Abstract
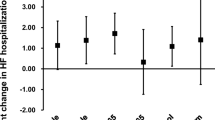
The cardiovascular impact of fine particles has caused great concern worldwide. However, evidences on the impact of fine particulate matter (PM2.5) on emergency department (ED) admissions for circulatory system disease in Northeast China is limited. We assessed the acute, lag, cumulative, and harvesting effects of PM2.5 on ED admissions for circulatory system diseases and their exposure-response relationship. A total of 26,168 ED admissions, including those for hypertension, ischemic heart disease (IHD), arrhythmia, heart failure (HF), and cerebrovascular events (CVE), were collected from the Shenyang Emergency Center from 1 January 2017 to 31 December 2018. The relationship between PM2.5 and ED admissions for circulatory system disease was estimated using a distributed lag non-linear model and a generalized additive quasi-Poisson model. We stratified the analyses by temperature. Air pollution was positively correlated with daily ED admissions for circulatory system disease or other cause-specific diseases under different lag structures. For every 10-μg/m3 increase in the PM2.5 concentration, the relative risk of daily ED admissions for circulatory system disease was 1.007 [95% confidence interval (CI), 1.001–1.013] in lag0, 1.007 (95%CI, 1.000–1.013) in lag1, and 1.011 (95%CI, 1.002–1.021) in lag03. A lag effect was found in IHD, a cumulative effect was found in CVE, and both lag and cumulative effects were found in hypertension and arrhythmia. A harvesting effect was observed in daily ED admissions for circulatory system disease and HF. We found no interaction between pollutants and temperature. We observed a monotonic and almost linear exposure-response relationship between PM2.5 and circulatory system disease with no threshold effect.PM2.5 contributes to obvious acute, lag, cumulative, and harvesting effects on circulatory system disease. PM2.5 was associated with the risk of daily ED admissions for circulatory system disease, hypertension, IHD, arrhythmia, HF, and CVE. Therefore, air quality management must be strengthened.




Similar content being viewed by others
References
Ministry of Ecology and Environment of the People ' s Republic of China (2016) Ambient Air Quality Standards GB 3095-2012. http://www.mee.gov.cn/ywgz/fgbz/bz/bzwb/dqhjbh/dqhjzlbz/201203/t20120302_224165.shtml. Accessed 25 May 2021
Arias-Pérez RD, Taborda NA, Gómez DM, Narvaez JF, Porras J, Hernandez JC (2020) Inflammatory effects of particulate matter air pollution. Environ Sci Pollut Res 27(34):42390–42404. https://doi.org/10.1007/s11356-020-10574-w
Bi J, D’Souza RR, Rich DQ, Hopke PK, Russell AG, Liu Y, Chang HH, Ebelt S (2020) Temporal changes in short-term associations between cardiorespiratory emergency department visits and PM2.5 in Los Angeles, 2005 to 2016. Environ Res 190:109967. 10/ghfsrs
Bowe B, Xie Y, Yan Y, Al-Aly Z (2019) Burden of cause-specific mortality associated with PM2.5 air pollution in the United States. JAMA Netw Open 2(11):e1915834. 10/ggwwq6
Chen R, Yin P, Meng X, Liu C, Wang L, Xu X, Ross JA, Tse LA, Zhao Z, Kan H, Zhou M (2017) Fine particulate air pollution and daily mortality. A Nationwide Analysis in 272 Chinese Cities. Am J Respir Crit Care Med 196(1):73–81. 10/gbmg49
