Abstract
Previous studies suggest that adenosine A1 receptors (A1R) modulate the processing of pain. The aim of this study was to characterize the distribution of A1R in nociceptive tissues and to evaluate whether targeting A1R with the partial agonist capadenoson may reduce neuropathic pain in mice. The cellular distribution of A1R in dorsal root ganglia (DRG) and the spinal cord was analyzed using fluorescent in situ hybridization. In behavioral experiments, neuropathic pain was induced by spared nerve injury or intraperitoneal injection of paclitaxel, and tactile hypersensitivities were determined using a dynamic plantar aesthesiometer. Whole-cell patch-clamp recordings were performed to assess electrophysiological properties of dissociated DRG neurons. We found A1R to be expressed in populations of DRG neurons and dorsal horn neurons involved in the processing of pain. However, administration of capadenoson at established in vivo doses (0.03–1.0 mg/kg) did not alter mechanical hypersensitivity in the spared nerve injury and paclitaxel models of neuropathic pain, whereas the standard analgesic pregabalin significantly inhibited the pain behavior. Moreover, capadenoson failed to affect potassium currents in DRG neurons, in contrast to a full A1R agonist. Despite expression of A1R in nociceptive neurons, our data do not support the hypothesis that pharmacological intervention with partial A1R agonists might be a valuable approach for the treatment of neuropathic pain.
Similar content being viewed by others
Introduction
Traumatic injuries, surgical insults and damages of peripheral nerves often lead to neuropathic pain, a chronic debilitating disease that affects 7–10% of the general population and is associated with great impairment of quality of life [1]. However, more than half of neuropathic pain patients report inadequate pain relief with currently available medications, and these are often associated with severe dose-limiting side effects. Therefore, there is a large unmet therapeutic need for effective and safe treatment of neuropathic pain [2,3,4].
Neuropathic pain is associated with multiple alterations in the peripheral and central nervous system [5, 6]. Accumulating evidence indicates that the nucleoside adenosine contributes to the processing of neuropathic pain [7, 8]. In general, adenosine interacts with four G protein-coupled receptors, A1R, A2AR, A2BR and A3R, which in turn affect the activity of various ion channels and enzymes [9]. Among the adenosine receptors, A1R has gained interest in pain research. Previous studies reported that A1R is expressed in both peripheral and central sites of the nociceptive system, although the cellular distribution remains controversial [10,11,12,13]. Several lines of evidence indicate the functional contribution of A1R to neuropathic pain processing. For example, mice lacking A1R globally demonstrated increased pain behaviors in models of neuropathic pain [14]. Increasing adenosine levels by delivery of ectonucleotidases that dephosphorylate adenosine 5′-monophosphate to adenosine is associated with potent, long-lasting, and A1R-dependent antinociceptive effects [15, 16]. Furthermore, administration of A1R agonists such as N6-cyclopentyladenosine (CPA) or 5’-chloro-5’deoxy-( ±)-ENBA (Cl-ENBA) ameliorated neuropathic pain in various animal models (for review, see [7]).
Although numerous full A1R agonists have been developed, clinical applications of these agents have been hampered by unintended pharmacological effects including sedation, motor impairment, bradycardia and atrioventricular blocks [17, 18]. These unwanted effects can be overcome by partial A1R agonists, which trigger only some of the physiological responses of receptor activation depending on endogenous adenosine levels and on receptor reserve in different tissues [19]. Partial A1R agonists might therefore hypothetically ameliorate neuropathic pain in an effective and safe manner. Among the selective and potent partial A1R agonists is capadenoson, which belongs to the non-adenosine dicyanopyridine class of compounds. Capadenoson shows EC50 values of 0.1 nM on A1R, a selectivity factor of 1800 and 900 versus A2AR and A2BR, respectively, and no significant activity on A3R [19]. Furthermore, it exhibits good pharmacokinetic parameters with sufficient bioavailability after oral administration [18, 19]. The primary objectives of the study were to characterize the cellular distribution of A1R in nociceptive tissues and to investigate whether targeting A1R using the partial agonist capadenoson might inhibit neuropathic pain in mice.
Material and methods
Animals
All experiments were performed in C57BL/6 N mice of either sex (6–12 weeks old) obtained from Charles River Laboratories (Sulzfeld, Germany). Animals were housed on a 12 h light/dark cycle with access to food and water ad libitum. All behavioral studies were carried out by observers blinded for treatment of the animals. All experiments were ethically reviewed and approved by our local Ethics Committee for Animal Research (Regierungspräsidium Darmstadt, Germany). They adhered to the IASP (International Association for the Study of Pain) and ARRIVE (Animal Research: Reporting on In Vivo Experiments) guidelines and conformed to Directive 2010/63/EU. All efforts were made to minimize animal suffering and to reduce the number of animals used.
Neuropathic pain models
The spared nerve injury (SNI) model [20] was used to investigate neuropathic pain behavior after surgically induced peripheral nerve injury. Animals were treated with carprofen (5 mg/kg, s.c.) 30 min prior to surgery to provide perioperative and postoperative analgesia. Under isoflurane anesthesia, two branches of the sciatic nerve were ligated and cut distally, leaving the sural nerve intact. This procedure leads to a hypersensitivity of the lateral surface (sural nerve skin area) of the affected hindpaw.
The paclitaxel model of neuropathy was used to mimic chemotherapy-induced neuropathic pain behavior. Animals received four i.p. injections of 1 mg/kg paclitaxel on days 0, 2, 4 and 6 (cumulative dose 4 mg/kg; [21]. Paclitaxel (Sigma Aldrich, Germany) was dissolved in a vehicle composed of Cremophor EL and absolute ethanol (1:1) and was further diluted in 0.9% NaCl [22, 23].
