Abstract
Public transport is a fundamental service for the resumption of work and production, but the enclosed environment and dense population create very favorable conditions for the spread of epidemic infections. Thus, effective public health interventions are urgently introduced. The objective of this paper is to quantitatively estimate the SARS-CoV-2 transmission probability and evaluate the influence of environmental parameters and individual intervention on the epidemic prevention. For this purpose, (1) we estimate the virus emission rate with Diamond Princess Cruise Ship infection data by Monte Carlo simulation and the improved Wells-Riley model, and (2) employ the reproductive number R to quantify diverse mitigation strategies. Different determinants are examined such as the duration of exposure, the number of passengers combined with individual interventions such as mask type and mask-wearing rate. The results show that the SARS-CoV-2 quantum generation rate is 185.63. The R shows a stronger positive correlation with the exposure time comparing to the number of passengers. In this light, reducing the frequency of long-distance journeys on crowded public transportation may be required to reduce the spread of the virus during the pandemic. N95 mask and surgical mask can reduce the transmission risk by 97 and 84%, respectively, and even homemade mask can reduce the risk by 67%, which indicates that it is necessary to advocate wearing masks on public transportation.
Similar content being viewed by others
Introduction
As of 9th November 2020, the novel coronavirus disease (COVID-19) has reached more than 50 million confirmed cases and 125 thousands deaths globally and, as of now, it is still spreading exponentially (Coronavirus Resource Center, Johns Hopkins University 2020). After lifting the public restrictions slightly, the outbreak significantly rebounded in the USA, Europe, and China (Grossman 2020; Vega 2020). To cope with the second wave, contact tracing and epidemiological quarantine were immediately strengthened in the affected areas. It can be seen that the prevention and control work in the global COVID-19 epidemic is facing another new challenge. In the face of the protracted war against the emerging epidemic, which is full of unknown factors, epidemic control and the resumption of work and production are the dilemmas faced by most countries during this crucial period. To quantify the public health risk in the confined space and make mitigation strategies, estimating the characteristics of the COVID-19 transmission probability is particularly pivotal.
The virus can spread between people in several routes. Susceptible people may catch COVID-19 when the virus gets into their mouth, nose, or eyes by direct contact with an infected person (World Health Organization 2020). Under other circumstances, the transmission routes are caused by respiratory droplets generated from cough, sneeze, speak, and breathe (Qian et al. 2018; Wenzhao Chen et al. 2020). From the moment the droplets are exhaled, they are experiencing physical changes, such as evaporation, which leads to the particle sizes ranging from larger “droplets” to smaller “aerosols or droplet nuclei,” with liquid sizes from 0.1 to 100 μm (Chenari et al. 2016; Inthavong et al. 2012). The large pathogen-load droplets may splash directly into the mouth or nasal mucous of exposed people nearby (less than 1 m), causing close contact transmission, and it can also settle on surfaces, resulting in indirect contact transmission (Qian et al. 2018). Droplets smaller than 100 μm will evaporate within seconds, forming droplet nuclei or aerosols (Hua et al. 2012) and the size smaller than 5 μm can suspend in the air for a long time (Morawska et al. 2009; Wenzhao Chen et al. 2020; Zhang et al. 2020). The floating virus in the air can spread over a long distance and may have a chance to be inhaled by healthy people under particular indoor, crowded, and inadequately ventilated spaces (Buonanno et al. 2020a; Correia et al. 2020).
Although the WHO, Disease Control and Prevention (CDC), and other organizations have accepted that SARS-COV-2 is primarily caused by large droplets and direct contact transmission (Neeltje Van Doremalen et al. 2020; Tellier et al. 2019), airborne transmission by inhaling aerosols carrying the virus should not be ruled out, and some studies have indeed shown the possibilities of SARS-CoV-2 airborne transmission. The National Academies of Sciences, Engineering and Medicine (National Academies Of Sciences 2020) recently reported that the collected gases exhaled by patients showed the evidence of SARS-CoV-2, implicitly indicating its airborne transmission. Jiang (Y. Jiang et al. 2020) also gave the evidence of SARS-CoV-2 in hospital air. Van (Neeltje Van Doremalen et al. 2020) found that SARS-CoV-2 could survive in aerosols for up to several hours. Guo (Guo et al. 2020) pointed out that SARS-CoV-2 was not only widely distributed in the air, but also had a transmission distance of up to 4 m. A series of studies verifying SARS-CoV-2 airborne transmission potential were being published (Ghinai et al. 2020; Jianyun et al. 2020; Morawska and Cao 2020; Park et al. 2020; Read 2020). Hence, the WHO updated the transmission routes on 20th October, 2020, adding airborne transmission as an additional route (World Health Organization 2020). A schematic diagram about how SARS-CoV-2 spread between people is shown in Fig. 1.
People live and work in the indoor environment for more than 80% of their time (Klepeis et al. 2001). From the perspective of epidemic prevention and control, interpersonal communication in a confined space creates a favorable environment for respiratory viruses through close contact and airborne transmission, which is likely to trigger a higher risk of infection. Especially, after the resumption of work and production, public transport has once again become the normal way of daily commuting and travel. The narrow social distancing on public transportation leads to a higher risk of inhaling the droplets at an early stage. If an asymptomatic patient coughs on a bus without wearing a mask during the peak hours, the virus droplets can be expelled at a speed of 10 m/s, with a concentration as high as 108 copies/mL (Buonanno et al. 2020a, 2020b; Neeltje Van Doremalen et al. 2020), so that adjacent passengers can instantly inhale the virus droplets. Study showed that despite the rapid inactivation in the number of virus, the relative survival rate could maintain at 88% after 30 min of exposure to air, the infection risks cannot be ignored (Buonanno et al. 2020b; Wenzhao Chen et al. 2020), thus earlier inhalation of the virus droplets will aggravate the risk of infection.
However, the success of virus infection in susceptible individuals is complicated by many factors. On departure from the host (initial velocity, particle size, and number of droplets), pathogen-load droplets will undergo heat and mass transfer under diverse indoor environment, which dramatically changes their living environment. The process leads to abundant decay and degraded reproductive activity of the virus. Furthermore, the exposure time of the vulnerable group is uncertain. This makes the deposition location and status of pathogens in the respiratory tract caused by aerodynamic influences still not well explained. At last, the heterogeneous immunity of susceptible people makes it difficult to predict the probability of infection from the mechanism perspective. Hence, it could be better to develop a respiratory diseases transmission model in conjunction with statistical concept to predict the infection probability at the early stage of the pandemic, just like other infectious diseases prediction.
