Abstract
Purpose
The purpose of this study was to evaluate associations between obstructive sleep apnea (OSA) severity and self-reported sleepiness and daytime functioning in patients considering bariatric surgery for treatment of obesity.
Methods
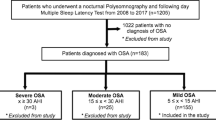
Using a retrospective cohort design, we identified 342 patients who had sleep evaluations prior to bariatric surgery. Our final sample included 269 patients (78.6 % of the original cohort, 239 females; mean age = 42.0 ± 9.5 years; body mass index = 50.2 ± 7.7 kg/m2) who had overnight polysomnography and completed the Epworth Sleepiness Scale (ESS) and the Functional Outcomes of Sleep Questionnaire (FOSQ). Patients' OSA was classified as none/mild (apnea–hypopnea index (AHI) < 15, n = 112), moderate (15 ≤ AHI < 30, n = 77), or severe (AHI ≥ 30, n = 80). We calculated the proportion of unique variance (PUV) for the five FOSQ subscales. ANOVA was used to determine if ESS and FOSQ were associated with OSA severity. Unpaired t tests compared ESS and FOSQ scores in our sample with published data.
Results
The average AHI was 29.5 ± 31.5 events per hour (range = 0–175.8). The mean ESS score was 6.3 ± 4.8, and the mean global FOSQ score was 100.3 ± 18.2. PUVs for FOSQ subscales showed moderate-to-high unique contributions to FOSQ variance. ESS and global FOSQ score did not differ by AHI group. Only the FOSQ vigilance subscale differed by OSA severity with the severe group reporting more impairment than the moderate and none/mild groups. Our sample reported less sleepiness and daytime impairment than previously reported means in patients and controls.
Conclusions
Subjective sleepiness and functional impairment were not associated significantly with OSA severity in our sample of patients considering surgery for obesity. Further research is needed to understand individual differences in sleepiness in patients with OSA. If bariatric patients underreport symptoms, self-report measures are not an adequate substitute for objective assessment and clinical judgment when evaluating bariatric patients for OSA. Patients with severe obesity need evaluation for OSA even in the absence of subjective complaints.


Similar content being viewed by others
References
Sergi M, Rizzi M, Comi AL, Resta O, Palma P, De Stefano A, Comi D (1999) Sleep apnea in moderate-severe obese patients. Sleep Breath 3:47–52
Frey WC, Pilcher J (2003) Obstructive sleep-related breathing disorders in patients evaluated for bariatric surgery. Obes Surg 13:676–683
Serafini FM, MacDowell Anderson W, Rosemurgy AS, Strait T, Murr MM (2001) Clinical predictors of sleep apnea in patients undergoing bariatric surgery. Obes Surg 11:28–31
O'Keeffe T, Patterson EJ (2004) Evidence supporting routine polysomnography before bariatric surgery. Obes Surg 14:23–26
Sareli AE, Cantor CR, Williams NN, Korus G, Raper SE, Pien G, Hurley S, Maislin G, Schwab RJ (2011) Obstructive sleep apnea in patients undergoing bariatric surgery—a tertiary center experience. Obes Surg 21:316–327
Carneiro G, Florio RT, Zanella MT, Pradella-Hallinan M, Ribeiro-Filho FF, Tufik S, Togeiro SM (2011) Is mandatory screening for obstructive sleep apnea with polysomnography in all severely obese patients indicated? Sleep Breath. doi:10.1007/s11325-010-0468-7
Malone S, Liu PP, Holloway R, Rutherford R, Xie A, Bradley TD (1991) Obstructive sleep apnoea in patients with dilated cardiomyopathy: effects of continuous positive airway pressure. Lancet 338:1480–1484
Peker Y, Carlson J, Hedner J (2006) Increased incidence of coronary artery disease in sleep apnoea: a long-term follow-up. Eur Respir J 28:596–602
Peppard PE, Young T, Palta M, Skatrud J (2000) Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med 342:1378–1384
Arzt M, Young T, Finn L, Skatrud JB, Bradley TD (2005) Association of sleep-disordered breathing and the occurrence of stroke. Am J Respir Crit Care Med 172:1447–1451