Mechanical sensitivity of the hindpaw was measured using a Dynamic Plantar Aesthesiometer (Ugo Basile, Italy). This device pushes a thin steel rod against the plantar surface of the paw from beneath, and automatically stops and records the latency time until the animal withdraws the paw. The force increased constantly from 0 to 5 g in 10 s (ramp 0.5 g/s) and remained at 5 g for an additional 10 s [23,24,25]. The paw withdrawal latency was calculated as the mean of 4–5 consecutive measurements with at least 20 s in between. Baseline measurements of mechanical sensitivity were performed 2 and 1 days before SNI surgery or paclitaxel injections. To ensure full development of neuropathic pain, mechanical sensitivity of the hindpaw was determined 13 or 20 days after SNI and 6 days after the last paclitaxel injection. One day thereafter, capadenoson (provided by Bayer AG, Germany, and purchased from MedChemExpress, USA), pregabalin (Bertin, France and Neuraxpharm, Germany), or vehicle (85% PEG400 and 15% glycerol; both from Carl Roth, Germany) were administered by oral gavage, whereas in another set of experiments capadenoson, N-Bicyclo[2.2.1]hept-2-yl-5'-chloro-5'-deoxyadenosine (CL-ENBA; Tocris, UK) or vehicle (60% PEG400 in water; Carl Roth, Germany) were administered by tail vein injection. The mechanical sensitivity of the ipsilateral hindpaw was determined over 24 h after drug administration.
In situ hybridization
Mice were killed by CO2 inhalation and perfused with 4% formaldehyde (PFA) in phosphate-buffered saline (PBS) for 5 min. Lumbar (L4-L5) spinal cords and lumbar (L4-L5) DRGs were dissected, post-fixed in PFA for 10 min, incubated in 20% sucrose in PBS overnight, and embedded in tissue freezing medium (Leica, Germany). Cryostat sections were cut at a thickness of 14 µm on a CryoStar NX50 device (Thermo Fisher Scientific, Germany). In situ hybridization (ISH) was performed using a QuantiGene ViewRNA Tissue Assay (Thermo Fisher Scientific, Germany) according to the manufacturer’s instructions and as previously described [26]. Briefly, probes for mouse Adora1 (diluted 1:40; NM_001039510.2, type 1 probe set, catalog # VB1-19,627, Thermo Fisher, Germany), Rbfox3 (diluted 1:40; NM_001039167.1, type 6 probe set, catalog # VB6-18,012) and scramble control (1:40; catalog # VF1-17,155) were incubated overnight at 40 °C (Thermobrite; Leica, Germany) followed by consecutive incubation with PreAmplifier Mix QT, Amplifier Mix QT, an alkaline phosphatase labeled probe against the Amplifier, AP Enhancer Solution, and Fast Red Substrate. Finally, sections were mounted with Fluoromount G (Southern Biotech, USA) or further processed for subsequent immunostaining.
In immunostaining experiments after in situ hybridization, sections were blocked in 10% normal goat serum (NGS), 3% bovine serum albumin (BSA) and 1% Triton X-100 in PBS for 1 h and incubated with primary antibodies overnight using rabbit anti-NF200 (1:2000; # N4142, Sigma-Aldrich, Germany) and rabbit anti-CGRP (1:800, # PC205C, Calbiochem, Germany). After rinsing in PBS, sections were incubated with secondary antibodies conjugated with Alexa Fluor 488 (Invitrogen/Life Technologies, USA) for 2 h at room temperature. For staining with Griffonia simplicifolia isolectin B4 (IB4), sections were incubated with AF488-labelled IB4 (# I21411, Invitrogen/Life Technologies, USA; dissolved 1:300 in PBS buffer containing 1 mM CaCl2, 1 mM MgCl2, 1 mM MnCl2, and 0.2% Triton X-100, pH 7.4) for 1 h at room temperature. Slides were coverslipped with Fluoromount G (Southern Biotech, USA). Images were taken using an Eclipse Ni-U microscope equipped with a monochrome DS-Qi2 camera (both from Nikon, Germany) and pseudocolored with the NIS Elements software (Nikon, Germany).
Cell counting
For quantification of A1R mRNA-positive sensory and dorsal horn neuron populations, serial sections of lumbar DRGs (L4-L5) and the lumbar spinal cord (L4–L5) from 3 mice were cut (14 µm). Per animal, ≥ 3 DRG sections at least 100 µm apart were counted manually (4837 cells in total). Only cells showing clear staining signals above background level, with a threshold set based on scramble control hybridization, were included. The percentage of CGRP-, IB4- and NF200-positive neurons is expressed as a proportion of marker-positive cells per total number of A1R-positive neurons. For calculation of the percentage of A1R-positive DRG neurons, the total number of DRG neuron somata was counted based on their autofluorescence visualized in the FITC channel.
DRG neuron culture
Mice (4–8 weeks old) were killed by CO2 inhalation and lumbar DRGs (L4-L5) were excised and transferred to HBSS (Thermo Fisher Scientific, USA). Following treatment with 2.5 U/ml dispase II and 500 U/ml collagenase IV (both from Roche, Switzerland) for 90 min and 0.05% Trypsin/EDTA (Thermo Fisher Scientific, USA) for 10 min, isolated cells were transferred onto coverslips coated with poly-d-lysine (250 μg/ml, Millipore, USA) and cultured in neurobasal medium supplemented with B27 (Thermo Fisher Scientific, USA), 100 μg/ml streptomycin and penicillin (Roth, Germany) at 37 °C and 5% CO2. Cells were used for experiments within 24 h after plating.
Electrophysiological recordings
Whole-cell voltage-clamp recordings on DRG neurons were performed at room temperature (20–22 °C), using an HEKA EPC 9 amplifier and Patchmaster software (HEKA Electronics, Germany). Offline analysis was performed using the Fitmaster software (HEKA Electronics, Germany) and GraphPad Prism 8. Micropipettes (3–5 MΩ) were pulled from borosilicate glass (Science Products, Germany) with a conventional micropipette puller (Model P-97, Sutter Instruments, USA). Potassium currents were measured by continuous perfusion of the external solution with clamp steps of 500 ms between -100 and + 120 mV starting from a 1000 ms prepulse at − 100 mV. The holding potential was − 70 mV. Current densities were normalized to the cell capacitance (pA/pF). The pipette solution contained (mM): KCl 140, MgCl2 2, EGTA 5, HEPES 10, MgATP 2, TrisGTP 1, pH 7.4 adjusted with KOH. The external solution contained (mM): NaCl 140, KCl 5, CaCl2 2, MgCl2 2, HEPES 10, pH 7.4 adjusted with NaOH. Capadenoson or CPA (Sigma-Aldrich, Germany), solved in external solution with a final concentration of 100 nM, were added to the bath without a continuous perfusion. Potassium currents were measured within 10 min after drug addition.
