Abstract
Objectives
Prior to oral appliance therapy for snoring and obstructive sleep apnea syndrome (OSAS), patients are screened for jaw symptoms (e.g., pain). However, the presence of jaw symptoms in a large spectrum of OSAS patients remains unknown. This study aimed to assess the distribution of subjective jaw symptoms in patients with symptoms of OSAS.
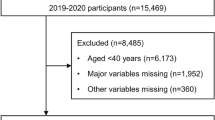
Methods
Five hundred and eleven consecutive patients (66 female, 445 male; mean age 49.6 ± 12.6 years) with clinical symptoms of OSAS were enrolled for cardiorespiratory evaluation. Self-administered questionnaires were used to assess jaw symptoms, tooth grinding and clenching during sleep, morning oral dryness, morning heartburn sensation, and pain in the neck and back.
Results
The mean apnea–hypopnea (AHI) index was 32.5 ± 30.6 per hour of sleep. Nineteen percent of patients (n = 96) reported at least one jaw symptom. The presence of jaw symptoms was more frequently reported by patients with AHI less than 15 (25 %) than those with AHI of 15 and more (15 %, p = 0.012). In the crude analyses, jaw symptoms were associated with tooth grinding, tooth clenching, morning oral dryness, morning heartburn sensation, and neck/back pain. Multiple logistic regression analysis confirmed that jaw symptoms were associated with AHI less than 15 (odds ratio (OR) 1.99, p = 0.009), tooth clenching (OR 1.79, p = 0.006), morning oral dryness (OR 2.17, p = 0.02), and neck/back pain (OR 1.99, p = 0.005).
Conclusions
Jaw symptoms can be found in 19 % of patients with symptoms of OSAS and are more frequently reported in patients with lower AHI, a patient population for whom oral appliances are often prescribed.
Similar content being viewed by others
References
Ferguson KA (2003) The role of oral appliance therapy in the treatment of obstructive sleep apnea. Clin Chest Med 24(2):355–364
Ferguson KA, Lowe AA (2005) Oral appliances for sleep-disordered breathing. In: Kryger MH, Roth T, Dement WC (eds) Principles and practices of sleep medicine, 4th edn. Elsevier Saunders, Philadelphia, pp 1098–1108
Hoffstein V (2007) Review of oral appliances for treatment of sleep-disordered breathing. Sleep Breath 11(1):1–22
Schmidt-Nowara W (1999) Recent developments in oral appliance therapy of sleep disordered breathing. Sleep Breath 3(3):103–106
Pantin CC, Hillman DR, Tennant M (1999) Dental side effects of an oral device to treat snoring and obstructive sleep apnea. Sleep 22(2):237–240
Clark GT, Sohn JW, Hong CN (2000) Treating obstructive sleep apnea and snoring: assessment of an anterior mandibular positioning device. J Am Dent Assoc 131(6):765–771
McGown AD, Makker HK, Battagel JM, L'Estrange PR, Grant HR, Spiro SG (2001) Long-term use of mandibular advancement splints for snoring and obstructive sleep apnoea: a questionnaire survey. Eur Respir J 17(3):462–466
Fritsch KM, Iseli A, Russi EW, Bloch KE (2001) Side effects of mandibular advancement devices for sleep apnea treatment. Am J Respir Crit Care Med 164(5):813–818
de Almeida FR, Lowe AA, Tsuiki S, Otsuka R, Wong M, Fastlicht S, Ryan F (2005) Long-term compliance and side effects of oral appliances used for the treatment of snoring and obstructive sleep apnea syndrome. J Clin Sleep Med 1(2):143–152
Tsuda H, Almeida FR, Masumi SI, Lowe AA (2010) Side effects of boil and bite type oral appliance therapy in sleep apnea patients. Sleep Breath 14(3):227–232
Doff MH, Veldhuis SK, Hoekema A, Slater JJ, Wijkstra PJ, de Bont LG, Stegenga B (2012) Long-term oral appliance therapy in obstructive sleep apnea syndrome: a controlled study on temporomandibular side effects. Clin Oral Investig. doi:10.1007/s00784-011-0555-6
Fransson AM, Tegelberg A, Johansson A, Wenneberg B (2004) Influence on the masticatory system in treatment of obstructive sleep apnea and snoring with a mandibular protruding device: a 2-year follow-up. Am J Orthod Dentofacial Orthop 126(6):687–693