Chen Y, Zheng M, Lv J, Shi T, Liu P, Wu Y, Feng W, He W, Guo P (2019) Interactions between ambient air pollutants and temperature on emergency department visits: analysis of varying-coefficient model in Guangzhou, China. Sci Total Environ 668:825–834. 10/ghh8gk
Chen R, Gao Q, Sun J, Yang H, Li Y, Kang F, Wu W (2020) Short-term effects of particulate matter exposure on emergency room visits for cardiovascular disease in Lanzhou, China: A time series analysis. Environ Sci Pollut Res 27(9):9327–9335. 10/ghjmz6
Choi Y-J, Kim S-H, Kang S-H, Kim S-Y, Kim O-J, Yoon C-H, Lee H-Y, Youn T-J, Chae I-H, Kim C-H (2019) Short-term effects of air pollution on blood pressure. Sci Rep 9(1):20298. 10/ggzvcp
Chu X, Liu X-J, Qiu J-M, Zeng X-L, Bao H-R, Shu J (2016) Effects of Astragalus and Codonopsis pilosula polysaccharides on alveolar macrophage phagocytosis and inflammation in chronic obstructive pulmonary disease mice exposed to PM2.5. Environ Toxicol Pharmacol 48:76–84. 10/f9hknd
Cui J, Lang J, Chen T, Mao S, Cheng S, Wang Z, Cheng N (2019) A framework for investigating the air quality variation characteristics based on the monitoring data: case study for Beijing during 2013–2016. J Environ Sci 81:225–237. 10/gg5hkt
Dastoorpoor M, Sekhavatpour Z, Masoumi K, Mohammadi MJ, Aghababaeian H, Khanjani N, Hashemzadeh B, Vahedian M (2019) Air pollution and hospital admissions for cardiovascular diseases in Ahvaz, Iran. Sci Total Environ 652:1318–1330. 10/ghcmkr
Day DB, Xiang J, Mo J, Li F, Chung M, Gong J, Weschler CJ, Ohman-Strickland PA, Sundell J, Weng W, Zhang Y, Zhang J(J) (2017) Association of ozone exposure with cardiorespiratory pathophysiologic mechanisms in healthy adults. JAMA Intern Med 177(9):1344. 10/ghjm5m
Dong G-H, Qian Z(M), Wang J, Chen W, Ma W, Trevathan E, Xaverius PK, DeClue R, Wiese A, Langston M, Liu M-M, Wang D, Ren W-H (2013) Associations between ambient air pollution and prevalence of stroke and cardiovascular diseases in 33 Chinese communities. Atmos Environ 77:968–973. 10/f5bsj2
Feng W, Li H, Wang S, Van Halm-Lutterodt N, An J, Liu Y, Liu M, Wang X, Guo X (2019) Short-term PM10 and emergency department admissions for selective cardiovascular and respiratory diseases in Beijing, China. Sci Total Environ 657:213–221. 10/ghcmk5
Fiordelisi A, Piscitelli P, Trimarco B, Coscioni E, Iaccarino G, Sorriento D (2017) The mechanisms of air pollution and particulate matter in cardiovascular diseases. Heart Fail Rev 22(3):337–347. 10/f98sbh
Folino AF, Scapellato ML, Canova C, Maestrelli P, Bertorelli G, Simonato L, Iliceto S, Lotti M (2009) Individual exposure to particulate matter and the short-term arrhythmic and autonomic profiles in patients with myocardial infarction. Eur Heart J 30(13):1614–1620. 10/bzk2z4
Franchini M, Mannucci PM (2011) Thrombogenicity and cardiovascular effects of ambient air pollution. Blood 118(9):2405–2412. 10/fvgv3f
Franklin BA, Brook R, Arden Pope C, 3rd (2015) Air pollution and cardiovascular disease. Curr Probl Cardiol 40(5):207–238. https://doi.org/10.1016/j.cpcardiol.2015.01.003
Gasparrini A (2011) Distributed lag linear and non-linear models in R: the package dlnm. J Stat Softw 43(8):1–20
Ge E, Lai K, Xiao X, Luo M, Fang Z, Zeng Y, Ju H, Zhong N (2018) Differential effects of size-specific particulate matter on emergency department visits for respiratory and cardiovascular diseases in Guangzhou, China. Environ Pollut 243:336–345. 10/gfp8z9