Statistical analysis
GraphPad Prism 8 software was used for statistical analysis. A two-way repeated-measures ANOVA with Bonferroni post hoc test was used to assess statistical significance. Changes with p < 0.05 were considered to be significant. All data are presented as mean ± SEM.
Results
Cellular distribution of adenosine A1 receptors in dorsal root ganglia and the spinal cord
We first investigated the cellular distribution of A1R mRNA in DRGs and the spinal cord using fluorescent in situ hybridization. In DRGs, we detected abundant hybridization signals (Fig. 1a), which were seen primarily in neuronal somata. Cell counting revealed that 60.7 ± 2.4% of DRG neurons express A1R mRNA. No hybridization signals were detected using a scramble control probe (Fig. 1b). To analyze the localization of A1R in DRG neuron subpopulations we combined in situ hybridization of A1R mRNA with immunostaining for established markers (Fig. 1c-f). Out of the A1R-positive neurons, 26.4 ± 2.9% coexpressed CGRP, a marker of peptidergic C fiber neurons, and 35.6 ± 3.0% bound IB4, a marker of non-peptidergic C fiber neurons. Furthermore, 45.7 ± 5.6% of A1R-positive neurons co-expressed NF200, which stains myelinated DRG neurons. These data suggest that A1R are expressed in both unmyelinated and myelinated DRG neurons of naive mice.
Distribution of adenosine A1 receptors (A1R) in dorsal root ganglia (DRG). a Fluorescent in situ hybridization detected A1R mRNA in mouse DRGs. b No hybridization signal was detected using a scramble control probe. c–e Fluorescent in situ hybridization of A1R mRNA combined with immunostaining of calcitonin gene-related peptide (CGRP; c), binding of isolectin B4 (IB4; d), or immunostaining of neurofilament-200 (NF200; e) revealed that A1R mRNA is expressed in populations of peptidergic and non-peptidergic C fibers and myelinated DRG neurons, respectively. f Quantitative summary of DRG neuron populations expressing A1R (2061 cells counted; n = 3 animals). Scale bars: 100 µm (a), 25 µm (c)
In the spinal cord, A1R mRNA was enriched in cells of the dorsal horn (Fig. 2a). No specific hybridization signal was detected using scramble control, as expected (Fig. 2b). Double-labeling in situ hybridization of A1R with the neuronal marker Rbfox3 (which produces the ‘neuronal nuclei’ antigen NeuN) revealed that virtually all A1R-positive cells co-express Rbfox3 (Fig. 2c), suggesting that A1R is mainly expressed in neurons in the dorsal horn of the spinal cord. Together, the expression of A1R in DRG neurons and dorsal horn neurons further supports its contribution to pain processing.
Distribution of adenosine A1 receptors (A1R) in the spinal cord. a Fluorescent in situ hybridization detected A1R mRNA primarily in the dorsal horn of mouse spinal cord. b No hybridization signal was detected using a scramble control probe. c Double-labeling in situ hybridization of A1R mRNA with mRNA of the neuronal marker Rbfox3 in the dorsal horn shows that A1R is mainly expressed by neurons. Scale bars: 500 µm (a), 50 µm (c)
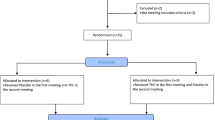
Treatment with capadenoson does not affect neuropathic pain behavior in mice
We next explored whether pharmacological activation of A1R might ameliorate neuropathic pain. For that purpose we tested whether treatment with the partial A1R agonist capadenoson affects mechanical hypersensitivity in two models of neuropathic pain in mice, i.e. the spared nerve injury (SNI) model of peripheral nerve injury and the paclitaxel model of chemotherapy-induced neuropathic pain. In a first set of experiments, we administered capadenoson perorally (p.o.) at three doses (0.03, 0.1 and 0.3 mg/kg). We chose these doses because capadenoson at 0.03, 0.1 and 0.3 mg/kg p.o. previously showed dose-dependent efficacy in a cardioprotection model in mice (personal communication from Cardiovascular Research, Bayer AG; data are not to be disclosed), and capadenoson at 0.3 mg/kg p.o. reduced overnight running distance on a running wheel in mice [18]. As shown in Fig. 3a, the SNI surgery induced a mechanical hypersensitivity of the affected hindpaw 13 days after SNI in all animals, as expected. One day thereafter, mice were p.o. treated with capadenoson, pregabalin or vehicle. However, treatment with capadenoson at all three doses did not significantly alter mechanical hypersensitivity over 24 h compared to the vehicle-treated group (Fig. 3a). By contrast, the positive control pregabalin (60 mg/kg [23, 27]), significantly ameliorated the mechanical hypersensitivity, confirming that the SNI-induced neuropathic pain behavior is responsive to standard analgesic treatment.
