Abstract
Background
Obstructive sleep apnea (OSA) is the most common form of sleep-disordered breathing in cerebrovascular diseases, requiring a multidisciplinary approach. There are few studies evaluating the effects of inspiratory muscle training (IMT) in individuals with OSA and the findings regarding the possible effect on apnea hypopnea index (AHI) reduction are controversial.
Objective
This protocol for a randomized clinical trial will assess the effects of IMT on the severity of obstructive sleep apnea, sleep quality, and daytime sleepiness in individuals after stroke participating in a rehabilitation program.
Methods
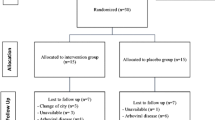
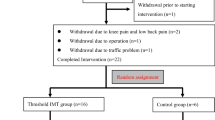
This study will be a randomized controlled trial with blinded assessors. Forty individuals after stroke will randomized to two groups. For 5 weeks, both groups will participate in the rehabilitation program activities, including aerobic exercise, resistance training, and educational class when they will receive guidance on the behavioral management of OSA. The experimental group will also perform high-intensity IMT 5 times a week, for 5 weeks, consisting initially of five sets of five repetitions achieving 75% of the maximal inspiratory pressure, increasing one set each week, totaling nine sets at the end of training. The primary outcome will be the severity of OSA measured as AHI at 5 weeks. Secondary outcomes will include sleep quality measured by the Pittsburgh Sleep Quality Index (PSQI) and daytime sleepiness measured by Epworth Sleepiness Scale (ESS). Outcomes will be collected by a researcher blinded to group allocation at baseline (week 0), after intervention (week 5), and 1 month beyond intervention (week 9).
Trial registration
Clinical Trials Register: NCT05135494.


Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to why dates are not public but are available from the corresponding author on reasonable request.
References
Johnson KG, Johnson DC (2010) Frequency of sleep apnea in stroke and TIA patients: a meta-analysis. J Clin sleep Med JCSM Off Publ Am Acad Sleep Med 6:131–137
Seiler A, Camilo M, Korostovtseva L et al (2019) Prevalence of sleep-disordered breathing after stroke and TIA. Neurology 92:e648–e654. https://doi.org/10.1212/WNL.0000000000006904
Bassetti CLA, Randerath W, Vignatelli L et al (2020) EAN/ERS/ESO/ESRS statement on the impact of sleep disorders on risk and outcome of stroke. Eur J Neurol 27:1117–1136. https://doi.org/10.1111/ene.14201
Dong JY, Zhang YH, Qin LQ (2013) Obstructive sleep apnea and cardiovascular risk: meta-analysis of prospective cohort studies. Atherosclerosis 229:489–495
Aaronson JA, Van Bennekom CAM, Hofman WF et al (2015) Obstructive sleep apnea is related to impaired cognitive and functional status after stroke. Sleep 38:1431-1437B. https://doi.org/10.5665/sleep.4984
Kernan WN, Ovbiagele B, Black HR et al (2014) Guidelines for the prevention of stroke in patients with stroke and transient ischemic attack: a guideline for healthcare professionals from the American Heart Association. Stroke 45:2160–2236. https://doi.org/10.1161/STR.0000000000000024
Sateia MJ (2014) International classification of sleep disorders-third edition: highlights and modifications. Chest 146(5):1387–1394
Eckert DJ (2018) Phenotypic approaches to obstructive sleep apnoea –new pathways for targeted therapy. Sleep Med Rev 37:45–59. https://doi.org/10.1016/j.smrv.2016.12.003
Chien MY, Wu YT, Lee PL et al (2010) Inspiratory muscle dysfunction in patients with severe obstructive sleep apnoea. Eur Respir J 35:373–380. https://doi.org/10.1183/09031936.00190208
Colelli DR, Kamra M, Rajendram P et al (2020) Predictors of CPAP adherence following stroke and transient ischemic attack. Sleep Med 66:243–249. https://doi.org/10.1016/j.sleep.2018.10.009
Patil SP, Ayappa IA, Caples SM et al (2019) Treatment of adult obstructive sleep apnea with positive airway pressure: an American Academy of Sleep Medicine Clinical Practice Guideline. J Clin Sleep Med 15:335–343. https://doi.org/10.5664/jcsm.7640
Menezes KKKP, Nascimento LR, Ada L et al (2016) Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. J Physiother 62:138–144. https://doi.org/10.1016/j.jphys.2016.05.014
How SC, McConnell AK, Taylor BJ, Romer LM (2007) Acute and chronic responses of the upper airway to inspiratory loading in healthy awake humans: an MRI study. Respir Physiol Neurobiol 157:270–280. https://doi.org/10.1016/j.resp.2007.01.008