Gu J, Shi Y, Chen N, Wang H, Chen T (2020) Ambient fine particulate matter and hospital admissions for ischemic and hemorrhagic strokes and transient ischemic attack in 248 Chinese cities. Sci Total Environ 715:136896. 10/ghjk2t
Hamanaka RB, Mutlu GM (2018) Particulate matter air pollution: effects on the cardiovascular system. Front Endocrinol 9:680. 10/gfqw5s
Hayes RB, Lim C, Zhang Y, Cromar K, Shao Y, Reynolds HR, Silverman DT, Jones RR, Park Y, Jerrett M, Ahn J, Thurston GD (2020) PM2.5 air pollution and cause-specific cardiovascular disease mortality. Int J Epidemiol 49(1):25–35. 10/ghfhcr
Hu J, Tang M, Zhang X, Ma Y, Li Y, Chen R, Kan H, Cui Z, Ge J (2020) Size-fractionated particulate air pollution and myocardial infarction emergency hospitalization in Shanghai, China. Sci Total Environ 737:140100. 10/ghg49h
Huang C, Wang Q, Wang S, Ren M, Ma R, He Y (2017) Air pollution prevention and control policy in China. Adv Exp Med Biol 1017:243–261. 10/ghg8dk
Ioanna T, Paul E, Vasilis K, Majid E (2016) Worldwide exposures to cardiovascular risk factors and associated health effects. Circulation 133(23):2314–2333. 10/f8p22w
Jiang S, Zhou J, Zhang J, Du X, Zeng X, Pan K, Xie Y, Kan H, Sun Q, Cai J, Zhao J (2018) The severity of lung injury and metabolic disorders induced by ambient PM2.5 exposure is associated with cumulative dose. Inhal Toxicol 30(6):239–246. 10/gj7mjs
Jiang L, Ye L, Dai M, Zhou J, Li Q (2020) Use Andersen’s behavior model to explain non-urgent visits in emergency department: A single center study in southwest China. Int Emerg Nurs 52:100845. 10/gj7c9w
Kan H, Pan D, Castranova V (2018) Engineered nanoparticle exposure and cardiovascular effects: the role of a neuronal-regulated pathway. Inhal Toxicol 30(9–10):335–342. 10/gj7mj3
Kojima S, Michikawa T, Matsui K, Ogawa H, Yamazaki S, Nitta H, Takami A, Ueda K, Tahara Y, Yonemoto N, Nonogi H, Nagao K, Ikeda T, Sato N, Tsutsui H, Japanese Circulation Society With Resuscitation Science Study (JCS-ReSS) Group (2020) Association of fine particulate matter exposure with bystander-witnessed out-of-hospital cardiac arrest of cardiac origin in Japan. JAMA Netw Open 3(4):e203043. 10/ghg5bj
Kwon OK, Kim SH, Kang SH, Cho Y, Oh IY, Yoon CH, Kim SY, Kim OJ, Choi EK, Youn TJ, Chae IH (2019) Association of short- and long-term exposure to air pollution with atrial fibrillation. Eur J Prev Cardiol 26(11):1208–1216. https://doi.org/10.1177/2047487319835984
Leepe KA, Li M, Fang X, Hiyoshi A, Cao Y (2019) Acute effect of daily fine particulate matter pollution on cerebrovascular mortality in Shanghai, China: a population-based time series study. Environ Sci Pollut Res 26(25):25491–25499. 10/ghhx8n
Li J, Liu F, Liang F, Huang K, Yang X, Xiao Q, Chen J, Liu X, Cao J, Chen S, Shen C, Yu L, Lu F, Wu X, Zhao L, Wu X, Li Y, Hu D, Huang J et al (2020) Long-term effects of high exposure to ambient fine particulate matter on coronary heart disease incidence: a population-based Chinese cohort study. Environ Sci Technol 54(11):6812–6821. 10/gj7hmp
Liu C, Chen R, Zhao Y, Ma Z, Bi J, Liu Y, Meng X, Wang Y, Chen X, Li W, Kan H (2017) Associations between ambient fine particulate air pollution and hypertension: a nationwide cross-sectional study in China. Sci Total Environ 584–585:869–874. 10/f95rkh
Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Guo Y, Tong S, Coelho MSZS, Saldiva PHN, Lavigne E, Matus P, Valdes Ortega N, Osorio Garcia S, Pascal M, Stafoggia M, Scortichini M, Hashizume M, Honda Y, Hurtado-Díaz M, Cruz J et al (2019a) Ambient particulate air pollution and daily mortality in 652 cities. N Engl J Med 381(8):705–715. 10/gf6svh
Liu M, Xue X, Zhou B, Zhang Y, Sun B, Chen J, Li X (2019b) Population susceptibility differences and effects of air pollution on cardiovascular mortality: epidemiological evidence from a time-series study. Environ Sci Pollut Res 26(16):15943–15952. 10/ghhdtw
Liu S, Wang L, Zhou L, Li W, Pu X, Jiang J, Chen Y, Zhang L, Qiu H (2020) Differential effects of fine and coarse particulate matter on hospitalizations for ischemic heart disease: a population-based time-series analysis in Southwestern China. Atmos Environ 224:117366. 10/ghjfp8
Liu Y, Zhao H, Ma Y, Yang H, Wang Y, Wang H, Zhang Y, Zou X, Wang H, Wen R, Zhao Z, Quan W (2021) Characteristics of particulate matter and meteorological conditions of a typical air-pollution episode in Shenyang, northeastern China, in winter 2017. Atmos Pollut Res 12(1):316–327. 10/gj28q4
Lu Y, Lin S, Fatmi Z, Malashock D, Hussain MM, Siddique A, Carpenter DO, Lin Z, Khwaja HA (2019) Assessing the association between fine particulate matter (PM2.5) constituents and cardiovascular diseases in a mega-city of Pakistan. Environ Pollut 252:1412–1422. 10/ghjdvh
Ma Y, Chen R, Pan G, Xu X, Song W, Chen B, Kan H (2011) Fine particulate air pollution and daily mortality in Shenyang, China. Sci Total Environ 409(13):2473–2477. 10/fw5z2x
Macintyre HL, Heaviside C, Neal LS, Agnew P, Thornes J, Vardoulakis S (2016) Mortality and emergency hospitalizations associated with atmospheric particulate matter episodes across the UK in spring 2014. Environ Int 97:108–116. 10/ghp32t
Miller KA, Siscovick DS, Sheppard L, Shepherd K, Sullivan JH, Anderson GL, Kaufman JD (2007) Long-term exposure to air pollution and incidence of cardiovascular events in women. N Engl J Med 356(5):447–458. 10/crtn4v
Mills NL, Törnqvist H, Robinson SD, Gonzalez M, Darnley K, MacNee W, Boon NA, Donaldson K, Blomberg A, Sandstrom T, Newby DE (2005) Diesel exhaust inhalation causes vascular dysfunction and impaired endogenous fibrinolysis. Circulation 112(25):3930–3936. 10/d7mf32
Mills NL, Robinson SD, Fokkens PHB, Leseman DLAC, Miller MR, Anderson D, Freney EJ, Heal MR, Donovan RJ, Blomberg A, Sandström T, MacNee W, Boon NA, Donaldson K, Newby DE, Cassee FR (2008) Exposure to concentrated ambient particles does not affect vascular function in patients with coronary heart disease. Environ Health Perspect 116(6):709–715. 10/bvzhsk
Murray CJL, Aravkin AY, Zheng P, Abbafati C, Abbas KM, Abbasi-Kangevari M, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, Abegaz KH, Abolhassani H, Aboyans V, Abreu LG, Abrigo MRM, Abualhasan A, Abu-Raddad LJ, Abushouk AI, Adabi M et al (2020) Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1223–1249. 10/ghfx5v
Pan H, Hibino M, Kobeissi E, Aune D (2020) Blood pressure, hypertension and the risk of sudden cardiac death: a systematic review and meta-analysis of cohort studies. Eur J Epidemiol 35(5):443–454. 10/ghg5tz