Neuropathic pain behavior in mice is not affected by capadenoson treatment. a In the spared nerve injury (SNI) model, neuropathic pain was induced by surgery. Fourteen days thereafter, a mechanical hypersensitivity of the affected hindpaw (determined using a Dynamic Plantar Aesthesiometer) was detected in all mice. Then animals were orally treated with vehicle (85% PEG400 / 15% glycerol, n = 13), 0.03 mg/kg capadenoson (n = 13), 0.1 mg/kg capadenoson (n = 9), 0.3 mg/kg capadenoson (n = 12), or 60 mg/kg pregabalin (n = 12) and the mechanical sensitivity was assessed over 24 h. Note that pregabalin inhibited the neuropathic pain behavior, whereas capadenoson was not effective. b In the paclitaxel model, neuropathic pain was induced by four i.p. injections of paclitaxel on day 0, 2, 4 and 6. Seven days after the last paclitaxel injection, 43% of treated animals developed a significant mechanical hypersensitivity. These animals were orally treated with vehicle (85% PEG400/15% glycerol, n = 11), 0.03 mg/kg capadenoson (n = 13), 0.1 mg/kg capadenoson (n = 13), 0.3 mg/kg capadenoson (n = 12), or 60 mg/kg pregabalin (n = 12) and the mechanical sensitivity was assessed over 24 h. Similar to the spared nerve injury model, pregabalin inhibited the paclitaxel-induced neuropathic pain behavior, whereas capadenoson was not effective. c–d In a separate cohort of mice, neuropathic pain was induced by SNI surgery. c At day 14 after SNI, the animals were orally treated with vehicle (85% PEG400/15% glycerol; n = 11), 1 mg/kg capadenoson (n = 11), or 30 mg/kg pregabalin (n = 10), and the mechanical sensitivity was assessed over 24 h. Pregabalin significantly inhibited the neuropathic pain behavior, whereas the effects of capadenoson were not significant. d At day 21 after SNI, the animals were i.v. treated by tail vein injection with vehicle (60% PEAG400 in water; n = 11), 0.3 mg/kg capadenoson (n = 11), or 0.5 mg/kg Cl-ENBA (n = 10) and the mechanical sensitivity was assessed over 5 h. Neither capadenoson nor Cl-ENBA did affect SNI-induced mechanical hypersensitivity. Data are presented as mean ± SEM. *p < 0.05, comparing drug treated and vehicle treated mice. Abbreviations used on the x-axis: BL: baseline sensitivity in naive animals; SNI: spared nerve injury-induced hypersensitivity before drug delivery; PTXL: paclitaxel-induced hypersensitivity before drug delivery
We then investigated whether capadenoson treatment may inhibit chemotherapy-induced neuropathic pain in the paclitaxel model. Four i.p. injections of 1 mg/kg paclitaxel (on days 0, 2, 4 and 6) resulted in a significant mechanical hypersensitivity (determined 6 days after the last paclitaxel injection) in 43% of all paclitaxel-injected animals. One day thereafter, mice showing a significant mechanical hypersensitivity were p.o. treated with capadenoson (0.03, 0.1 and 0.3 mg/kg), pregabalin (60 mg/kg), or vehicle. Similar to the SNI model, the delivery of capadenoson at three doses did not result in significant changes of paclitaxel-induced mechanical hypersensitivity as compared to vehicle (Fig. 3b). We observed a tendency of increased hypersensitivity after administration of 0.3 mg/kg capadenoson, which however was not significant. By contrast, treatment with pregabalin significantly inhibited the hypersensitivity (Fig. 3b). Together, these data suggest that treatment with the partial A1R agonist capadenoson at doses up to 0.3 mg/kg p.o. does not significantly affect neuropathic pain behavior in mice.
In a separate cohort of mice, we tested capadenoson at a higher dose (1 mg/kg p.o.) in the SNI model using the same experimental paradigm described above. After administration of this dose 14 days after SNI, the extent of SNI-induced mechanical hypersensitivity was slightly, but not significantly, ameliorated as compared to vehicle-treated mice (Fig. 3c). By contrast, pregabalin, which in this experiment was given at 30 mg/kg p.o. [27], significantly inhibited the mechanical hypersensitivity in comparison to vehicle (Fig. 3c).
Finally, we assessed whether intravenous (i.v.) delivery of capadenoson affects SNI-induced mechanical hypersensitivity. For these experiments we used the same cohort of mice, but injected drugs 21 days after SNI (i.e., after a wash-out period of 7 days following the 1 mg/kg capadenoson p.o. measurements). We administered capadenoson at a dose of 0.3 mg/kg i.v. that significantly decreased infarct size in a model of acute myocardial infarction in rats [19]. As a control we used the full A1R agonist Cl-ENBA at a dose of 0.5 mg/kg that has been reported to inhibit SNI-induced mechanical allodynia in mice after i.p. delivery [28]. As shown in Fig. 3d, 0.3 mg/kg i.v. capadenoson did not affect SNI-induced mechanical hypersensitivity as compared to vehicle-treated animals. Unexpectedly, 0.5 mg/kg i.v. Cl-ENBA also failed to alter the mechanical hypersensitivity (Fig. 3d; see also discussion). Moreover, all mice treated with Cl-ENBA displayed obvious sedative effects within the first 30–45 min after drug injection. Altogether, these behavioral experiments suggest that capadenoson is of limited value for the treatment of neuropathic pain.
Capadenoson fails to affect potassium currents in dissociated DRG neurons
We next assessed whether capadenoson affects electrophysiological properties of DRG neurons. Because coupling of A1R to neuronal potassium channels has been considered as a mechanism contributing to the analgesic activity of A1R agonists [29,30,31], we analyzed outward potassium currents (IK) of dissociated DRG neurons in presence of capadenoson. In particular, we assessed the transient, peak current component and the sustained, steady-state current component of IK [32, 33]. Whole-cell patch-clamp recordings were performed at a holding potential of − 70 mV by applying a 1000-ms-long prepulse of -100 mV followed by series of 500-ms-long pulses ranging from − 100 to + 120 mV in intervals of 20 mV. As shown in Fig. 4, addition of capadenoson (100 nM) to the external solution did neither affect IK peak currents (Fig. 4a) nor IK steady-state currents (Fig. 4b). An original registration at + 100 mV is depicted in Fig. 4c. The IK peak currents were also not affected by the full A1R agonist CPA (100 nM [13]; Fig. 4d). However, IK steady-state currents were significantly reduced by CPA (Fig. 4e and 4f), pointing to a coupling of A1R and potassium channels in DRG neurons. The lack of effect of capadenoson in these experiments further supports the finding that pharmacological intervention with this partial A1R agonist might not be a valuable approach for the treatment of pain.
Potassium currents in DRG neurons are not affected by capadenoson. IV relations of the total potassium currents (IK) were measured in isolated lumbar DRG neurons of mice using the whole cell patch-clamp technique. After the measurement of the control current, the partial A1R agonist capadenoson (100 nM; n = 4; a–c) or the full A1R agonist N6-cyclopentyladenosine (CPA; 100 nM; n = 5; d–f) were added into the bath solution. Ten minutes thereafter, currents were measured again. Original registrations at + 100 mV are presented in c and f and indicate the peak current component (marked by a triangle) and the steady-state current component (marked by a circle). Capadenoson failed to affect both the peak and steady-state currents. CPA did not affect the peak current but significantly reduced the steady-state current. Data are presented as mean ± SEM, *p < 0.05
Discussion
In this study, we investigated whether the partial A1R agonist capadenoson might be sufficient for treatment of neuropathic pain. Even though A1R is localized to DRG neurons and dorsal horn neurons, which are relevant for pain processing, capadenoson did not affect the pain behavior induced by peripheral nerve injury and chemotherapy, and it did not alter potassium currents in DRG neurons. Hence, capadenoson seems not to be suitable for neuropathic pain therapy.
