (2015) Medical device regulations: a current perspective. Journal of Young Pharmacists. 8(1):06–11. https://doi.org/10.5530/jyp.2016.1.3
Gupta P, Janodia MD, Jagadish PC, Udupa N (2010) Medical device vigilance systems: India, US, UK, and Australia. Medical Devices (Auckland, NZ);3:67.
Handa N, Ishii K, Matsui Y, Ando Y (2015) Reporting of cardiovascular medical device adverse events to pharmaceuticals and medical devices agency, Japan. EBioMedicine 2(9):1211–1216. https://doi.org/10.1016/j.ebiom.2015.07.011
Healthcare IT news (2018) Unsafe medical devices allowed into global markets harm patients, investigation reveals. https://www.healthcareitnews.com/news/emea/unsafe-medical-devices-allowed-global-markets-harm-patients-investigation-reveals. Accessed 4 January 2021
Hoda F, Verma R, Arshad M, Siddiqui AN, Khan MA, Akhtar M, Najmi AK (2020) Materiovigilance: concept, structure and emerging perspective for patient’s safety in India. Drug Research 70(09):429–436
Hutt PB, HuttII PB (1984) A history of government regulation of adulteration and misbranding of food. Food Drug Cosmetic Law Journal 39:2–73
India.com (2017) Amravati: four infants die as fire breaks out in incubator due to short circuit. https://www.india.com/news/india/amravati-four-infants-die-as-fire-breaks-out-in-incubator-due-to-short-circuit-2180029/. Accessed 5 January 2021
Indian Pharmacopeia Commission (2018), National Coordination Center MvPI, Ministry of Health and Family Welfare, Government of India; a guidance document for medical devices, draft version. Accessed 14 January 2021
Kalaiselvan V, Mishra P, Singh GN (2014) Helpline facility to assist reporting of adverse drug reactions in India. WHO South East Asia J Public Health 3:194. https://doi.org/10.4103/2224-3151.206737
Kalaiselvan V, Kumar P, Mishra P, Singh GN (2015) System of adverse drug reactions reporting: what, where, how and whom to report? Indian J Crit Care Med 19(9):564–566. https://doi.org/10.4103/0972-5229.164819
Kramer DB, Tan YT, Sato C, Kesselheim AS (2014) Ensuring medical device effectiveness and safety: a cross-national comparison of approaches to regulation. Food and Drug Law Journal 69(1):1–23
Kumar P, Kalaiselvan V, Kaur I, Thota P, Singh GN (2016) Materiovigilance programme of India (MVPI): a step towards patient safety for medical devices. Eur J Biomed Pharm Sci 12:497–501
Manu M, Anand G (2021) A review of medical device regulations in India, comparison with European Union and way-ahead. Perspect Clin Res. https://doi.org/10.4103/picr.PICR_222_20
Med Device Online (2020) Addressing the challenges of complaint handling, investigations, and adverse event reporting. https://www.meddeviceonline.com/doc/addressing-the-challenges-of-complaint-0002. Accessed 21 October 2021
Meher BR (2018) Materiovigilance: an Indian perspective. Perspect Clin Res 9(4):175–178
Mirel S, Colobatiu L, Fasniuc E, Boboia A, Gherman C, Mirel V, Muresan D (2014) Materiovigilance and medical devices. In: Vlad S., Ciupa R. (eds) International Conference on Advancements of Medicine and Health Care through Technology; 5th – 7th June 2014, Cluj-Napoca, Romania. IFMBE Proceedings, vol 44. Springer, Cham. https://doi.org/10.1007/978-3-319-07653-9_21
Oriel STAT A Matrix (2020) EU MDR vigilance reporting requirements and MEDDEV 2.12-1 Rev 8: what has changed? https://www.orielstat.com/blog/eu-mdr-ivdr-vigilance-reporting-requirements/. Accessed 22 September 2020
Pacific Bridge Medical (2018). Japan MHLW & PMDA medical device and pharmaceutical regulations. https://www.pacificbridgemedical.com/regulation/japan-medical-device-pharmaceutical-regulations/. Accessed 18 October 2020
Peiffer M (2019) Defective medical devices—how new european legislation is shaping German liability laws. Genre. https://www.genre.com/knowledge/publications/cmint19-1-en.html Accessed 20 January 2021
Peter L, Hajek L, Maresova P, Augustynek M, Penhaker M (2020) Medical devices: regulation, risk classification, and open innovation. Journal of Open Innovation: Technology, Market, and. Complexity 6(2):42
Pharma to Market (2020) China NMPA releases “Adverse event reporting guidance for medical device registrants”. https://www.pharmatomarket.com/china-nmpa-releases-adverse-event-reporting-guidance-for-medical-device-registrants/. Accessed 16 January 2021
Qual Tech (2020) China: NMPA published the update guidance of adverse event monitoring for medical device—May,2020. https://www.qualtechs.com/en-gb/article/393. Accessed 16 January 2021
Ramesh A (2019) Johnson and Johnson faulty hip implants, curse to the Indian patients. International Journal of Research and Analytical Reviews 6(1):5
RAMS (2019). Health Canada Regulatory Approval Process for Medical Devices. EMERGO by UL. https://www.emergobyul.com/resources/canada-process-chart. Accessed 16 January 2021
Rehni AK, Singh TG, Singh N, Arora S (2010) Tramadol-induced seizurogenic effect: a possible role of opioid-dependent histamine (H1) receptor activation-linked mechanism. Naunyn Schmiedebergs Arch Pharmacol 381(1):11–19. https://doi.org/10.1007/s00210-009-0476-y
Sanjana P, Kirti AH, Begum AS (2016) Medical devices and their approval procedure in India. International Journal of Drug Regulatory Affairs 4(3):19–29