Gross JB, Bachenberg KL, Benumof JL, Caplan RA, Connis RT, Cote CJ, Nickinovich DG, Prachand V, Ward DS, Weaver EM, Ydens L, Yu S (2006) Practice guidelines for the perioperative management of patients with obstructive sleep apnea: a report by the American Society of Anesthesiologists Task Force on Perioperative Management of patients with obstructive sleep apnea. Anesthesiology 104:1081–1093
Meoli AL, Rosen CL, Kristo D, Kohrman M, Gooneratne N, Aguillard RN, Fayle R, Troell R, Kramer R, Casey KR, Coleman J Jr (2003) Upper airway management of the adult patient with obstructive sleep apnea in the perioperative period–avoiding complications. Sleep 26:1060–1065
Loube DI, Erman MK, Reed W (1997) Perioperative complications in obstructive sleep apnea patients. Sleep Breath 2:3–10
Flum DR, Belle SH, King WC, Wahed AS, Berk P, Chapman W, Pories W, Courcoulas A, McCloskey C, Mitchell J, Patterson E, Pomp A, Staten MA, Yanovski SZ, Thirlby R, Wolfe B (2009) Perioperative safety in the longitudinal assessment of bariatric surgery. N Engl J Med 361:445–454
Shafazand S (2009) Perioperative management of obstructive sleep apnea: ready for prime time? Cleve Clin J Med 76(Suppl 4):S98–S103
Chung SA, Yuan H, Chung F (2008) A systemic review of obstructive sleep apnea and its implications for anesthesiologists. Anesth Analg 107:1543–1563
Kump K, Whalen C, Tishler PV, Browner I, Ferrette V, Strohl KP, Rosenberg C, Redline S (1994) Assessment of the validity and utility of a sleep-symptom questionnaire. Am J Respir Crit Care Med 150:735–741
Maislin G, Pack AI, Kribbs NB, Smith PL, Schwartz AR, Kline LR, Schwab RJ, Dinges DF (1995) A survey screen for prediction of apnea. Sleep 18:158–166
Chung F, Yegneswaran B, Liao P, Chung SA, Vairavanathan S, Islam S, Khajehdehi A, Shapiro CM (2008) STOP questionnaire: a tool to screen patients for obstructive sleep apnea. Anesthesiology 108:812–821
Dixon JB, Schachter LM, O'Brien PE (2003) Predicting sleep apnea and excessive day sleepiness in the severely obese: indicators for polysomnography. Chest 123:1134–1141
Gafsou B, Marsac L, Fournier J, Beloucif S, Baillard C (2010) Validation of the STOP-Bang questionnaire as screening tools for obstructive sleep apnea in patients scheduled for bariatric surgery. Eur J Anaesthesiol 27:13
D'Ambrosio C, Bowman T, Mohsenin V (1999) Quality of life in patients with obstructive sleep apnea: effect of nasal continuous positive airway pressure–a prospective study. Chest 115:123–129
Dixon JB, Dixon ME, Anderson ML, Schachter L, O'Brien PE (2007) Daytime sleepiness in the obese: not as simple as obstructive sleep apnea. Obesity (Silver Spring) 15:2504–2511
Grunstein RR, Stenlof K, Hedner JA, Sjostrom L (1995) Impact of self-reported sleep-breathing disturbances on psychosocial performance in the Swedish Obese Subjects (SOS) Study. Sleep 18:635–643
Pan A, Sun Q, Czernichow S, Kivimaki M, Okereke OI, Lucas M, Manson JE, Ascherio A, Hu FB (2011) Bidirectional association between depression and obesity in middle-aged and older women. Int J Obes (Lond). doi:10.1038/ijo.2011.111
Cameron AJ, Magliano DJ, Dunstan DW, Zimmet PZ, Hesketh K, Peeters A, Shaw JE (2011) A bi-directional relationship between obesity and health-related quality of life: evidence from the longitudinal AusDiab study. Int J Obes (Lond). doi:10.1038/ijo.2011.103
Bixler EO, Vgontzas AN, Lin HM, Calhoun SL, Vela-Bueno A, Kales A (2005) Excessive daytime sleepiness in a general population sample: the role of sleep apnea, age, obesity, diabetes, and depression. J Clin Endocrinol Metab 90:4510–4515
Johns MW (1993) Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest 103:30–36
Weaver TE, Laizner AM, Evans LK, Maislin G, Chugh DK, Lyon K, Smith PL, Schwartz AR, Redline S, Pack AI, Dinges DF (1997) An instrument to measure functional status outcomes for disorders of excessive sleepiness. Sleep 20:835–843
Granger C (1984) A conceptual model for functional assessment. In: Granger C, Gresham G (eds) Functional assessment in rehabilitation medicine. Williams and Wilkins, Baltimore, pp 14–25
Johns MW (1992) Reliability and factor analysis of the Epworth Sleepiness Scale. Sleep 15:376–381