When the risk of transmission routes was not clear, many scholars used statistical methods to rapidly predict the infection risks of respiratory diseases in a confined space or even on a larger scale, like a city, and provided prevention and control strategies. Buonanno et al. (Buonanno et al. 2020b) used the Gammaitoni-Nucci model to quantify the risk of SARS-COV-2 through airborne transmission, obtaining the variation rule of the quantum generation rate of SARS-CoV-2 under different behavior. The paper predicted the basic reproductive number for post offices, restaurants, supermarkets, banks, and clinics in Italy with the quanta emission rate of 142 and evaluated the impact of public intervention on curbing the spread of the epidemic. Liao et al. (Liao et al. 2005; Liao et al. 2008) predicted the airborne transmission risks of SARS, influenza, measles and chickenpox such respiratory diseases on a Boeing 737 aircraft by using the SIR model and the Wells-Riley model, obtaining the quanta values of different epidemics, and proposed that increasing the fresh air exchange was an efficient control measure to reduce the epidemic transmission. Furuya (FURUYA 2007) estimated that the basic reproductive number of influenza virus on trains was 2.2 by using the Wells-Riley model, and put forward that ventilation was an effective way to minimize the risk of transmission. Zhang (Zhang et al. 2018) used the SIR and Wells-Riley models to predict the infection risk of respiratory diseases at different locations in Hong Kong by taking into account the spatial and temporal dimensions of population mobility. Oslen et al. (Olsen et al. 2003) applied contact tracing in studying the actual infection case reports of three flights carrying SARS patients, and found that the risk to passengers was related to the relative position of the infected person on the plane. The infection risk appeared to be higher where the seats are located in three rows from the infected source. Mizumoto and Chowell (Mizumoto and Chowell 2020) used mathematical modeling to predict that the basic reproductive number of SARS-CoV-2 on the Diamond Princess Cruise Ship reached 11.
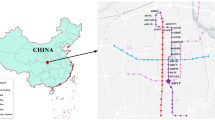
February 2020 was the early stage of the outbreak of the epidemic; unfortunately, it fell on the period of the Spring Festival in China. Various kinds of public transportation were frequently used, leading to the high risk of infection. Estimating the infection risk of SARS-CoV-2 involves interdisciplinary researches, including virology, epidemiology, aerosol science, and engineering. What is worse, for the emerging pandemic, the relevant epidemic parameters were unclear and lacked detailed data for estimating. In order to quickly carry out a quantitative prediction of SARS-CoV-2 transmission risk in the public transportation and make scientific mitigation strategies, this paper firstly used the classic Wells-Riley model to estimate the quantum of SARS-CoV-2 on the basis of the actual daily infection cases of the Diamond Princess Cruise Ship. Secondly, we predicted the basic reproductive number R in similar transportation vehicles such as air-conditioned buses by using the SARS-CoV-2 quantum of the Diamond Princess Cruise Ship. Thirdly, by simulating the transmission probabilities under various bus scheduling and mask-wearing efficiency, we discussed the prevention and control strategies in such spaces and proposed useful optimization suggestions. The findings also provided reference for efficient decision making in COVID-19 epidemic prevention and control.
Materials and methods
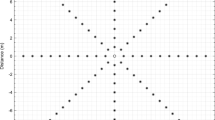
Quantitative epidemiology of SARS-CoV-2
Infection data of the Diamond Princess Cruise Ship was collected from the daily confirmed new cases reported by the Ministry of Health, Labor and Welfare of Japan from 3rd February, 2020 to 23rd February, 2020 (Ministry of Health, Labor and Welfare, Japan 2020). With the detailed epidemiological data from reported cases regarding influenza and SARS, the respiratory diseases were estimated a log-normal distribution fitted to the infection data (FURUYA 2007; Liao et al. 2005; Liao et al. 2008). Hence, we used Monte Carlo simulation to quantify the daily infection rate of the Diamond Princess Cruise Ship. After optimizing the Kolmogorov-Smirnov (K-S) statistics, log-normal distribution was the best fit for daily infection rate. Then, we obtained the SARS-CoV-2 quantum generation rate by substituting the physical parameters of the Diamond Princess Cruise Ship and the estimated infection rate through the Wells-Riley model. Finally, according to the quantum generation rate of the Diamond Princess Cruise Ship together with public bus physical parameters and Wells-Riley model, the basic reproductive number R of buses in accordance with log-normal distribution was obtained after using the K-S method. The research process was shown in Fig. 2. We employed the Crystal Ball software (Version 2015, ORACLE, Inc., Redwood Shores, CA, USA) to analyze the data and to estimate the distribution parameters. For this study, 10,000 iterations were sufficient to ensure stability of the results.
Transmission model
The probability of infection is related to many factors, such as the number of virus, the type of virus, transmission routes, and the immunity of the host (Morawska and Cao 2020). Because these parameters are difficult to accurately determine, resulting in obstacles to quantitatively predict the risk of respiratory diseases, therefore, many respiratory infectious disease prediction models were developed on the basis of statistical concepts. Wells in 1955 put forward the concept of “quanta” to determine the probability of airborne transmission diseases. Quanta was defined as the minimum number of pathogens required to infect a person, which may consist of one or more infectious particles (William Firth Wells 1955). From the perspective of statistics, Riley believed that the average probability of infection was subject to Poisson distribution, so quanta was then defined as the number of infectious particles that can cause 63.2% susceptible people infected in an indoor environment, and proposed the Wells-Riley equation in 1978 (Riley et al. 1978):
where PI is the probability of infection, I is the initial number of confirmed people, C is the number of infection cases caused by I, S is the number of susceptible people, p is the breathing rate of each person, q is the quanta productivity, t is the exposure time, and Q is the room ventilation rate.
The Wells-Riley model assumes that the air in the room is well mixed and the concentration of infectious particles together with the ventilation rate are under steady state. (Riley et al. 1978) The equation is a stochastic model and it can be applied to many diseases. Quanta cannot be obtained directly through the equation, but it can be reversely obtained according to the infection cases, thus the respiratory deposition of infectious particles, the biological decay of pathogens in droplet state, as well as the many complexities of airborne diseases transmission are implicitly considered when calculating the quantum generation rate. It is an indicator of the virus transmission ability, which is a statistical concept. Once the quanta for a specific respiratory infectious disease is acknowledged, the risk assessment for the pandemic under diverse indoor environment could be rapidly quantified by the Wells-Riley model (G N Sze To and Christopher Yu Hang Chao 2010). For instance, Liao et al. (2005) calculated quantum value of influenza (66.91) and SARS (28.77), and compared estimating the two virus infected probability in hospital, school, and aircraft.