Pope Iii CA, Burnett RT, Thun MJ, Calle EE, Krewski D, Ito K, Thurston GD (2002) Lung cancer, cardiopulmonary mortality, and long-term exposure to fine particulate air pollution. Jama 287(9):1132–1141. 10/cvqphv
Pu H, Li J, Wang P, Cui L, Wang H (2017) The death of the circulatory system diseases in China: Provincial socioeconomic and environmental perspective. Environ Sci Pollut Res 24(11):10381–10390. 10/f94wzv
R Core Team (2020) R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/
Rider CF, Carlsten C (2019) Air pollution and DNA methylation: effects of exposure in humans. Clin Epigenetics 11. 10/ghfsrf
Rodopoulou S, Samoli E, Chalbot M-CG, Kavouras IG (2015) Air pollution and cardiovascular and respiratory emergency visits in Central Arkansas: a time-series analysis. Sci Total Environ 536:872–879. 10/ghfsrj
Rodríguez-Villamizar LA, Rojas-Roa NY, Fernández-Niño JA (2019) Short-term joint effects of ambient air pollutants on emergency department visits for respiratory and circulatory diseases in Colombia, 2011-2014. Environ Pollut 248:380–387. https://doi.org/10.1016/j.envpol.2019.02.028
Sarnat SE, Winquist A, Schauer JJ, Turner JR, Sarnat JA (2015) Fine particulate matter components and emergency department visits for cardiovascular and respiratory diseases in the St. Louis, Missouri–Illinois, Metropolitan Area. Environ Health Perspect 123(5):437–444. 10/ghhxdp
Schwartz J (2000) Harvesting and long term exposure effects in the relation between air pollution and mortality. Am J Epidemiol 151(5):440–448. 10/bmwd
Shen Z, Sun J, Cao J, Zhang L, Zhang Q, Lei Y, Gao J, Huang R-J, Liu S, Huang Y, Zhu C, Xu H, Zheng C, Liu P, Xue Z (2016) Chemical profiles of urban fugitive dust PM2.5 samples in Northern Chinese cities. Sci Total Environ 569–570:619–626. 10/f82xrt
Shi Y, Wang G, Gao X, Xu Y (2018) Effects of climate and potential policy changes on heating degree days in current heating areas of China. Sci Rep 8(1):1–13. 10/gdxz3m
Solimini AG, Renzi M (2017) Association between air pollution and emergency room visits for atrial fibrillation. Int J Environ Res Public Health 14(6):661. https://doi.org/10.3390/ijerph14060661
Song C, Wu L, Xie Y, He J, Chen X, Wang T, Lin Y, Jin T, Wang A, Liu Y, Dai Q, Liu B, Wang Y, Mao H (2017) Air pollution in China: status and spatiotemporal variations. Environ Pollut 227:334–347. 10/gbmbsn
Song J, Lu M, Lu J, Chao L, An Z, Liu Y, Xu D, Wu W (2019) Acute effect of ambient air pollution on hospitalization in patients with hypertension: a time-series study in Shijiazhuang, China. Ecotoxicol Environ Saf 170:286–292. 10/ghh3kw
Tapia V, Steenland K, Sarnat SE, Vu B, Liu Y, Sánchez-Ccoyllo O, Vasquez V, Gonzales GF (2020) Time-series analysis of ambient PM2.5 and cardiorespiratory emergency room visits in Lima, Peru during 2010-2016. J Expo Sci Environ Epidemiol 30(4):680–688. 10/ghjfgb
Tian L, Sun S (2017) Comparison of health impact of air pollution between China and other countries. Adv Exp Med Biol 1017:215–232. 10/ghg8dq
Tian Y, Xiang X, Juan J, Song J, Cao Y, Huang C, Li M, Hu Y (2018) Short-term effect of ambient ozone on daily emergency room visits in Beijing, China. Sci Rep 8(1):2775. 10/gc29d7