Gooneratne NS, Weaver TE, Cater JR, Pack FM, Arner HM, Greenberg AS, Pack AI (2003) Functional outcomes of excessive daytime sleepiness in older adults. J Am Geriatr Soc 51:642–649
Rechtschaffen A, Kales A (1968) A manual of standardized terminology, techniques, and scoring system for sleep stages in human subjects. UCLA Brain Information Service/Brain Research Institute, Los Angeles
American Academy of Sleep Medicine (1999) Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Report of the American Academy of Sleep Medicine Task Force. Sleep 22:667–689
American Academy of Sleep Medicine (1992) EEG arousals: scoring rules and examples: a preliminary report from the Sleep Disorders Atlas Task Force of the American Sleep Disorders Association. Sleep 15:173–184
Seifer R, Sameroff A, Barrett L, Krafchuk E (1994) Infant temperament measured by multiple observations and mother report. Child Dev 65:1478–1490
Sharma SK, Kurian S, Malik V, Mohan A, Banga A, Pandey RM, Handa KK, Mukhopadhyay S (2004) A stepped approach for prediction of obstructive sleep apnea in overtly asymptomatic obese subjects: a hospital based study. Sleep Med 5:351–357
Chung F, Ward B, Ho J, Yuan H, Kayumov L, Shapiro C (2007) Preoperative identification of sleep apnea risk in elective surgical patients, using the Berlin questionnaire. J Clin Anesth 19:130–134
Sharkey KM, Machan JT, Tosi C, Roye GD, Harrington D, Millman RP (2010) Predicting obstructive sleep apnea among women candidates for bariatric surgery. J Womens Health (Larchmt) 19:1833–1841
Foster GD, Sanders MH, Millman R, Zammit G, Borradaile KE, Newman AB, Wadden TA, Kelley D, Wing RR, Sunyer FX, Darcey V, Kuna ST (2009) Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care 32:1017–1019
Hoy CJ, Vennelle M, Kingshott RN, Engleman HM, Douglas NJ (1999) Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am J Respir Crit Care Med 159:1096–1100
Elias MF, Elias PK, Sullivan LM, Wolf PA, D'Agostino RB (2003) Lower cognitive function in the presence of obesity and hypertension: the Framingham heart study. Int J Obes Relat Metab Disord 27:260–268
Gunstad J, Strain G, Devlin MJ, Wing R, Cohen RA, Paul RH, Crosby RD, Mitchell JE (2010) Improved memory function 12 weeks after bariatric surgery. Surg Obes Relat Dis 7:465–472
Benbadis SR, Mascha E, Perry MC, Wolgamuth BR, Smolley LA, Dinner DS (1999) Association between the Epworth sleepiness scale and the multiple sleep latency test in a clinical population. Ann Intern Med 130:289–292
Chervin RD, Aldrich MS (1999) The Epworth Sleepiness Scale may not reflect objective measures of sleepiness or sleep apnea. Neurology 52:125–131
Cruz IA, Drummond M, Winck JC (2011) Obstructive sleep apnea symptoms beyond sleepiness and snoring: effects of nasal APAP therapy. Sleep Breath. doi:10.1007/s11325-011-0502-4
Punjabi NM, Bandeen-Roche K, Young T (2003) Predictors of objective sleep tendency in the general population. Sleep 26:678–683
Jimenez-Correa U, Haro R, Gonzalez-Robles RO, Velazquez-Moctezuma J (2011) How is the Epworth Sleepiness Scale related with subjective sleep quality and polysomnographic features in patients with sleep-disordered breathing? Sleep Breath 15:513–518
Gander PH, Marshall NS, Harris R, Reid P (2005) The Epworth Sleepiness Scale: influence of age, ethnicity, and socioeconomic deprivation. Epworth sleepiness scores of adults in New Zealand. Sleep 28:249–253
Jackson ML, Stough C, Howard ME, Spong J, Downey LA, Thompson B (2011) The contribution of fatigue and sleepiness to depression in patients attending the sleep laboratory for evaluation of obstructive sleep apnea. Sleep Breath 15:439–445
Acknowledgments
The authors thank the polysomnographic technologists and clerical staff at the Sleep Disorders Center for their excellent work with our patients.
Conflicts
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sharkey, K.M., Orff, H.J., Tosi, C. et al. Subjective sleepiness and daytime functioning in bariatric patients with obstructive sleep apnea. Sleep Breath 17, 267–274 (2013). https://doi.org/10.1007/s11325-012-0685-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11325-012-0685-3