Whereas, in reality, the outdoor air supply rate changes along time and it is difficult to measure. By proposing the concept of the fraction of inhaled air that has been exhaled previously by someone in the space (rebreathed fraction), the Wells-Riley model can be derived that considered the variation of the infective particles concentration with ventilation and the non-uniform distribution of infective particles at different locations in a finite space (Rudnick and Milton 2003), as shown below:
where P is the probability of infection for susceptible people, I is the initial number of infectors, D is the final number of infectors that caused by I, S is the total number of susceptible people, q is the quantum generation rate (quanta/h) of an infected person, p is the breathing rate per person (m3/h), t is the total exposure time (h), and Q is the outdoor air supply rate (m3/h) and V is the volume of the ventilated space (m3).
The fraction of indoor air that was exhaled-breath (f) is quantified by using total number of people in the ventilated airspace (n), breathing rate per person (p), and outdoor air supply rate (Q), which can be expressed as f = np/Q [18]. Substituting into Eq. (2), the Wells-Riley equation was further modified as Eq. (3), making it more applicable to the large indoor space, such as hospitals. (Chen et al. 2006):
When I = 1, S = n-1, the basic reproductive number (R) in the confined airspace can be obtained, as shown below:
R refers to the average number of secondary infected people by one primary infected patient during the infectious period. It is a key epidemiological parameter to describe the potential of disease transmission, and essentially determines the rate of epidemic transmission. However, the value of R changes over time under different transmission stages of the epidemic and diverse interventions. When R > 1, it implies that the epidemic is spreading through people at an increasing rate, while R < 1, means that the epidemic is disappearing. R = 1 means that the disease has reached a regional equilibrium (Olsen et al. 2003).
Parameters used to estimate quantum for COVID-19 on a cruise ship
The first infection passenger boarded the Diamond Princess Cruise Ship on 20th January, and the virus started to spread quietly until 3rd February, the Japanese medical team boarded the ship for maritime quarantine. The incubation period which refers to the time between infection and the start of infectiousness for SARS-CoV-2 is about 5.9 days (Adam J Kucharski et al. 2020), and it is the first infection stage of the virus. The second stage is the infection period which means the time interval during which the infected individuals could transmit the disease to any susceptible contacts and it is about 2.9 to 6 days (Adam J Kucharski et al. 2020; Wu et al. 2020). The 14 days which started from 20th January to 3rd February covered the above two transmission stages of the virus; in other words, passengers may experience from initially be infected to they could transmit the disease to any susceptible contacts. Besides, according to relevant information and data released by the Japan Institute of Infectious Diseases, combined with the actual situation (passengers could move freely in public space and cabin before quarantine without taking any prevention and control measures), it could be concluded that the spread of the virus has been almost completely developed on the ship (National Institute Of Infectious Diseases 2020). On 5th February, all the passengers including crew members were announced a 14-day quarantine on board until 19th February. Considering the incubation period, therefore, we chose the confirmed cases from 3rd February to 23rd February to calculate the infection rate, which completely demonstrated the spread before passengers finishing quarantine.
On the other hand, the cruise ship adopted an all-air air-conditioned system in which the return air of the room went back to the air-conditioned unit from the corridor tuyere. After mixing with outdoor fresh air, the air was sent back to the room after the temperature and humidity adjustment of the air-conditioned unit. The return air with transmitted virus, possibly, may mix with the fresh air and be sent to other rooms. Even if the return air may pass through the filtering system, the filtering efficiency for SARS-CoV-2 of the filter installed on the cruise ship was not known and may not have been sterilized in time, so the air supply still had the chance to carry the virus. In addition, as we analyzed above, since the initial patient have already infected many people in the early stage, the virus loads have been very large because of accumulated amount of patients. Even if the air supply volume on the cruise ship was huge, the virus concentration may still break the safety threshold in the supplied air (Junzhou et al. 2020); thus, the air-conditioned system on the cruise ship may offer a channel for the airborne spread of the virus.
It is difficult to predict the transmission probability in the whole indoor space. Since there may be asymptomatic cases or infected cases that are still in the incubation period and it is hard to detect infection under such conditions. Additionally, it is impractical to accurately point out the volume, ventilation, and location of the scattered source of infection in each space. Random behaviors lead to diverse infection routes, making it difficult to identify the dominating routes of infection on the ship. Before quarantine, passengers could freely walk down the aisle to the public area for meals and entertainment, and then return to the cabin for rest. Close contact or aerosol transmission is inclined to be found in public areas, while the narrower spaces such as walkways and cabins may have a larger chance of direct and close contact transmission. Fortunately, Chen et al. (2006) has used the Wells-Riley model to study the average transmission risk of respiratory diseases in a hospital after taking into consideration various transmission routes in such a large space. He assumed that the air was well mixed throughout the hospital, and the people were exposed to it for 24 h (Chen et al. 2006). Therefore, in this paper, in order to simply and rapidly predict the quantum generation rate of the Diamond Princess Cruise Ship by the Wells-Riley model, we also assumed that the air on the ship was well mixed, and the risk of various transmission routes represented the average infection probability. The exposure time of passengers on the ship was set at 24 h. The following are the parameters to predict the quantum generation rate of the Diamond Princess Cruise Ship, as shown in Table 1.
The total number of people on the cruise before quarantine was 3711, including passengers and crew members. We calculated the volume of the shared indoor space of the Diamond Princess Cruise Ship based on the open literature for the ship (Vessel Tracker 2020). Further, diverse behavior and activities intensity generate different respiration rates. Since the breathing rates of resting, standing, light exercise, moderate exercise, and heavy exercise vary greatly (0.3 ~ 3.30 m3/h). We chose p = 0.49 m3/h, indicating that the majority of cruise passengers tend to relax. The fresh air supply rate was 28.8m3/h per person according to the International Organization for Standardization of Ships and Marine (International Organization for Standardization 2002); thus, the fraction of indoor air that was exhaled-breath was calculated as f = 0.016.