The distribution of A1R in the nociceptive system has been investigated in earlier studies, however with conflicting results. In immunostaining experiments it was reported that A1R immunoreactivity is present in a subset of rat DRG neurons [10], and double-labeling experiments suggested that about 32%, 80% and 1% of A1R-positive rat DRG neurons co-express substance P, IB4 and NF200, respectively [11]. We here performed in situ hybridization experiments and confirmed A1R expression in a subset of mouse DRG neurons. However, our in situ hybridization combined with immunostaining revealed that A1R mRNA is expressed in 26%, 36% and 46% of neurons positive for CGRP, IB4 and NF200, respectively. Species differences in the distribution of A1R in DRG neurons of rats and mice, differences between protein and mRNA expression, or a lack of antibody specificity might account for this apparent discrepancy.
In the spinal cord, we found A1R mRNA to be enriched in dorsal horn neurons. This observation is in accordance with previous autoradiography experiments on rat spinal cord sections, in which A1R were detected predominantly in the superficial dorsal horn [34,35,36]. Immunohistochemical analyses of rat spinal cord sections were less consistent, because some studies showed a dense band of staining predominantly in lamina II of the dorsal horn [10, 12], whereas more diffuse A1R immunoreactivity throughout the spinal cord were observed in another study [13]. Hence, our in situ hybridization data add confidence that the major localization of A1R mRNA in the spinal cord are interneurons in the dorsal horn. It should be noted however that A1R has been detected in activated microglia cells after induction of neuropathic pain [37], and that delivery of an A1R agonist ameliorated the injury-induced microglia activation and neuronal sensitization [28]. Moreover, A1R are expressed in various supraspinal CNS regions including brain cortex, hippocampus, and cerebellum [9], which was however not investigated in this study.
Early preclinical studies in the 1980s with systemic and intrathecal administration of adenosine, A1R agonists and A1R antagonists suggested that targeting A1R might be suitable for treatment of neuropathic pain (for review, see [7, 38, 39]). However, the development of analgesics is hampered by the wide distribution of A1R leading to a variety of possible side effects, the high number of receptor subtypes (the four existing adenosine receptors present a sequence homology of 80–95% [9]), and the lack of truly subtype-selective agonists to be dispensed through clinically relevant routes of administration [31]. For example, systemic (intraperitoneal or intravenous) administration of the full A1R agonist CPA has been reported to inhibit neuropathic pain after nerve injury in rats [40, 41]. However, systemic treatment with CPA is accompanied by an intense depression of blood pressure as an unwanted side effect that might also affect the behavior in animal models of pain [40]. Moreover, A1R are thought to mediate the local anti-nociceptive effects of acupuncture, and injection of the A1R agonist 2-Chloro-CPA (CCPA) into the Zusanli point ST36 inhibited neuropathic pain in a model of peripheral nerve injury [42]. However, CCPA seems not to be suitable for systemic treatment as it reduced the latency to fall off the rotarod and caused catalepsy-like behavior in a dose-dependent manner [43]. Hence, the usefulness of systemic A1R agonists is limited by unwanted cardiovascular, motor and sedative side effects.
In general, improved efficacy of A1R agonists for pain treatment might be reached with allosteric modulators or partial agonists [7, 31, 44, 45]. Among the allosteric A1R modulators that have been tested for analgesia in vivo are T62 and TRR469. Oral administration of T62 reduced mechanical allodynia after peripheral nerve injury in rats. However, within 5 days of repeated daily administration, a tolerance occurred that led to decreased analgesic efficacy over time partly as a result of receptor down-regulation [46, 47]. T62 was also subjected to a clinical trial in patients with postherpetic neuralgia, which however was discontinued [9, 45]. Intraperitoneal administration of TRR469, a more potent allosteric A1R modulator as compared to T62, inhibited neuropathic pain in the model of streptozotocin-induced diabetic neuropathy and did not display locomotor or cataleptic side effects in mice [43]. Hence, there are obvious discrepancies on the effectiveness and tolerability of A1R agonists reported in different studies, probably due to the use of different compounds, routes of administration and models of neuropathic pain.
Another strategy to separate the desired from undesired pharmacological effects is to use partial A1R agonists. These compounds have been shown to activate only certain responses of A1R-mediated G-protein signaling, mostly in cells with high receptor reserve [48]. Moreover, the partial agonism is postulated to achieve conformational selection of a distinct active state, as recently shown for A2AR [49]. Hence, partial agonists might show better receptor selectivity due to increased receptor density and/or efficiency of receptor coupling to effector systems in the presence of nerve injury [7, 50, 51]. We here tested the partial A1R agonist capadenoson in two animal models of neuropathic pain. Capadenoson, which previously entered into two phase IIa clinical trials in patients with atrial fibrillation and stable angina, has been reported to have beneficial cardiovascular effects [19, 52, 53]. Unexpectedly, in our behavior experiments, four different doses of p.o. administered capadenoson (0.03, 0.1, 0.3 and 1 mg/kg) and one dose of i.v. delivered capadenoson (0.3 mg/kg) failed to significantly inhibit mechanical hypersensitivity in neuropathic pain models. In a previous study, p.o. administration of capadenoson at 0.3 and 1 mg/kg in mice led to a significant decrease of locomotion activity in a running wheel model as a surrogate marker for sedative CNS effects, and capadenoson at 1 mg/kg substantially decreased the running distance in this model by 37% [18]. We observed a trend towards inhibition of neuropathic pain behavior (not significant) at a dose of 1 mg/kg p.o. capadenoson in the SNI model. However, the profound impairment of running wheel behavior [18] indicates that this dose is associated with sedative adverse effects. Thus, we did not test higher doses of p.o. administered capadenoson in our study. Instead thereof, we assessed i.v. delivery of capadenoson at 0.3 mg/kg, but again did not observe any inhibition of neuropathic pain behavior. By contrast, capadenoson at 0.1 and 0.3 mg/kg i.v. has been reported to decrease infarct size in a model of acute myocardial infarction in rats [19]. Considering that capadenoson in the dose range of 0.3–1 mg/kg p.o. and 0.1–0.3 mg/kg i.v. provided significant pharmacological activity in other models [18, 19] we conclude that partial A1R agonism is of minor value for treatment of neuropathic pain. It should be noted however that in a recent study, capadenoson was found to have also activity at A2BR [54]. As A2BR agonists exhibit proinflammatory effects on immune cells [7], this might also affect the pain behavior after nerve injury or chemotherapy.
