Abstract
Purpose
Drug-induced sedation endoscopy (DISE) and simulated snoring (SimS) can locate the site of obstruction in patients with sleep-disordered breathing (SDB). There is clinical evidence for a change in collapsibility of the upper airway depending on the depth of sedation. So far, a dose-response relationship between sedation and collapsibility has not been demonstrated.
Methods
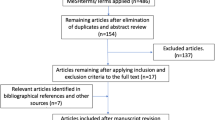
DISE and SimS were performed in 60 consecutive patients with SDB under monitoring of depth of sedation by BiSpectral Index® (BIS). Initially, SimS was conducted followed by DISE using bolus application of propofol. Sedation was performed up to a sedation level representing slow wave sleep (BIS = 40). The collapsibility of the upper airway was documented at decreasing sedation levels by an identical pictogram classification.
Results
For all levels and patterns of obstruction, a dose-dependent increase in the collapsibility of the upper airway was detected. A maximum collapsibility was achieved at sedation levels representing slow wave sleep. The collapsibility during SimS corresponded to light sleep stages and did not cover slow wave sleep.
Conclusion
A dose-dependent change of patterns of obstructions can be observed during DISE under BIS monitoring indicating sedation depth. The obtained patterns of obstruction during DISE and SimS should thus be interpreted with regard to the sedation depth.






Similar content being viewed by others
References
Croft CB, Pringle M (1991) Sleep nasendoscopy: a technique of assessment in snoring and obstructive sleep apnoea. Clin Otolaryngol Allied Sci 16(5):504–509
Pringle MB, Croft CB (1993) A grading system for patients with obstructive sleep apnoea—based on sleep nasendoscopy. Clin Otolaryngol Allied Sci 18(6):480–484
De Vito A, Carrasco Llatas M, Vanni A, Bosi M, Braghiroli A, Campanini A, de Vries N, Hamans E, Hohenhorst W, Kotecha BT, Maurer J, Montevecchi F, Piccin O, Sorrenti G, Vanderveken OM, Vicini C (2014) European position paper on drug-induced sedation endoscopy (DISE). Sleep Breath 18(3):453–465. doi:10.1007/s11325-014-0989-6
Kotecha BT, Hannan SA, Khalil HM, Georgalas C, Bailey P (2007) Sleep nasendoscopy: a 10-year retrospective audit study. Eur Arch Otorhinolaryngol 264(11):1361–1367. doi:10.1007/s00405-007-0366-1
Gillespie MB, Reddy RP, White DR, Discolo CM, Overdyk FJ, Nguyen SA (2013) A trial of drug-induced sleep endoscopy in the surgical management of sleep-disordered breathing. Laryngoscope 123(1):277–282. doi:10.1002/lary.23506
Fernandez-Julian E, Garcia-Perez MA, Garcia-Callejo J, Ferrer F, Marti F, Marco J (2014) Surgical planning after sleep versus awake techniques in patients with obstructive sleep apnea. Laryngoscope 124(8):1970–1974. doi:10.1002/lary.24577
Cho JS, Soh S, Kim EJ, Cho HJ, Shin S, Kim HJ, Koo BN (2015) Comparison of three sedation regimens for drug-induced sleep endoscopy. Sleep & breathing = Schlaf & Atmung 19(2):711–717. doi:10.1007/s11325-015-1127-9
Ehsan Z, Mahmoud M, Shott SR, Amin RS, Ishman SL (2015) The effects of anesthesia and opioids on the upper airway: a systematic review. Laryngoscope. doi:10.1002/lary.25399
Atkins JH, Mandel JE, Rosanova G (2014) Safety and efficacy of drug-induced sleep endoscopy using a probability ramp propofol infusion system in patients with severe obstructive sleep apnea. Anesth Analg 119(4):805–810. doi:10.1213/ANE.0000000000000229
Eastwood PR, Platt PR, Shepherd K, Maddison K, Hillman DR (2005) Collapsibility of the upper airway at different concentrations of propofol anesthesia. Anesthesiology 103(3):470–477
Abdullah VJ, Lee DL, Ha SC, van Hasselt CA (2013) Sleep endoscopy with midazolam: sedation level evaluation with bispectral analysis. Otolaryngol Head Neck Surg 148(2):331–337. doi:10.1177/0194599812464865
Borek RC, Thaler ER, Kim C, Jackson N, Mandel JE, Schwab RJ (2012) Quantitative airway analysis during drug-induced sleep endoscopy for evaluation of sleep apnea. Laryngoscope 122(11):2592–2599. doi:10.1002/lary.23553
Hong SD, Dhong HJ, Kim HY, Sohn JH, Jung YG, Chung SK, Park JY, Kim JK (2013) Change of obstruction level during drug-induced sleep endoscopy according to sedation depth in obstructive sleep apnea. Laryngoscope 123(11):2896–2899. doi:10.1002/lary.24045