Parameters used to estimate R for COVID-19 on a bus
In order to verify the model, we obtained the R for a bus with the calculated quantum of COVID-19 and compared it with the actual bus infection cases. Table 2 shows the number of passengers, exposure time, and physical parameters of the actual bus infection cases according to the epidemic contact tracing investigation. In detail, the patient originally took an air-conditioned bus (with 48 passengers) for 2 h, and then transferred to an air-conditioned minibus (with 12 passengers) for 1 h. In the first period of time, eight people were infected. During the second period of time, three people were infected (Sun and Zhai 2020). The volume of the buses was calculated by capacity. The activity intensity value of the passengers on the bus was counted as a low breathing rate which was the same as the Diamond Princess Cruise Ship. The fresh air supply rate was 20m3/h, which was selected according to the People’s Republic of China Transportation Standards JT/T 888-2014 (Ministry of Transport of The People’s Republic of China 2014).
The mask intervention
Public transport, serving as the method of choice for the daily travel of the majority of people, especially as the predominant vehicle for inter-city population movement, has been facing great challenges in preventing SARS-CoV-2 cross-infection due to its limited space and a large number of occupants. Even worse, the high transmission risk of asymptomatic persons during the peak of the outbreak aggravates the challenge. A series of cases of SARS-CoV-2 infection on ships, planes, trains, and buses can be found everywhere through the contact tracing reports of COVID-19 (Moriarty et al. 2020). Direct contact and close contact transmission of SARS-CoV-2 are still the main ways to spread the diseases in closed spaces at present, with not mutually exclusive (Morawska et al. 2020). In these two modes of transmission, a confined space provides a fast channel for the virus from the infected person to the exposed person, so that it can maintain a high virus concentration and vitality in the process of transmission, achieving further reproductive. Due to the coupling effect of multiple factors, such as the different types of virus, virus concentration, environmental conditions, exposure time, and heterogeneous of exposed people, it is difficult to quantify. Thus, the transmission mechanism of SARS-CoV-2 in public transport fluctuates and is still unknown. So passengers should take personal protective measures as much as possible to minimize the risk of infection in a closed vehicle.
The high effectiveness of N95 masks is widely recognized. Whereas, the limited supply at the peak of the outbreak exacerbated the shortage of masks. In the face of the exponentially growing number of new cases, some countries began to encourage the public to use homemade masks that were made of common materials for self-protection (Davies et al. 2013). However, except for N95 masks, the public have always doubt the efficacy of surgical and homemade masks, because the National Institute for Occupational Safety and Health (NOISH) regulated the 0.30 μm particle diameter filtering efficiency as the basis to evaluate the performance of masks; thus, some people pointed out the ordinary masks cannot block exhaled virus droplets of small particle size, and thus wearing masks cannot reduce the risk of infection. Hence, our objective is to quantitatively distinguish the working efficiency of the three kinds of masks through the Wells-Riley model and give scientific mask-wearing suggestions under different conditions.
In order to detect the protection levels of several common masks, we reviewed and analyzed the experimental research results of N95, surgical, and homemade masks according to the four papers (Davies et al. 2013; Lee et al. 2008; Noti et al. 2012; Weber et al. 1993), and used filtration efficiency as the indicator, obtaining the efficiency distribution characteristics along with different particle sizes of the masks, as depicted in Fig. 3.
It can be seen that the five different types of N95 masks do show excellent filtration efficiency for all particle sizes. The filtration efficiency of three surgical masks and one homemade mask are obviously lower than that of N95 masks, especially for small droplets less than 1 μm in diameter. However, it is undeniable that various types of masks can achieve the blocking effect of exhaled droplets to different degrees. The filtering efficiency of N95 masks remained stable above 98% (Lee et al. 2008; Noti et al. 2012), surgical masks ranged from 75 to 93% (Davies et al. 2013; Lee et al. 2008; Noti et al. 2012). Even homemade masks can have a filtering efficiency of 71–82%. Hence, according to the papers, we assumed that the average filtration efficiency of N95, surgical, and homemade masks were 98, 80, 70%, and could reduce the amount of contaminated air inhaled to 0.03, 0.2, and 0.3p, respectively.
Results
Quantum generation rate of SARS-CoV-2 on the Diamond Princess Cruise Ship
Figure 4 shows the daily number of new confirmed cases and cumulative cases of the Diamond Princess Cruise Ship from 3rd February to 23rd February. On 3rd February, 10 people were firstly confirmed as infected, and subsequently, the cumulative number of confirmed cases gradually increased over time, reaching a peak of 99 people on 17th February. By 23rd February, the total cumulative confirmed cases were 691.
According to Fig. 4, we quantified the daily infection rate by Monte Carlo simulation, and optimized the statistics by the K-S method. The infection rate of the Diamond Princess Cruise Ship fitted to a log-normal distribution was LN (0.0173, 2.058).
Then, we substituted the fitted infection rate and parameters in Table 1 into Eq. (3). After the K-S optimization fitting, the quantum generation rate LN (184.64, 2.1) was obtained, as shown in Fig. 5. It can be seen that the median of the quantum generation rate of SARS-CoV-2 is 185.63, which is about six times that of SARS (Chen et al. 2006). The distribution fitted to the long-normal distribution was with a geometric mean of 184.64 and a geometric standard deviation of 2.1.
Basic reproductive number R for air-conditioned buses
Figure 6 is the log-normal distribution curve of R for the two buses based on the fitted quantum generation rate of SARS-CoV-2 in the “Quantum generation rate of SARS-CoV-2 on the Diamond Princess Cruise Ship” section. This figure was obtained by combining the parameters of the air-conditioned bus in Table 2 with the basic reproductive number R prediction Eq. (4), after optimizing the goodness fit of distribution by the K-S method. It can be noticed that the SARS-CoV-2 basic reproductive number R for the 48-seat bus after fitted log-normal distribution is LN (7.48, 1.92), shown in Fig. 6a. The median value is 7.48. Figure 6b shows that the SARS-CoV-2 basic reproductive number R for the 18-seat minibus is LN (2.96, 1.81), with a median value of 3.07. The results showed that the predicted median value R for the bus and minibus in urban transportation was close to the actual number of infections, which proved the reliability of the estimated COVID-19 transmission probability by using the revised Wells-Riley model.
Impact of various masks on COVID-19 epidemic prevention and control
Substituting the modified breathing rate in the above “The mask intervention” section into Eq. (4), we forecasted the basic reproduction number R when all passengers are wearing masks on the bus and minibus. Figure 7 shows the log-normal distribution of the SARS-CoV-2 basic reproductive number R of all passengers on the bus without masks, entirely wearing N95 masks, surgical masks, and homemade masks. It is found that the R is 7.48 without wearing masks. After wearing masks, R decreases to 0.16 (N95 masks), 1.62 (surgical masks), and 2.53 (homemade masks). Even the controversial homemade masks can lower the basic reproductive number R to 2.53, a 66% reduction in transmission risk.