Giannasi LC, Almeida FR, Magini M, Costa MS, de Oliveira CS, de Oliveira JC, Kalil Bussadori S, de Oliveira LV (2009) Systematic assessment of the impact of oral appliance therapy on the temporomandibular joint during treatment of obstructive sleep apnea: long-term evaluation. Sleep Breath 13(4):375–381
Martinez-Gomis J, Willaert E, Nogues L, Pascual M, Somoza M, Monasterio C (2010) Five years of sleep apnea treatment with a mandibular advancement device. Side effects and technical complications. Angle Orthod 80(1):30–36
Fransson AM, Isacsson G, Leissner LC, Nasman AB, Alton MK (2001) Treatment of snoring and obstructive sleep apnea with a mandibular protruding device: an open-label study. Sleep Breath 5(1):23–33
Petit FX, Pepin JL, Bettega G, Sadek H, Raphael B, Levy P (2002) Mandibular advancement devices: rate of contraindications in 100 consecutive obstructive sleep apnea patients. Am J Respir Crit Care Med 166(3):274–278
Gold AR, Dipalo F, Gold MS, O'Hearn D (2003) The symptoms and signs of upper airway resistance syndrome: a link to the functional somatic syndromes. Chest 123(1):87–95
Oksenberg A, Froom P, Melamed S (2006) Dry mouth upon awakening in obstructive sleep apnea. J Sleep Res 15(3):317–320
Blanco J, Zamarron C, Abeleira Pazos MT, Lamela C, Suarez Quintanilla D (2005) Prospective evaluation of an oral appliance in the treatment of obstructive sleep apnea syndrome. Sleep Breath 9(1):20–25
Fransson AM, Tegelberg A, Leissner L, Wenneberg B, Isacsson G (2003) Effects of a mandibular protruding device on the sleep of patients with obstructive sleep apnea and snoring problems: a 2-year follow-up. Sleep Breath 7(3):131–141
American Academy of Sleep Medicine (2005) International classification of sleep disorders: diagnostic and coding manual, 2nd edn. American Academy of Sleep Medicine, Westchester
Chesson AL Jr, Berry RB, Pack A (2003) Practice parameters for the use of portable monitoring devices in the investigation of suspected obstructive sleep apnea in adults. Sleep 26(7):907–913
Collop NA, Anderson WM, Boehlecke B, Claman D, Goldberg R, Gottlieb DJ, Hudgel D, Sateia M, Schwab R (2007) Clinical guidelines for the use of unattended portable monitors in the diagnosis of obstructive sleep apnea in adult patients. Portable Monitoring Task Force of the American Academy of Sleep Medicine. J Clin Sleep Med 3(7):737–747
Carmelli D, Colrain IM, Swan GE, Bliwise DL (2004) Genetic and environmental influences in sleep-disordered breathing in older male twins. Sleep 27(5):917–922
Emsellem HA, Corson WA, Rappaport BA, Hackett S, Smith LG, Hausfeld JN (1990) Verification of sleep apnea using a portable sleep apnea screening device. South Med J 83(7):748–752
Redline S, Tishler PV, Tosteson TD, Williamson J, Kump K, Browner I, Ferrette V, Krejci P (1995) The familial aggregation of obstructive sleep apnea. Am J Respir Crit Care Med 151(3 Pt 1):682–687
Kato T, Velly AM, Nakane T, Masuda T, Maki S (2012) Age is associated with self-reported sleep bruxism, independently of tooth loss. Sleep Breath. doi:10.1007/s11325-011-0625-7
Cunali PA, Almeida FR, Santos CD, Valdrighi NY, Nascimento LS, Dal'Fabbro C, Tufik S, Bittencourt LR (2009) Prevalence of temporomandibular disorders in obstructive sleep apnea patients referred for oral appliance therapy. J Orofac Pain 23(4):339–344
Smith MT, Wickwire EM, Grace EG, Edwards RR, Buenaver LF, Peterson S, Klick B, Haythornthwaite JA (2009) Sleep disorders and their association with laboratory pain sensitivity in temporomandibular joint disorder. Sleep 32(6):779–790
Onen SH, Onen F, Albrand G, Decullier E, Chapuis F, Dubray C (2010) Pain tolerance and obstructive sleep apnea in the elderly. J Am Med Dir Assoc 11(9):612–616
Khalid I, Roehrs TA, Hudgel DW, Roth T (2011) Continuous positive airway pressure in severe obstructive sleep apnea reduces pain sensitivity. Sleep 34(12):1687–1691
Lautenbacher S, Kundermann B, Krieg JC (2006) Sleep deprivation and pain perception. Sleep Med Rev 10(5):357–369