About the reasons for the ineffectiveness of the full A1R agonist Cl-ENBA in the SNI model we can only speculate. We intended to use 0.5 mg/kg Cl-ENBA as a positive control in our experiment with i.v. administered capadenoson, because Luongo and colleagues [28] reported that this dose significantly reduced neuropathic pain behavior after SNI. It has to be considered that Luongo et al. used a modified version of the SNI model, in which the tibial nerve is left intact [55], and not the sural nerve as in our study. Moreover, in the study by Luongo et al. Cl-ENBA was i.p. administered 7 days post injury and mechanical hypersensitivity was assessed with a dynamic plantar aesthesiometer using a ramp of 3 g/s [28], whereas we delivered Cl-ENBA i.v. 21 days post injury and used a ramp of 0.5 g/s. Although speculative, these differences in experimental settings might account for the discrepancies between the study of Luongo et al. and our findings.
The lack of efficacy of capadenoson for analgesia is also supported by our patch-clamp experiments, in which capadenoson failed to affect potassium currents in dissociated mouse DRG neurons. Various downstream mechanisms of A1R have been previously identified in different tissues including cAMP/PKA and PLC/IP3/DAG signaling, potassium channel stimulation, calcium channel inhibition, and β-arrestin mediated receptor modulation (for review, see [7]). In rat ventricular myocytes, A1R are coupled to potassium channels by G protein signaling [56], and we thus speculated that a coupling of A1R and potassium channels might also exist in DRG neurons. Indeed, in our patch-clamp experiments addition of the full A1R agonist CPA significantly decreased the steady-state potassium currents at positive voltage ranges. By contrast, the peak potassium currents were not altered, suggesting a specific inhibition of the sustained current component. In previous studies, adenosine and the full A1R agonist CCPA inhibited potassium currents by a steady-state block in AZF cells [33], and inhibition of sustained potassium currents by tetraethylammonium prolonged the duration of the repolarization phase and thereby reduced intrinsic firing in trigeminal neurons [32]. Accordingly, CPA has been shown to inhibit action potentials [57] and A- and C-fiber evoked field potentials [41] in neuronal tissues. Hence, we hypothesize that a decrease of the steady-state potassium current by CPA might lead to a reduced firing frequency in DRG neurons and inhibition of pain processing. However, in contrast to CPA, capadenoson did not affect the steady-state potassium currents in DRG neurons.
Altogether, in our study, a partial A1R agonist failed to ameliorate neuropathic pain in mice. If this holds true in other species or humans has to be shown.
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
References
van Hecke O, Austin SK, Khan RA et al (2014) Neuropathic pain in the general population: a systematic review of epidemiological studies. Pain 155:654–662. https://doi.org/10.1016/j.pain.2013.11.013
Yekkirala AS, Roberson DP, Bean BP et al (2017) Breaking barriers to novel analgesic drug development. Nat Rev Drug Discov 16:545–564. https://doi.org/10.1038/nrd.2017.87
Woolf CJ (2020) Capturing novel non-opioid pain targets. Biol Psychiat 87:74–81. https://doi.org/10.1016/j.biopsych.2019.06.017
Finnerup NB, Attal N, Haroutounian S et al (2015) Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 14:162–173
Basbaum AI, Bautista DM, Scherrer G et al (2009) Cellular and molecular mechanisms of pain. Cell 139:267–284. https://doi.org/10.1016/j.cell.2009.09.028
Colloca L, Ludman T, Bouhassira D et al (2017) Neuropathic pain Nat Rev Dis Primers 3:2220. https://doi.org/10.1038/nrdp.2017.2
Sawynok J (2016) Adenosine receptor targets for pain. Neuroscience 338:1–18. https://doi.org/10.1016/j.neuroscience.2015.10.031
Adebiyi MG, Manalo J, Kellems RE et al (2019) Differential role of adenosine signaling cascade in acute and chronic pain. Neurosci Lett 712:134483. https://doi.org/10.1016/j.neulet.2019.134483
Borea PA, Gessi S, Merighi S et al (2018) Pharmacology of adenosine receptors: the state of the art. Physiol Rev 98:1591–1625. https://doi.org/10.1152/physrev.00049.2017
Schulte G, Robertson B, Fredholm B et al (2003) Distribution of antinociceptive adenosine A1 receptors in the spinal cord dorsal horn, and relationship to primary afferents and neuronal subpopulations. Neuroscience 121:907–916. https://doi.org/10.1016/S0306-4522(03)00480-9
Lima FO, Souza GR, Verri WA, JR et al. (2010) Direct blockade of inflammatory hypernociception by peripheral A1 adenosine receptors: involvement of the NO/cGMP/PKG/KATP signaling pathway. Pain 151:506–515. https://doi.org/10.1016/j.pain.2010.08.014
Ackley MA, Governo RJM, Cass CE et al (2003) Control of glutamatergic neurotransmission in the rat spinal dorsal horn by the nucleoside transporter ENT1. J Physiol 548:507–517. https://doi.org/10.1113/jphysiol.2002.038091
Deuchars SA, Brooke RE, Deuchars J (2001) Adenosine A1 receptors rreduce release from excitatory but not inhibitory synaptic inputs onto lateral horn neurons. J Neurosci 21:6308–6320. https://doi.org/10.1523/JNEUROSCI.21-16-06308.2001
Wu W-P, Hao J-X, Halldner L et al (2005) Increased nociceptive response in mice lacking the adenosine A1 receptor. Pain 113:395–404. https://doi.org/10.1016/j.pain.2004.11.020
Zylka MJ, Sowa NA, Taylor-Blake B et al (2008) Prostatic acid phosphatase is an ectonucleotidase and suppresses pain by generating adenosine. Neuron 60:111–122. https://doi.org/10.1016/j.neuron.2008.08.024