Figure 8 shows the log-normal distribution of the minibus basic reproductive number R under four scenarios: without masks, N95 masks, surgical masks, and homemade masks. As shown in Fig. 8, the value of R without wearing masks is 3.07. After wearing it, R decreases to 0.07 (N95 masks), 0.67 (surgical masks), and 1.01 (homemade masks), respectively. In other words, under the condition that all passengers are wearing surgical masks, the basic reproductive number R would be directly reduced to 0.67, which means that if there is a SARS-CoV-2 carrier on the bus while all other passengers are wearing surgical masks, the risk of infection would be effectively controlled. Moreover, a secondary transmission risk would hardly occur.
However, different countries had various attitudes towards wearing masks during the COVID-19 pandemic due to their culture and customs. After the outbreak of COVID-19, mainland China, Hong Kong, Taiwan, South Korea, and other Asian regions quickly responded to the national mask-wearing strategy (Feng et al. 2020). Whereas, some European, American, and Japanese administrative staff believed that there was little evidence that masks could effectively prevent respiratory infections, and thought that it was unnecessary to encourage the whole population to wear masks (Federal Ministry of Health, Germany 2020; National Health Service 2020). So it was hard to convince all the people to wear masks. Figure 9 simulates the R for an air-conditioned bus with the changing mask-wearing rate k. It can be concluded that: (1) despite the various mask types, R dramatically decreases with the increase mask-wearing rate, and any kind of masks can play significant roles in controlling the spread of the epidemic. (2) The larger mask-wearing rate can markedly reduce the transmission risk. Besides, when k is very small, the slight reduction of R has little effect on the prevention and control of the epidemic, which means the importance of calling on the entire population to wear masks.
Discussions
The impact of the bus scheduling on enclosed transportation
The air-conditioned bus is one of the most common public transportation for long and short trips, as well as commutes. The driving distance and number of passengers are relatively fixed regardless of a long trip or short trip, but city bus scheduling is fluctuating due to different time of a day and bus routes. In order to evaluate the impact of changes in travel time and number of passengers on a bus, this study used the transmission model to estimate the COVID-19 basic reproductive number R for air-conditioned buses under different bus scheduling, as shown in Figs. 10 and 11.
Figure 10 shows the variation of bus basic reproductive number R with the number of people at different exposure times. Assuming that the number of passengers n = 48, when the travel time is reduced from t = 2 h to t = 1 h, the bus basic reproductive number R would decrease from 7.68 to 3.82. The risk of infection is dramatically reduced. However, if the number of passengers is changed from n = 48 to n = 24, keeping the travel time t = 2 h fixed, the R would decrease from 7.68 to 6.57. Similarly, predictions were made for the minibus. Figure 11 shows the values of the minibus basic reproductive number R for different exposure times alongside the changing number of passengers. Assuming that the number of passengers n = 18 fixed and changing the travel time from t = 1 h to t = 0.5 h, the R would decrease from 3.52 to 1.65. It reduces the transmission risk more than 50%. However, curtailing the number of passengers from n = 18 to n = 9 while keeping the travel time t = 1 h, R shall be reduced by only about 24%. Thus, reducing the exposure time in closed traffic is more sensitive to the impact of infection risk than limiting the number of passengers.
However, it is not practical to change the traffic exposure time for fixed travel distances. Several applicable suggestions can be implemented during an outbreak. Firstly, the long-distance bus of each day can be appropriately reduced. Secondly, regulate passengers to sit at intervals so as to limit the total population in vehicle. Thirdly, add rest-stops and ask all the passengers to get off the car for air in order to reduce the risk of transmission. That way, if a bus is running 1 h with 10 people, the basic reproductive number R would go from 7.7 to 2. Nevertheless, it should be pointed out that in the case of city buses most passengers will not ride for a long time, usually 15 to 30 min, and the occupants getting on and off at each station are random. Such uncertain factors work together, making it difficult to accurately predict the situation through the model. Yet, according to Fig. 10, even if the number of passengers is reduced from 48 to 24, the basic reproductive number R of SARS-CoV-2 only decreases by 15.9%. The transmission risk is still very high. To conclude, exposure time on a city bus, to a large extent, determines the risk of infection rather than the number of passengers on board. The basic reproductive number R is about 0.5 for a 15-min ride and 1.5 for 30 min. It can be deduced that taking a bus within 30 min, the infection risk may be relatively low, according to the definition of the basic reproductive number R, discussed in the “Transmission Model” section.
Mask efficiency outward and inward
The above three types of mask filtration efficiency were calculated based the cited papers in the “The mask intervention” section. Among those papers, the experiments designed for evaluating mask efficiency can be divided into outward experiments and inward experiments. Outward defines that the mask wearing contains outgoing particles to the environment, while inward refers to the effect of mask on protecting an individual from incoming particles. Accordingly, the inward efficiency of mask is better than the outward (Van der Sande et al. 2008).
The outward scenario is more suitable for mask-wearing patients in a public occasion, which can prevent the outside environment from pollution, especially in confined space. Because for some respiratory pandemic, the coarse aerosols are researched to be generated at the upper respiratory tract while the fine aerosols reflected infection in the lung (Leung et al. 2020). They are independent; thus, the viral load in the fine aerosol are 8.8-fold more than that in coarse aerosols (Milton et al. 2013). For example, sneezes will generate abundant large droplets (Yan et al. 2018), which are likely to cause close and indirect contact transmission, and wearing surgical masks can reduce large aerosol by 25-fold. Even if surgical masks reduce fine aerosol by only 2.8-fold compared to large aerosol, it can reduce overall 3.4-fold of viral aerosol shedding (Milton et al. 2013). But there are differences in the effectiveness of masks against diverse viruses. Surgical masks seem to be more efficient for both coarse aerosols and fine aerosols of coronavirus (Leung et al. 2020). Therefore, in the public transportation, patients wearing surgical masks could reduce the emission of exhaled particles into the environment.