Choinieré M, Racine M, Raymond-Shaw I (2007) Epidemiology of pain and sleep disturbances and their reciprocal interrelationships. In: Lavigne GJ, Sessle BJ, Choinieré M, Soja PJ (eds) Sleep and pain. IASP, Seattle, pp 267–284
Lavigne GJ, Smith MT, Denis R, Zucconi M (2011) Pain and sleep. In: Kryger MH, Roth T, Dement WC (eds) Principles and practices of sleep medicine, 5th edn. Elsevier Saunders, Philadelphia, pp 1442–1451
Kino K, Sugisaki M, Haketa T, Amemori Y, Ishikawa T, Shibuya T, Sato F, Amagasa T, Tanabe H, Yoda T, Sakamoto I, Omura K, Miyaoka H (2005) The comparison between pains, difficulties in function, and associating factors of patients in subtypes of temporomandibular disorders. J Oral Rehabil 32(5):315–325
Velly AM, Gornitsky M, Philippe P (2003) Contributing factors to chronic myofascial pain: a case–control study. Pain 104(3):491–499
Lavigne GJ, Khoury S, Abe S, Yamaguchi T, Raphael K (2008) Bruxism physiology and pathology: an overview for clinicians. J Oral Rehabil 35(7):476–494
Lobbezoo F, Lavigne GJ (1997) Do bruxism and temporomandibular disorders have a cause-and-effect relationship? J Orofac Pain 11(1):15–23
Kato T, Lavigne GJ (2010) Sleep bruxism: a sleep related movement disorder. Sleep Med Clin 5(1):9–35
Ohayon MM, Li KK, Guilleminault C (2001) Risk factors for sleep bruxism in the general population. Chest 119(1):53–61
Phillips BA, Okeson J, Paesani D, Gilmore R (1986) Effect of sleep position on sleep apnea and parafunctional activity. Chest 90(3):424–429
Sjoholm TT, Lowe AA, Miyamoto K, Fleetham JA, Ryan CF (2000) Sleep bruxism in patients with sleep-disordered breathing. Arch Oral Biol 45(10):889–896
Camparis CM, Siqueira JT (2006) Sleep bruxism: clinical aspects and characteristics in patients with and without chronic orofacial pain. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(2):188–193
Rompre PH, Daigle-Landry D, Guitard F, Montplaisir JY, Lavigne GJ (2007) Identification of a sleep bruxism subgroup with a higher risk of pain. J Dent Res 86(9):837–842
Kato T (2004) Sleep bruxism and its relation to obstructive sleep apnea–hypopnea syndrome. Sleep Biol Rhyth 2(1):1–15
Thie NM, Kato T, Bader G, Montplaisir JY, Lavigne GJ (2002) The significance of saliva during sleep and the relevance of oromotor movements. Sleep Med Rev 6(3):213–227
da Silva LA, Teixeira MJ, de Siqueira JT, de Siqueira SR (2011) Xerostomia and salivary flow in patients with orofacial pain compared with controls. Arch Oral Biol 56(10):1142–1147
Haack M, Mullington JM (2005) Sustained sleep restriction reduces emotional and physical well-being. Pain 119(1–3):56–64
Kamisaka M, Yatani H, Kuboki T, Matsuka Y, Minakuchi H (2000) Four-year longitudinal course of TMD symptoms in an adult population and the estimation of risk factors in relation to symptoms. J Orofac Pain 14(3):224–232
LeBlanc M, Merette C, Savard J, Ivers H, Baillargeon L, Morin CM (2009) Incidence and risk factors of insomnia in a population-based sample. Sleep 32(8):1027–1037
Sipila K, Suominen AL, Alanen P, Heliovaara M, Tiittanen P, Kononen M (2011) Association of clinical findings of temporomandibular disorders (TMD) with self-reported musculoskeletal pains. Eur J Pain 15(10):1061–1067
Sipila K, Zitting P, Siira P, Laukkanen P, Jarvelin MR, Oikarinen KS, Raustia AM (2002) Temporomandibular disorders, occlusion, and neck pain in subjects with facial pain: a case–control study. Cranio 20(3):158–164
Cunali PA, Almeida FR, Santos CD, Valdrichi NY, Nascimento LS, Dal-Fabbro C, Tufik S, Bittencourt LR (2011) Mandibular exercises improve mandibular advancement device therapy for obstructive sleep apnea. Sleep Breath 15(4):717–727
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kato, T., Mikami, A., Sugita, H. et al. Negative association between self-reported jaw symptoms and apnea–hypopnea index in patients with symptoms of obstructive sleep apnea syndrome: a pilot study. Sleep Breath 17, 373–379 (2013). https://doi.org/10.1007/s11325-012-0704-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0704-4