Tian M, Zhao J, Mi X, Wang K, Kong D, Mao H, Wang T (2021) Progress in research on effect of PM2.5 on occurrence and development of atherosclerosis. J Appl Toxicol 41(5):668–682. 10/gj7mn4
Tobaldini E, Iodice S, Bonora R, Bonzini M, Brambilla A, Sesana G, Bollati V, Montano N (2020) Out-of-hospital cardiac arrests in a large metropolitan area: synergistic effect of exposure to air particulates and high temperature. Eur J Prev Cardiol 27(5):513–519. 10/ghh8gj
Vanasse A, Talbot D, Chebana F, Bélanger D, Blais C, Gamache P, Giroux J-X, Dault R, Gosselin P (2017) Effects of climate and fine particulate matter on hospitalizations and deaths for heart failure in elderly: a population-based cohort study. Environ Int 106:257–266. 10/gbpzs6
von Bornstädt D, Kunz A, Endres M (2014) Impact of particulate matter exposition on the risk of ischemic stroke: epidemiologic evidence and putative mechanisms. J Cereb Blood Flow Metab 34(2):215–220. 10/f5rm89
Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, Abbasi-Kangevari M, Abbastabar H, Abd-Allah F, Abdelalim A, Abdollahi M, Abdollahpour I, Abolhassani H, Aboyans V, Abrams EM, Abreu LG, Abrigo MRM, Abu-Raddad LJ, Abushouk AI et al (2020) Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396(10258):1204–1222. 10/ghf2zj
Wang C, Feng L, Chen K (2019) The impact of ambient particulate matter on hospital outpatient visits for respiratory and circulatory system disease in an urban Chinese population. Sci Total Environ 666:672–679. 10/ghcmk9
Wen LS, Xu J, Steptoe AP, Sullivan AF, Walline JH, Yu X, Camargo CA (2013) Emergency department characteristics and capabilities in Beijing, China. J Emerg Med 44(6):1174–1179.e4. 10/f42qdr
Wood SN (2017) Generalized additive models: an introduction with R. CRC press
World Health Organization (2018) Ambient (outdoor) air pollution. https://www.who.int/news-room/fact-sheets/detail/ambient-(outdoor)-air-quality-and-health
Wu X, Braun D, Schwartz J, Kioumourtzoglou MA, Dominici F (2020) Evaluating the impact of long-term exposure to fine particulate matter on mortality among the elderly. Sci Adv 6(29):eaba5692. 10/ghhqx5
Xu Q, Wang S, Guo Y, Wang C, Huang F, Li X, Gao Q, Wu L, Tao L, Guo J, Wang W, Guo X (2017) Acute exposure to fine particulate matter and cardiovascular hospital emergency room visits in Beijing, China. Environ Pollut 220:317–327. 10/ghf3q5
Yang F, Tan J, Zhao Q, Du Z, He K, Ma Y, ... Chen GJAC (2011) Characteristics of PM 2.5 speciation in representative megacities and across China. Atmos Chem Phys 11(11):5207–5219. https://doi.org/10.5194/acp-11-5207-2011
Yang BY, Guo Y, Markevych I, Qian ZM, Bloom MS, Heinrich J, Dharmage SC, Rolling CA, Jordan SS, Komppula M, Leskinen A, Bowatte G, Li S, Chen G, Liu KK, Zeng XW, Hu LW, Dong GH (2019) Association of long-term exposure to ambient air pollutants with risk factors for cardiovascular disease in China. JAMA Network Open 2(3):e190318. https://doi.org/10.1001/jamanetworkopen.2019.0318
Yang J, Zhou M, Li M, Yin P, Hu J, Zhang C, Wang H, Liu Q, Wang B (2020a) Fine particulate matter constituents and cause-specific mortality in China: a nationwide modelling study. Environ Int 143:105927. 10/ghg5nm
Yang L, Li C, Tang X (2020b) The impact of PM(2.5) on the host defense of respiratory system. Front Cell Dev Biol 8:91–91. 10/gj6r9q