The inward scenario refers to the individual who has a risk in staying in the pathogen-load aerosol environment, especially for the health-care workers. Surgical masks cannot prevent all the aerosol from penetrating through the masks, and the leak of submicrometer-size aerosols may also curtail the protective factor (Weber et al. 1993). The leakage characteristics are related with different types of surgical masks. Even if, the surgical masks can achieve the reduction factor from 1 to 55, an average of 6 (Health and Safety Executive UK 2008; Makison Booth et al. 2013). Homemade masks perform less efficient than surgical masks, especially preventing fine aerosols from penetrating. As the exposure time becomes longer, wearing surgical masks keeps a relative stable efficiency, while homemade masks perform gradually better, narrowing the gap between surgical masks. Therefore, homemade masks may still achieve important protection degree, even though they perform less strong than surgical masks. Besides, homemade masks can be made in ordinary families, which will not be constricted by limited supplies. As can be seen, for the reproductive number of minibus which may not be very high, equal to 3.07, a small reduction in transmissibility by wearing homemade masks may be sufficient for decreasing the reproduction number to 1.01, achieving 67% improvement in the epidemic prevention, nearly controlling the transmission. Greater reduction may be achieved for the COVID-19 that is predominantly carried by large droplets (Van der Sande et al. 2008; Wenzhao Chen et al. 2020; World Health Organization 2020).
Even though, authorities and academics have no clear guidelines on the wearing of types of masks under different conditions (Roberge 2016). According to the masks efficiency discussed from inward and outward protection, if both the patient and susceptible individuals wear surgical masks in an enclosed environment, the infection risks will dramatically decrease. For the time when masks limited provide, homemade masks could also confer a significant degree of protection, even though they are less strong than surgical masks. From a public health point of view, mask is not the single resort of interventions, but to integrate all effective interventions for an optimal protection.
As to the health-care workers who normally have situations in close exposure to an infectious aerosol environment, considering the leakage of surgical masks and less protection against fine aerosols, it is better for them to wear correctly fitting masks together with visors, N95 masks, or higher level respiratory protection, which can substantially curtail short-range exposure and long-term exposure to infectious aerosols (Makison Booth et al. 2013; Lindsley et al. 2014).
Limitations and outlook
The premise of the Wells-Riley model is the assumption that the air is well mixed which means all the susceptible people have the same infection risk. So far, there is no method available that can estimate the quanta from an outbreak other than the assumption. Even if we have used the revised Wells-Riley equation, taking spatial variation into consideration, the survival of viruses in the air is full of uncertainty and complexity, which shows it is unreasonable that the quanta value stays unchanged along time. Hence, in order to improve the model, future work should pay more attention to the virus survival study under different environments together with their aerodynamic characteristics.
As to the masks, additional studies can explore mask protection efficiency against different groups of people. Since fine aerosols generation correlates with health conditions, ages, and the virus type also has an effect on masks. Taking the heterogeneous performances of diverse masks into an estimation model, future recommendations for infection control could be critically evaluated for different groups of people based on a specific virus.
Conclusions
This study developed an innovative approach for estimating the SARS-CoV-2 epidemiological parameters “quanta” in confined spaces by applying the daily confirmed cases on the Diamond Princess Cruise Ship. With the calculated “quanta,” we also predicted the basic reproductive number R of SARS-CoV-2 for air-conditioned buses through the Wells-Riley model. Finally, we quantitatively evaluated the mitigation strategies for transportation transmission risk of COVID-19 and personal protection measures by simulating different mask-wearing modes, highlighting the role of wearing masks as one of the public interventions. Our study can be incorporated into the interdisciplinary field among engineering, virology, epidemiology, and indoor environment for better understanding of the complex dynamic environment. This information could also provide key theoretical support for the related departments to conduct control strategies and for scholars to optimize relevant models. The main conclusions drawn from this study are summarized as follows:
-
(1)
The median value of the SARS-CoV-2 quantum generation rate in an enclosed vehicle space is 185.63 according to the daily number of new confirmed cases reported on the Diamond Princess Cruise Ship.
-
(2)
An increase in the number of passengers slightly increases the infection risks, while the longer exposure time in a confined traffic space can heavily increase the risks. In other words, reducing the passenger exposure time in an enclosed vehicle space is more effective than curtailing the number of passengers in regard to the impact on the infection risk. Hence, it is advisable to reduce the frequencies of long-distance driving with crowded people during the outbreak. However, for this study, less than 30 min exposure in public transportation is relatively low for the infection risk.
-
(3)
It is necessary to advocate wearing masks in public transportation. A large mask-wearing percentage plays a significant role in achieving successful reduction of the transmission risk.
References
Adam J Kucharski, Russell TW, Diamond C, Liu Y, Edmunds J, Funk S, Eggo RM (2020) Early dynamics of transmission and control of COVID-19: a mathematical modelling study. medRxiv
Buonanno G, Morawska L, Stabile L (2020a) Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: prospective and retrospective applications. Environ Int 145:106112
Buonanno G, Stabile L, Morawska L (2020b) Estimation of airborne viral emission: quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ Int 141:105794
Chen S, Chang C, Liao C (2006) Predictive models of control strategies involved in containing indoor airborne infections. Indoor Air 16:469–481
Chenari B, Dias Carrilho J, Gameiro Da Silva M (2016) Towards sustainable, energy-efficient and healthy ventilation strategies in buildings: a review. Renew Sust Energ Rev 59:1426–1447
Coronavirus Resource Center ,Johns Hopkins University (2020) COVID-19 Case Tracker
Correia G, Rodrigues L, Gameiro Da Silva M, Gonçalves T (2020) Airborne route and bad use of ventilation systems as non-negligible factors in SARS-CoV-2 transmission. Med Hypotheses 141:109781
Davies A, Thompson K, Giri K, Kafatos G, Walker J, Bennett A (2013) Testing the efficacy of homemade masks: would they protect in an influenza pandemic? DISASTER MED PUBLIC 7:413–418
Federal Ministry Of Health,Germany. (2020). Daily updates on the coronavirus: is wearing a surgical mask, as protection against acute respiratory infections, useful for members of the general public?