Shukla S, Gupta M, Pandit S, Thomson M, Shivhare A, Kalaiselvan V, Singh GN (2020) Implementation of adverse event reporting for medical devices, India. Bulletin of the World Health Organization 98(3):206. https://www.who.int/bulletin/volumes/98/3/19-232785/en/. –211
Singh & Associates (2018) Materiovigilance Programme of India (MvPI) issues draft guidance on medical devices Mondaq. http://www.mondaq.com/india/life-sciences-biotechnology-nanotechnology/736918/materiovigilance-programme-of-india-mvpi-issues-draft-guidance-on-medical-devices. Accessed 22 February 2021
Taylor NP (2019) Asia regulatory roundup: China expands medical device registration pilot to cover multiple regions. RAPS. https://www.raps.org/news-and-articles/news-articles/2019/8/asia- . Accessed 22 February 2021
U.S. Food and Drug Administration (2018). https://www.fda.gov/industry/regulated-products/medical-device-overview. Accessed 22 February 2021
U.S. Food and Drug Administration (2019a). https://www.fda.gov/medical-devices/medical-device-recalls/abbott-formerly-st-jude-medical-inc-recalls-ellipse-implantable-cardioverter-defibrillators-due#:~:text=Abbott%20is%20recalling%20the%20Ellipse,wires%20to%20be%20partially%20exposed.&text=Of%20the%20devices%20recalled%20in,31%20devices%20have%20been%20implanted. Accessed 22 February 2021.
U.S. Food and Drug Administration (2019b). https://www.fda.gov/regulatory-information/search-fda-guidance-documents/humanitarian-device-exemption-hde-program. Accessed 22 February 2021.
U.S. Food and Drug Administration (2019c). https://www.fda.gov/medical-devices/premarket-submissions/humanitarian-device-exemption. Accessed 22 February 2021.
U.S. Food and Drug Administration (2020a). https://www.fda.gov/medical-devices/device-advice-comprehensive-regulatory-assistance/overview-device-regulation. Accessed 22 February 2021.
U.S. Food and Drug Administration (2020b). https://www.fda.gov/medical-devices/premarket-submissions/premarket-notification-510k#who. Accessed 22 February 2021.
U.S. Food and Drug Administration (2020c). Medical Device Reporting 21 CFR Part 803. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?CFRPart=803. Accessed 22 February 2021.
U.S. Food and Drug Administration (2020d). https://www.fda.gov/medical-devices/medical-device-safety/medical-device-reporting-mdr-how-report-medical-device-problems. Accessed 22 February 2021.
Weiss M, Mohr H (2018). NBC News. Available at: https://www.nbcnews.com/health/health-care/spinal-cord-stimulators-help-some-patients-injure-others-n940131. Accessed 22 February 2021.
World Health Organization (2020a). Medical device regulations: global overview and guiding principles. https://www.who.int/medical_devices/publications/en/MD_Regulations.pdf?ua=1. Accessed 22 February 2021.
World Health Organization (2020b). Medical devices. Available at: https://www.who.int/medical_devices/collaborations/force/en/. Accessed 22 February 2021.
Wright EA, Datlof SB (2010) Adverse event reporting in the EU and the US: similarities and differences. Journal of Medical Device Regulation 7(3):14–22
Yoon C, Nam KC, Lee YK, Kang Y, Choi SJ, Shin HM, Jang H, Kim JK, Kwon BS, Ishikawa H, Woo E (2019) Differences in perspectives of medical device adverse events: observational results in training program using virtual cases. Journal of Korean Medical Science 34(39):e255. https://doi.org/10.3346/jkms.2019.34.e255
Acknowledgements
I would like to express my deep gratitude towards Mr. Shubham Joshi for providing enthusiastic encouragement and helpful critiques of this review work. Also, I would like to extend my thanks to Mrs. Swati Gauniyal for the writing assistance to enhance the quality of this work.
Availability of data and materials
Not applicable.
Author information
Authors and Affiliations
Contributions
DJ, IS: methodology, data curation, and writing—original draft; SG: conceptualization, validation, supervision, and writing—review & editing; TGS: supervision and writing—review & editing; SD, AP, MG, BK, SV, GG, NKJ, PKG, PN: methodology; DKC, KD: review and editing; SKS: conceptualization, validation, supervision, and writing—review & editing.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Yes.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Philippe Garrigues
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights:
• Medical device regulation plays a vital role in ensuring efficacy, safety, and performance of medical devices.
• Materiovigilance is a study of incidents caused by medical devices.
• The principles, perspectives, and practices of materiovigilance in the USA, Europe, China, Japan, Australia, Canada, and India are being compared.
• Different countries possess different penalties for device failure.
• By the year 2030, medical devices will play an active role in bringing value by connecting with the patients and customers globally.
Rights and permissions
About this article
Cite this article
Joshi, ., Sharma, I., Gupta, S. et al. A global comparison of implementation and effectiveness of materiovigilance program: overview of regulations. Environ Sci Pollut Res 28, 59608–59629 (2021). https://doi.org/10.1007/s11356-021-16345-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-16345-5