Sowa NA, Voss MK, Zylka MJ (2010) Recombinant ecto-5′-Nucleotidase (CD73) has long lasting antinociceptive effects that are dependent on adenosine A1 receptor activation. Mol. Pain 6:1744–8069–6–20. https://doi.org/10.1186/1744-8069-6-20
Korboukh I, Hull-Ryde EA, Rittiner JE et al (2012) Orally active adenosine A1 receptor agonists with antinociceptive effects in mice. J Med Chem 55:6467–6477. https://doi.org/10.1021/jm3004834
Meibom D, Albrecht-Küpper B, Diedrichs N et al (2017) Neladenoson bialanate hydrochloride: a prodrug of a partial adenosine A1 receptor agonist for the chronic treatment of heart diseases. ChemMedChem 12:728–737. https://doi.org/10.1002/cmdc.201700151
Albrecht-Kupper BE, Leineweber K, Nell PG (2012) Partial adenosine A1 receptor agonists for cardiovascular therapies. Purinergic Signal 8:91–99. https://doi.org/10.1007/s11302-011-9274-3
Decosterd I, Woolf CJ (2000) Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain 87:149–158. https://doi.org/10.1016/S0304-3959(00)00276-1
Smith SB, Crager SE, Mogil JS (2004) Paclitaxel-induced neuropathic hypersensitivity in mice: Responses in 10 inbred mouse strains. Life Sci 74:2593–2604. https://doi.org/10.1016/j.lfs.2004.01.002
Alessandri-Haber N, Dina OA, Joseph EK et al (2008) Interaction of transient receptor potential vanilloid 4, integrin, and Src tyrosine kinase in mechanical hyperalgesia. J Neurosci 28:1046–1057. https://doi.org/10.1523/JNEUROSCI.4497-07.2008
Lu R, Bausch AE, Kallenborn-Gerhardt W et al (2015) Slack channels expressed in sensory neurons control neuropathic pain in mice. J Neurosci 35:1125–1135. https://doi.org/10.1523/JNEUROSCI.2423-14.2015
Schmidtko A, Gao W, Konig P et al (2008) cGMP produced by NO-sensitive guanylyl cyclase essentially contributes to inflammatory and neuropathic pain by using targets different from cGMP-dependent protein kinase I. J Neurosci 28:8568–8576. https://doi.org/10.1523/JNEUROSCI.2128-08.2008
Heine S, Michalakis S, Kallenborn-Gerhardt W et al (2011) CNGA3: a target of spinal nitric oxide/cGMP signaling and modulator of inflammatory pain hypersensitivity. J Neurosci 31:11184–11192. https://doi.org/10.1523/JNEUROSCI.6159-10.2011
Petersen J, Mergia E, Kennel L et al (2019) Distinct functions of soluble guanylyl cyclase isoforms NO-GC1 and NO-GC2 in inflammatory and neuropathic pain processing. Pain 160:607–618. https://doi.org/10.1097/j.pain.0000000000001440
Leksiri S, Hasriadi, Dasuni Wasana PW et al. (2020) Co-administration of pregabalin and curcumin synergistically decreases pain-like behaviors in acute nociceptive pain murine models. Molecules 25. https://doi.org/10.3390/molecules25184172
Luongo L, Petrelli R, Gatta L et al (2012) 5’-Chloro-5’-deoxy-(±)-ENBA, a potent and selective adenosine A1 receptor agonist, alleviates neuropathic pain in mice through functional glial and microglial changes without affecting motor or cardiovascular functions. Molecules 17:13712–13726. https://doi.org/10.3390/molecules171213712
Trussell LO, Jackson MB (1985) Adenosine-activated potassium conductance in cultured striatal neurons. PNAS 82:4857–4861. https://doi.org/10.1073/pnas.82.14.4857
Varani K, Vincenzi F, Merighi S et al. (2017) Biochemical and pharmacological role of A1 adenosine receptors and their modulation as novel therapeutic strategy. Protein Reviews 1051. https://doi.org/10.1007/5584_2017_61
Magni G, Ceruti S (2019) The role of adenosine and P2Y receptors expressed by multiple cell types in pain transmission. Brain Res Bull 151:132–143. https://doi.org/10.1016/j.brainresbull.2019.02.011
Yoshida S, Takahashi M, Kadoi J et al (2007) The functional difference between transient and sustained K+ currents on the action potentials in tetrodotoxin-resistant adult rat trigeminal ganglion neurons. Brain Res 1152:64–74. https://doi.org/10.1016/j.brainres.2007.03.039
Xu L, Enyeart JJ (1999) Adenosine inhibits a non-inactivating K+ current in bovine adrenal cortical cells by activation of multiple P1 receptors. J Physiology 521(Pt 1):81–97. https://doi.org/10.1111/j.1469-7793.1999.00081.x
Geiger JD, LaBella FS, Nagy JI (1984) Characterization and localization of adenosine receptors in rat spinal cord. J Neurosci 4:2303–2310. https://doi.org/10.1523/JNEUROSCI.04-09-02303.1984
Choca JI, Green RD, Proudfit HK (1988) Adenosine A1 and A2 receptors of the substantia gelatinosa are located predominantly on intrinsic neurons: an autoradiography study. J Pharmacol Exp Ther 247:757
Bantel CM, Childers SRP, Eisenach JCM (2002) Role of adenosine receptors in spinal G-protein activation after peripheral nerve injury. Anesthesiology 96:1443–1449
Luongo L, Guida F, Imperatore R et al (2014) The A1 adenosine receptor as a new player in microglia physiology. Glia 62:122–132. https://doi.org/10.1002/glia.22592
Sawynok J (1998) Adenosine receptor activation and nociception. Eur J Pharmacol 347:1–11. https://doi.org/10.1016/S0014-2999(97)01605-1
Dickenson AH, Suzuki R, Reeve AJ (2000) Adenosine as a potential analgesic target in inflammatory and neuropathic pains. CNS Drugs 13:77–85. https://doi.org/10.2165/00023210-200013020-00001
Curros-Criado MM, Herrero JF (2005) The antinociceptive effects of the systemic adenosine A1 receptor agonist CPA in the absence and in the presence of spinal cord sensitization. Pharmacol Biochem Behav 82:721–726. https://doi.org/10.1016/j.pbb.2005.11.014
Gong Q-J, Li Y-Y, Xin W-J et al (2010) Differential effects of adenosine A1 receptor on pain-related behavior in normal and nerve-injured rats. Brain Res 1361:23–30. https://doi.org/10.1016/j.brainres.2010.09.034