Feng S, Shen C, Xia N, Song W, Fan M, Cowling BJ (2020) Rational use of face masks in the COVID-19 pandemic. Lancet Respir Med 8:434–436
FURUYA H (2007) Risk of transmission of airborne infection during train commute based on mathematical model. ENVIRON HEALTH PREV 12:78–83
G N Sze To, Christopher Yu Hang Chao (2010) Review and comparison between the Wells-Riley and dose-response approaches to risk assessment of infectious respiratory diseases. Indoor Air 20:2–16
Ghinai I, Woods S, Ritger KA, McPherson TD, Black SR, Sparrow L, Fricchione MJ, Kerins JL, Pacilli M, Ruestow PS, Arwady MA, Beavers SF, Payne DC, Kirking HL, Layden JE (2020) Community transmission of SARS-CoV-2 at two family gatherings—Chicago, Illinois, February-March 2020. MMWR-MORBID MORTAL W 69:446–450
Grossman D (2020) As COVID-19 cases rise, a mental health epidemic among frontline healthcare workers may be growing as well. The denver channel
Guo Z, Wang Z, Zhang S, Li X, Li L, Li C, Cui Y, Fu R, Dong Y, Chi X, Zhang M, Liu K, Cao C, Liu B, Zhang K, Gao Y, Lu B, Chen W (2020) Aerosol and surface distribution of severe acute respiratory syndrome coronavirus 2 in hospital wards, Wuhan, China, 2020. Emerg Infect Dis 26:1583–1591
Health and Safety Executive UK (2008) Evaluating the protection afforded by surgical masks against influenza bioaerosols
Hua Q, Xiaohong Z, Xuejun Z (2012) Prediction of risk of airborne transmitted diseases. Journal of Southeast University (Natural Science) 42:468–472
International Organization for Standardization (2002) Ships and marine technology—air conditioning and ventilation of accommodation spaces—design conditions and basis of calculations, ISO 7547. International Organization for Standardization, Geneva, p 8
Inthavong K, Ge QJ, Li XD, Tu JY (2012) Detailed predictions of particle aspiration affected by respiratory inhalation and airflow. Atmos Environ 62:107–117
Jiang Y, Wang H, Chen Y, He J, Chen L, Liu Y et al (2020) Clinical data on hospital environmental hygiene monitoring and medical staffs protection during the coronavirus disease 2019 outbreak. medRxiv
Jianyun L, Jieni G, Kuibiao L, Conghui X, Wenzhe S, Zhisheng L, Deqian Z, Chao Y, Bin X, Zhicong Y (2020) COVID-19 outbreak associated with air conditioning in restaurant, Guangzhou, China, 2020. Emerg Infect Dis 26:1628–1631
Junzhou H, Ziwe Z, Xudong Y (2020) Ventilation!Ventilation?From prevention and control of SARS in 2003 to COVID-19 transmission on “Diamond princess” cruise in 2020. Heating Ventilation & Conditioning 50:86–90
Klepeis NE, Nelson WC, Ott WR, Robison JP, Tsang AM, Switzer P, Behar JV, Hern SC, Engelmann WH (2001) The National Human Activity Pattern Survey (NHAPS): a resource for assessing exposure to environmental pollutants. J Exposure Sci Environ Epidemiol 11:231–252
Lee S, Grinshpun SA, Reponen T (2008) Respiratory performance offered by N95 respirators and surgical masks: human subject evaluation with NaCl aerosol representing bacterial and viral particle size range. The Annals of Occupational Hygiene 52:177–185
Leung NHL, Chu DKW, Shiu EYC, Chan K, McDevitt JJ, Hau BJP, Yen H, Li Y, Ip DKM, Peiris JSM, Seto W, Leung GM, Milton DK, Cowling BJ (2020) Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 26:676–680
Liao C, Chang C, Liang H (2005) A probabilistic transmission dynamic model to assess indoor airborne infection risks. Risk Anal 25:1097–1107
Liao CM, Chen SC, Chang CF (2008) Modelling respiratory infection control measure effects. Epidemiol Infect 136:299–308
Lindsley WG, Noti JD, Blachere FM, Szalajda JV, Beezhold DH (2014) Efficacy of Face Shields Against Cough Aerosol Droplets from a Cough Simulator. J Occup Environ Hyg 11(8):509–518
Makison Booth C, Clayton M, Crook B, Gawn JM (2013) Effectiveness of surgical masks against influenza bioaerosols. J HOSP INFECT 84:22–26
Milton DK, Fabian MP, Cowling BJ, Grantham ML, McDevitt JJ (2013) Influenza virus aerosols in human exhaled breath: particle size, culturability, and effect of surgical masks. PLoS Pathog 9:e1003205
Ministry of Health, Labor and Welfare,Japan (2020) 横浜港で検疫中のクルーズ船内で確認された新型コロナウイルス感染症について[About new coronavirus infectious diseases confirmed on cruise ships quarantine in Yokohama Port]
Ministry of Transport of The People’s Republic of China (2014) Type dividing and class rating for public bus , JT/T 888–2014, first ed ed. China Communications Press Co.,Ltd, Beijing,China, p 13
Mizumoto K, Chowell G (2020) Transmission potential of the novel coronavirus (COVID-19) onboard the diamond princess cruises ship, 2020. Infectious Disease Modelling 5:264–270
Morawska L, Cao J (2020) Airborne transmission of SARS-CoV-2: the world should face the reality. Environ Int 139:105730
Morawska L, Johnson GR, Ristovski ZD, Hargreaves M, Mengersen K, Corbett S, Chao CYH, Li Y, Katoshevski D (2009) Size distribution and sites of origin of droplets expelled from the human respiratory tract during expiratory activities. J Aerosol Sci 40:256–269
Morawska L, Tang JW, Bahnfleth W, Bluyssen PM, Boerstra AC, Buonanno G, Cao J, Dancer S, Floto A, Franchimon F, Haworth C, Hogeling J, Isaxon C, Jiminez JL, Kurnitski J, Li Y, Loomans MGLC, Marks G, Marr LC, Mazzarella L, Melikov A, Miller S, Milton DK, Nazaroff W, Nielsen PV, Noakes C, Peccia J, Querol X, Sekhar C, Seppänen O, Tanabe S, Tellier R, Tham KW, Wargocki P, Wierzbicka A, Yao M (2020) How can airborne transmission of COVID-19 indoors be minimised? Environ Int 142:105832
Moriarty LF, Plucinski MM, Marston BJ, Kurbatova EV, Knust B, Murray EL, Pesik N, Rose D, Fitter D, Kobayashi M, Toda M, Canty PT, Scheuer T, Halsey ES, Cohen NJ, Stockman L, Wadford DA, Medley AM, Green G, Regan JJ, Tardivel K, White S, Brown C, Morales C, Yen C, Wittry B, Freeland A, Naramore S, Novak RT, Daigle D, Weinberg M, Acosta A, Herzig C, Kapella BK, Jacobson KR, Lamba K, Ishizumi A, Sarisky J, Svendsen E, Blocher T, Wu C, Charles J, Wagner R, Stewart A, Mead PS, Kurylo E, Campbell S, Murray R, Weidle P, Cetron M, Friedman CR, Behravesh CB, Bjork A, Bower W, Bozio C, Braden Z, Bertulfo MC, Chatham-Stephens K, Chu V, Cooper B, Dooling K, Dubray C, Curren E, Honein MA, Ivey K, Jones J, Kadzik M, Knight N, Marlow M, McColloch A, McDonald R, Klevos A, Poser S, Rinker RA, Ritter T, Rodriguez L, Ryan M, Schneider Z, Shockey C, Shugart J, Silver M, Smith PW, Tobolowsky F, Treffiletti A, Wallace M, Yoder J, Barry P, Berumen R, Bregman B, Campos K, Chai S, Glenn-Finer R, Guevara H, Hacker J, Hsieh K, Morris MK, Murphy R, Myers JF, Padilla T, Pan C, Readhead A, Saguar E, Salas M, Snyder RE, Vugia D, Watt J, Wong C, Acosta M, Davis S, Kapuszinsky B, Matyas B, Miller G, Ntui A, Richards J (2020) Public health responses to COVID-19 outbreaks on cruise ships—worldwide, February–March 2020. MMWR. Morb Mortal Wkly Rep 69:347–352