Chen T-A, Mao S-T, Lin H-C et al (2022) Effects of inspiratory muscle training on blood pressure- and sleep-related outcomes in patients with obstructive sleep apnea: a meta-analysis of randomized controlled trials. Sleep Breath. https://doi.org/10.1007/s11325-022-02773-1
Azeredo LM de, Souza LC de, Guimarães BLS, Puga FP, Behrens NSCS, Lugon JR (2022) Inspiratory muscle training as adjuvant therapy in obstructive sleep apnea: a randomized controlled trial. Braz J Med Biol Res 55:e12331. https://doi.org/10.1590/1414-431X2022e12331
Dar JA, Mujaddadi A, Moiz JA (2022) Effects of inspiratory muscle training in patients with obstructive sleep apnoea syndrome: a systematic review and meta-analysis. Sleep Sci (Sao Paulo, Brazil) 15:480–489. https://doi.org/10.5935/1984-0063.20220081
Nóbrega-Júnior JCN, Dornelas de Andrade A, de Andrade EAM et al (2020) Inspiratory muscle training in the severity of obstructive sleep apnea, sleep quality and excessive daytime sleepiness: a placebo-controlled, randomized trial. Nat Sci Sleep 12:1105–1113. https://doi.org/10.2147/NSS.S269360
Lin HC, Chiang LL, Ong JH et al (2020) The effects of threshold inspiratory muscle training in patients with obstructive sleep apnea: a randomized experimental study. Sleep Breath 24:201–209. https://doi.org/10.1007/s11325-019-01862-y
Sateia MJ (2014) International Classification of Sleep Disorders-Third Edition. Chest 146:1387–1394. https://doi.org/10.1378/chest.14-0970
ATS (2002) ATS/ERS Statement on respiratory muscle testing. Am J Respir Crit Care Med 166:518–624. https://doi.org/10.1164/rccm.166.4.518
Britto RR, Rezende NR, Marinho KC et al (2011) Inspiratory muscular training in chronic stroke survivors: a randomized controlled trial. Arch Phys Med Rehabil 92:184–190. https://doi.org/10.1016/j.apmr.2010.09.029
Buysse DJ, Reynolds CF, Monk TH et al (1989) The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213. https://doi.org/10.1016/0165-1781(89)90047-4
Bertolazi AN, Fagondes SC, Hoff LS et al (2009) Validação da escala de sonolência de Epworth em português para uso no Brasil. J Bras Pneumol 35:877–883
Kuo Y-C, Song T-T, Bernard JR, Liao Y-H (2017) Short-term expiratory muscle strength training attenuates sleep apnea and improves sleep quality in patients with obstructive sleep apnea. Respir Physiol Neurobiol 243:86–91. https://doi.org/10.1016/j.resp.2017.05.007
POWERbreathe International Limited (2020) POWERbreathe Medic Plus. In: POWERbreathe. https://www.powerbreathe.com/powerbreathe-medic-plus
Ferreira STBP, do Socorro Brasileiro-Santos M, Teixeira JB, et al (2022) Clinical safety and hemodynamic, cardiac autonomic and inflammatory responses to a single session of inspiratory muscle training in obstructive sleep apnea. Sleep Breath 26:99–108. https://doi.org/10.1007/s11325-021-02364-6
Parreiras de Menezes KK, Nascimento LR, Ada L et al (2019) High-intensity respiratory muscle training improves strength and dyspnea poststroke: a double-blind randomized trial. Arch Phys Med Rehabil 100:205–212. https://doi.org/10.1016/j.apmr.2018.09.115
Zhang XX, Zheng Y, Dang Y et al (2020) Can inspiratory muscle training benefit patients after stroke? A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil 34:866–876. https://doi.org/10.1177/0269215520926227
Pozuelo-Carrascosa DP, Carmona-Torres JM, Laredo-Aguilera JA et al (2020) Effectiveness of respiratory muscle training for pulmonary function and walking ability in patients with stroke: a systematic review with meta-analysis. Int J Environ Res Public Health 17:1–22. https://doi.org/10.3390/ijerph17155356
Sapienza CM, Wheeler K (2006) Respiratory muscle strength training: functional outcomes versus plasticity. Semin Speech Lang 27:236–244. https://doi.org/10.1055/s-2006-955114
Vaz L de O, Almeida J de C, Froes KS dos SO, et al (2021) Effects of inspiratory muscle training on walking capacity of individuals after stroke: a double-blind randomized trial. Clin Rehabil 35:1247–1256. https://doi.org/10.1177/0269215521999591
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
de Oliveira Vaz, L., Galvão, A.P., Nunes, D.L.M. et al. Effects of inspiratory muscle training on the severity of obstructive sleep apnea in individuals after stroke: a protocol for a randomized controlled trial. Sleep Breath 27, 2257–2263 (2023). https://doi.org/10.1007/s11325-023-02825-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-023-02825-0