Yang M, Zhou R, Qiu X, Feng X, Sun J, Wang Q, Lu Q, Zhang P, Liu B, Li W, Chen M, Zhao Y, Mo B, Zhou X, Zhang X, Hua Y, Guo J, Bi F, Cao Y et al (2020c) Artificial intelligence-assisted analysis on the association between exposure to ambient fine particulate matter and incidence of arrhythmias in outpatients of Shanghai community hospitals. Environ Int 139:105745. 10/ghh7ks
Yu Y, Yao S, Dong H, Wang L, Wang C, Ji X, Ji M, Yao X, Zhang Z (2019) Association between short-term exposure to particulate matter air pollution and cause-specific mortality in Changzhou, China. Environ Res 170:7–15. 10/ghhrfm
Zeng W, Zhang Y, Wang L, Wei Y, Lu R, Xia J, Chai B, Liang X (2018) Ambient fine particulate pollution and daily morbidity of stroke in Chengdu, China. PLoS One 13(11):e0206836. 10/gfk8dj
Zhan D, Kwan M-P, Zhang W, Wang S, Yu J (2017) Spatiotemporal variations and driving factors of air pollution in China. Int J Environ Res Public Health 14(12):1538. 10/gcxwwf
Zhang Y, Wang S, Fan X, Ye X (2018) Temperature modulation of the health effects of particulate matter in Beijing. China. Environ Sci Pollut Res Int 25(11):10857–10866. https://doi.org/10.1007/s11356-018-1256-3
Zhou X, Cao Z, Ma Y, Wang L, Wu R, Wang W (2016) Concentrations, correlations and chemical species of PM2.5/PM10 based on published data in China: Potential implications for the revised particulate standard. Chemosphere 144:518–526. 10/f768gm
Zhu Y, Wang Y, Xu H, Luo B, Zhang W, Guo B, Chen S, Zhao X, Li W (2020) Joint effect of multiple air pollutants on daily emergency department visits in Chengdu, China. Environ Pollut 257:113548. 10/ghhxc8
Zuo B, Liu C, Chen R, Kan H, Sun J, Zhao J, Wang C, Sun Q, Bai H (2019) Associations between short-term exposure to fine particulate matter and acute exacerbation of asthma in Yancheng, China. Chemosphere 237:124497. 10/ghcmkx
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
This study was supported by the National Natural Science Foundations of China (42077396); Key Projects of Natural Science Foundation of Liaoning Province, China (20170541038). We appreciate the support of Key Laboratory of Environmental Health Damage Research and Assessment, Liaoning Province, for this research.
Author information
Authors and Affiliations
Contributions
Chenkai Zhao: Conceptualization; Methodology; Software; Data curation; Writing, original draft. Qidian Li: Writing, original draft. Zhongming Cui: Writing, review and editing. Junlong Wang: Writing, review and editing. Junlong Wang: Writing, review and editing. Li Sun: Writing, review and editing. Yan Yin: Project administration; Conceptualization; Writing, review and editing.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
There is no potential risk to population health in this study, so the Ethics Committee of China Medical University has confirmed that no ethical approval is required.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 8534 kb)
Rights and permissions
About this article
Cite this article
Zhao, C., Li, Q., Cui, Z. et al. Impact of ambient fine particulate matter on emergency department admissions for circulatory system disease in a city in Northeast China. Environ Sci Pollut Res 28, 62839–62852 (2021). https://doi.org/10.1007/s11356-021-15222-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-15222-5