National Academies Of Sciences EAM (2020) Rapid expert consultation on the possibility of bioaerosol spread of SARS-CoV-2 for the COVID-19 pandemic (April 1, 2020). The National Academies Press, Washington, DC
National Health Service (2020) Are face masks useful for preventing coronavirus? 2020
National Institute Of Infectious Diseases (2020) Field briefing: Diamond Princess COVID-19 Cases, 20 Feb Update
Neeltje Van Doremalen, Bushmaker T, Morris DH, Holbrook M, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloydsmith JO, De Wit E, Munster VJ (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. NEW ENGL J MED 382:1564–1567
NOISH, National Institute for Occupational Safety and Health (n.d.) Respiratory Protective Equipment Standard Certification, 42CF-84
Noti JD, Lindsley WG, Blachere FM, Cao G, Kashon ML, Thewlis RE, McMillen CM, King WP, Szalajda JV, Beezhold DH (2012) Detection of infectious influenza virus in cough aerosols generated in a simulated patient examination room. Clin Infect Dis 54:1569–1577
Olsen SJ, Chang H, Cheung TY, Tang AF, Fisk TL, Ooi SP, Kuo H, Jiang DD, Chen K, Lando J, Hsu K, Chen T, Dowell SF (2003) Transmission of the severe acute respiratory syndrome on aircraft. NEW ENGL J MED 349:2416–2422
Park SY, Kim Y, Yi S, Lee S, Na B, Kim CB, Kim J, Kim HS, Kim YB, Park Y, Huh IS, Kim HK, Yoon HJ, Jang H, Kim K, Chang Y, Kim I, Lee H, Gwack J, Kim SS, Kim M, Kweon S, Choe YJ, Park O, Park YJ, Jeong EK (2020) Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis 26:1666–1670
Qian H, Zhang CY, Zheng XH (2018) The function of aerosols in transmitting and infecting of respiratory infectious diseases and its risk prediction. Chin Sci Bull 63:931–939
Read R (2020) A choir decided to go ahead with rehearsal. Now dozens of members have COVID-19 and two are dead, Los Angeles Times
Riley EC, Murphy G, Riley RL (1978) Airborne spread of measles in a suburban elementary school. Am J Epidemiol 107:421–432
Roberge RJ (2016) Face shields for infection control: a review. J Occup Environ Hyg 13:235–242
Rudnick SN, Milton DK (2003) Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air 13:237–245
Sun C, Zhai Z (2020) The efficacy of social distance and ventilation effectiveness in preventing COVID-19 transmission. Sustain Cities Soc 62:102390
Tellier R, Li Y, Cowling BJ, Tang JW (2019) Recognition of aerosol transmission of infectious agents: a commentary. BMC Infect Dis 19:101
Van der Sande M, Teunis P, Sabel R (2008) Professional and home-made face masks reduce exposure to respiratory infections among the general population. PLoS One 3:e2618
Vega JA (2020) PRCC head urges Vázquez to refrain from a general lockdown, implement restrictions focused on hot spots; Says SMEs are on the edge due to crisis, Caribbean Business
Vessel Tracker (2020) Advanced masterdata for the vessel Diamond Princess
Weber A, Willeke K, Marchloni R, Myojo T, Mckay R, Donnelly J, Liebhaber F (1993) Aerosol penetration and leakae characteristics of masks used in the health care industry. Am J Infect Control 21:167–173
Wenzhao Chen, Zhang N, JianjianWei H-LY, YuguoLi (2020) Short-range airborne route dominates exposure of respiratory 4 infection during close contact. Build Environ 176:106859
William Firth Wells (1955) Airborne contagion and air hygiene. Harvard University Press, Cambridge, MA
World Health Organization (2020) Coronavirus disease (COVID-19): how is it transmitted?
Wu JT, Leung K, Leung GM (2020) Nowcasting and forecasting the potential domestic and international spread of the 2019-nCoV outbreak originating in Wuhan, China: a modelling study. Lancet 395:689–697
Yan J, Grantham M, Pantelic J, Bueno De Mesquita PJ, Albert B, Liu F, Ehrman S, Milton DK (2018) Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc Natl Acad Sci 115:1081–1086
Zhang N, Huang H, Su B, Ma X, Li Y (2018) A human behavior integrated hierarchical model of airborne disease transmission in a large city. Build Environ 127:211–220
Zhang N, Chen W, Chan PT, Yen HL, Tang JWT, Li Y (2020) Close contact behavior in indoor environment and transmission of respiratory infection. Indoor Air 30:645–661
Acknowledgments
We thank the MOE Key Laboratory of Deep Earth Science and Engineering, Institute for Disaster Management and Reconstruction at Sichuan University and Hong Kong Polytechnic University for providing technical support.
Availability of data and materials
The datasets generated/or analyzed during the current study are available from the corresponding author on reasonable request.
Funding
We thank the National Natural Science Foundation of China (No. 51478280 & 51778382), and The Sichuan Science and Technology Program (No. 2019YFS0051&2020YFS0439) for providing technical support.
Author information
Authors and Affiliations
Contributions
Linlin Chen did the conceptualization, data curation, formal analysis, methodology validation, and writing. Guangze Ban did the simulation and analyzed the data. Enshen Long did the conceptualization and supervision. Gretchen Kalonji did the supervision and visualization. Zhu Cheng did the supervision and technical support. Li Zhang did the supervision. Shurui Guo did the visualization.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Chen, L., Ban, G., Long, E. et al. Estimation of the SARS-CoV-2 transmission probability in confined traffic space and evaluation of the mitigation strategies. Environ Sci Pollut Res 28, 42204–42216 (2021). https://doi.org/10.1007/s11356-021-13617-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-021-13617-y