Goldman N, Chen M, Fujita T et al (2010) Adenosine A1 receptors mediate local anti-nociceptive effects of acupuncture. Nat Neurosci 13:883–888. https://doi.org/10.1038/nn.2562
Vincenzi F, Targa M, Romagnoli R et al (2014) TRR469, a potent A1 adenosine receptor allosteric modulator, exhibits anti-nociceptive properties in acute and neuropathic pain models in mice. Neuropharmacology 81:6–14. https://doi.org/10.1016/j.neuropharm.2014.01.028
Petrelli R, Torquati I, Kachler S et al (2015) 5′-C-Ethyl-tetrazolyl-N6-substituted adenosine and 2-Chloro-adenosine derivatives as highly potent dual acting A1 adenosine receptor agonists and A3 adenosine receptor antagonists. J Med Chem 58:2560–2566. https://doi.org/10.1021/acs.jmedchem.5b00074
Deb PK (2019) Therapeutic potentials of adenosine receptors: the state of the art. Curr Pharm Des 25:2789–2791. https://doi.org/10.2174/138161282526191007143942
Li X, Conklin D, Ma W et al (2002) Spinal noradrenergic activation mediates allodynia reduction from an allosteric adenosine modulator in a rat model of neuropathic pain. Pain 97:117–125. https://doi.org/10.1016/S0304-3959(02)00011-8
Li XP, Bantel CM, Conklin DB et al (2004) Repeated dosing with oral allosteric modulator of adenosine A1 receptor produces tolerance in rats with neuropathic pain. Anesthesiology 100:956–961
Srinivas M, Shryock JC, Dennis DM et al (1997) Differential A1 adenosine receptor reserve for two actions of adenosine on guinea pig atrial myocytes. Mol Pharmacol 52:683–691. https://doi.org/10.1124/mol.52.4.683
Ye L, van Eps N, Zimmer M et al (2016) Activation of the A2A adenosine G-protein-coupled receptor by conformational selection. Nature 533:265–268. https://doi.org/10.1038/nature17668
Schaddelee MP, Collins SD, DeJongh J et al (2005) Pharmacokinetic/pharmacodynamic modelling of the anti-hyperalgesic and anti-nociceptive effect of adenosine A1 receptor partial agonists in neuropathic pain. Eur J Pharmacol 514:131–140. https://doi.org/10.1016/j.ejphar.2005.03.026
Magni G, Riccio D, Ceruti S (2018) Tackling chronic pain and inflammation through the purinergic system. Curr Med Chem 25:3830–3865. https://doi.org/10.2174/0929867324666170710110630
Tendera M, Gaszewska-Zurek E, Parma Z et al (2012) The new oral adenosine A1 receptor agonist capadenoson in male patients with stable angina. Clin Res Cardiol 101:585–591. https://doi.org/10.1007/s00392-012-0430-8
Sabbah HN, Gupta RC, Kohli S et al (2013) Chronic therapy with a partial adenosine A1 receptor agonist improves left ventricular function and remodeling in dogs with advanced heart failure. Circ Heart Fail 6:563–571. https://doi.org/10.1161/CIRCHEARTFAILURE.112.000208
Baltos J-A, Vecchio EA, Harris MA et al (2017) Capadenoson, a clinically trialed partial adenosine A1 receptor agonist, can stimulate adenosine A2B receptor biased agonism. Biochem Pharmacol 135:79–89. https://doi.org/10.1016/j.bcp.2017.03.014
Shields SD, Eckert WA, Basbaum AI (2003) Spared nerve injury model of neuropathic pain in the mouse: a behavioral and anatomic analysis. J Pain 4:465–470. https://doi.org/10.1067/S1526-5900(03)00781-8
Kirsch GE, Codina J, Birnbaumer L et al (1990) Coupling of ATP-sensitive K+ channels to A1 receptors by G proteins in rat ventricular myocytes. Am J Physiol 259:H820–H826. https://doi.org/10.1152/ajpheart.1990.259.3.H820
Hargus NJ, Bertram EH, Patel MK (2009) Adenosine A1 receptors presynaptically modulate excitatory synaptic input onto subiculum neurons. Brain Res 1280:60–68. https://doi.org/10.1016/j.brainres.2009.05.027
Acknowledgements
We are grateful to Cyntia Schäfer for excellent technical assistance. This study was supported by the Grants4IndicationsTM initiative of Bayer AG, Leverkusen, Germany, and by European Regional Development Fund/LeitmarktAgentur.NRW (EFRE-0800971/LS-1-2-023d). The funding sources had no role in study design; the collection, analysis, and interpretation of data; or the writing of the manuscript and the decision to publish.
Funding
Open Access funding enabled and organized by Projekt DEAL. This study was supported by the Grants4Indications™ initiative of Bayer AG, Leverkusen, Germany, and by European Regional Development Fund/LeitmarktAgentur.NRW (EFRE-0800971/LS-1–2-023d). The funding sources had no role in study design; the collection, analysis, and interpretation of data; or the writing of the manuscript and the decision to publish.
Author information
Authors and Affiliations
Contributions
Achim Schmidtko designed and supervised the experiments. Katharina Metzner, Tilman Gross, Annika Balzulat, Gesine Wack, and Ruirui Lu conducted the experiments. Katharina Metzner and Achim Schmidtko analyzed the data and wrote the manuscript. All authors discussed the results and commented on the manuscript.
Corresponding author
Ethics declarations
Ethics approval
All experiments were ethically reviewed and approved by our local Ethics Committee for Animal Research (Regierungspräsidium Darmstadt, Germany).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Conflicts of interest
Katharina Metzner declares no conflict of interest.
Tilman Groß declares no conflict of interest.
Annika Balzulat declares no conflict of interest.
Gesine Wack declares no conflict of interest.
Ruirui Lu declares no conflict of interest.
Achim Schmidtko declares no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Metzner, K., Gross, T., Balzulat, A. et al. Lack of efficacy of a partial adenosine A1 receptor agonist in neuropathic pain models in mice. Purinergic Signalling 17, 503–514 (2021). https://doi.org/10.1007/s11302-021-09806-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11302-021-09806-6