Berry RB, Budhiraja R, Gottlieb DJ, Gozal D, Iber C, Kapur VK, Marcus CL, Mehra R, Parthasarathy S, Quan SF, Redline S, Strohl KP, Davidson Ward SL, Tangredi MM (2012) Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 8(5):597–619. doi:10.5664/jcsm.2172
Herzog M, Metz T, Schmidt A, Bremert T, Venohr B, Hosemann W, Kaftan H (2006) The prognostic value of simulated snoring in awake patients with suspected sleep-disordered breathing: introduction of a new technique of examination. Sleep 29(11):1456–1462
Campanini A, Canzi P, De Vito A, Dallan I, Montevecchi F, Vicini C (2010) Awake versus sleep endoscopy: personal experience in 250 OSAHS patients. Acta Otorhinolaryngol Ital 30(2):73–77
Cavaliere M, Russo F, Iemma M (2013) Awake versus drug-induced sleep endoscopy: evaluation of airway obstruction in obstructive sleep apnea/hypopnoea syndrome. Laryngoscope 123(9):2315–2318
Rabelo FA, Kupper DS, Sander HH, Santos Junior V, Thuler E, Fernandes RM, Valera FC (2013) A comparison of the Fujita classification of awake and drug-induced sleep endoscopy patients. Braz J Otorhinolaryngol 79(1):100–105
Lo YL, Ni YL, Wang TY, Lin TY, Li HY, White DP, Lin JR, Kuo HP (2015) Bispectral index in evaluating effects of sedation depth on drug-induced sleep endoscopy. J Clin Sleep Med 11(9):1011–1020. doi:10.5664/jcsm.5016
Nieuwenhuijs D, Coleman EL, Douglas NJ, Drummond GB, Dahan A (2002) Bispectral index values and spectral edge frequency at different stages of physiologic sleep. Anesth Analg 94 (1):125–129, table of contents
Sleigh JW, Andrzejowski J, Steyn-Ross A, Steyn-Ross M (1999) The bispectral index: a measure of depth of sleep? Anesth Analg 88(3):659–661
Dahaba AA, Xue JX, Xu GX, Liu QH, Metzler H (2011) Bilateral Bispectral Index (BIS)-Vista as a measure of physiologic sleep in sleep-deprived anesthesiologists. Minerva Anestesiol 77(4):388–393
Babar-Craig H, Rajani NK, Bailey P, Kotecha BT (2012) Validation of sleep nasendoscopy for assessment of snoring with bispectral index monitoring. Eur Arch Otorhinolaryngol 269(4):1277–1279. doi:10.1007/s00405-011-1798-1
Miner JR, Biros MH, Heegaard W, Plummer D (2003) Bispectral electroencephalographic analysis of patients undergoing procedural sedation in the emergency department. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine 10(6):638–643
Miner JR, Biros MH, Seigel T, Ross K (2005) The utility of the bispectral index in procedural sedation with propofol in the emergency department. Academic emergency medicine: official journal of the Society for Academic Emergency Medicine 12(3):190–196. doi:10.1197/j.aem.2004.10.004
Herzog M, Kellner P, Plossl S, Glien A, Rohrmeier C, Kuhnel T, Plontke S, Herzog B (2015) Drug-induced sleep endoscopy and simulated snoring in patients with sleep-disordered breathing: agreement of anatomic changes in the upper airway. Eur Arch Otorhinolaryngol. doi:10.1007/s00405-015-3559-z
Acknowledgments
The technical assistance provided by Annett Christel (Dept. of Anaesthesiology and Surgical Intensive Care, Martin-Luther-University Halle-Wittenberg) is gratefully acknowledged.
Parts of this investigation were presented at the German Anaesthesia Congress (DAC) 2013, Nürnberg, Germany and at the annual meeting of the German Society of Oto-Rhino-Laryngology, Head and Neck Surgery, 2013 Nürnberg, Germany.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no competing interests.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Funding
No funding was received for this research.
Statement of human rights and ethical approval
All procedures performed in our study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. A corresponding ethical approval was given by the institutional ethics board (ethic board ID: 2011–55), and the study was registered at the German Medical Trial Register (DRKS-ID: DRKS00004560).
Rights and permissions
About this article
Cite this article
Kellner, P., Herzog, B., Plößl, S. et al. Depth-dependent changes of obstruction patterns under increasing sedation during drug-induced sedation endoscopy: results of a German monocentric clinical trial. Sleep Breath 20, 1035–1043 (2016). https://doi.org/10.1007/s11325-016-1348-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-016-1348-6