Abstract
Purpose
This study was designed to investigate the clinicopathological features of idiopathic membranous nephropathy (IMN) with hyperuricemia (HUA), together with associated factors within 10 years in a single centre in Shandong Province.
Methods
In this cross-sectional study, we analysed the clinical and pathological data of 694 IMN patients in our hospital from January 2010 to December 2019. Based on serum uric acid (UA) level, the patients were divided into hyperuricemia (HUA) group (n = 213) and normal serum uric acid (NUA) group (n = 481). Multi-variate logistic regression analysis was conducted on to screen the associated factors of HUA.
Results
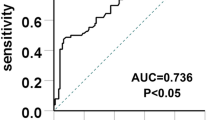
213 (30.69%) IMN patient were complicated with HUA. Compared with the patients with NUA, significant increase was noticed in the proportion of patients showing edema, concurrent hypertensive disease or diabetes mellitus (DM), as well as the proportion of positive glomerular capillary loop IgM and positive C1q in the HUA group (P < 0.05). In addition, significant increase was noticed in the 24 h urine protein, serum creatinine, triglycerides, complement C3 and complement C4 in HUA group compared with those of NUA group (all P < 0.05). With gender as a control factor, multi-variate logistic regression analysis showed positive glomerular capillary loops C1q, serum albumin, serum phosphorus were associated with IMN combined with HUA in male, while triglycerides and serum creatinine were associated with IMN combined with HUA in female counterparts.
Conclusion
About 30.69% of IMN patients had HUA, with a male predominance than female. In male patients with IMN, higher serum albumin level and serum phosphorus level were associated with higher incidence of HUA, while in female IMN patients, higher serum triglyceridemia and serum creatinine level were associated with higher incidence of HUA. Therefore, it can be targeted to prevent the occurrence of HUA in IMN.


Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Ramachandran R, Kaundal U, Girimaji N, Rakha A, Rathi M, Gupta KL, Kohli HS, Jha V (2020) Regulatory B cells are reduced and correlate with disease activity in primary membranous nephropathy. Kidney Intern Rep 5(6):872–878. https://doi.org/10.1016/j.ekir.2020.03.023
Safar-Boueri L, Piya A, Beck LH Jr, Ayalon R (2021) Membranous nephropathy: diagnosis, treatment, and monitoring in the post-PLA2R era. Pediatr Nephrol 36(1):19–30. https://doi.org/10.1007/s00467-019-04425-1
Kidney Disease: Improving Global Outcomes Glomerular Diseases Work G (2021) KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney Int 100(4S):S1–S276. https://doi.org/10.1016/j.kint.2021.05.021
Couser WG (2017) Primary membranous nephropathy. Clin J Am Soc Nephrol 12(6):983–997. https://doi.org/10.2215/CJN.11761116
Kanda E, Muneyuki T, Kanno Y, Suwa K, Nakajima K (2015) Uric acid level has a U-shaped association with loss of kidney function in healthy people: a prospective cohort study. PLoS ONE 10(2):e0118031. https://doi.org/10.1371/journal.pone.0118031
Liu R, Han C, Wu D, Xia X, Gu J, Guan H, Shan Z, Teng W (2015) Prevalence of hyperuricemia and gout in mainland china from 2000 to 2014: a systematic review and meta-analysis. Biomed Res Int 2015:762820. https://doi.org/10.1155/2015/762820
Su HY, Yang C, Liang D, Liu HF (2020) Research advances in the mechanisms of hyperuricemia-induced renal injury. Biomed Res Int 2020:5817348. https://doi.org/10.1155/2020/5817348
Fan S, Zhang P, Wang AY, Wang X, Wang L, Li G, Hong D (2019) Hyperuricemia and its related histopathological features on renal biopsy. BMC Nephrol 20(1):95. https://doi.org/10.1186/s12882-019-1275-4
Johnson RJ, Nakagawa T, Jalal D, Sánchez-Lozada LG, Duk-Hee K (2013) Uric acid and chronic kidney disease: which is chasing which? Nephrol Dialy Trans. 28(9):2221–2228
Liu B, Zhao L, Yang Q, Zha D, Si X (2021) Hyperuricemia and hypertriglyceridemia indicate tubular atrophy/interstitial fibrosis in patients with IgA nephropathy and membranous nephropathy. Int Urol Nephrol. https://doi.org/10.1007/s11255-021-02844-4
Zhang J, Pan M, Zhang J, You X, Li D, Lin F, Lu G (2019) Serum uric acid is an independent predictor of renal outcomes in patients with idiopathic membranous nephropathy. Int Urol Nephrol 51(10):1797–1804. https://doi.org/10.1007/s11255-019-02254-7
Hisatome I, Li P, Miake J, Taufiq F, Mahati E, Maharani N, Utami SB, Kuwabara M, Bahrudin U, Ninomiya H (2021) Uric acid as a risk factor for chronic kidney disease and cardiovascular disease—japanese guideline on the management of asymptomatic hyperuricemia. Circ J 85(2):130–138. https://doi.org/10.1253/circj.CJ-20-0406
Fogo AB (2003) Approach to renal biopsy. Am J Kidney Dis 42(4):826–836
Fu K, Zhang P, Han Y, Wang R, Cai J (2022) Anti-phospholipase A2 receptor antibody expression at different stages of idiopathic membranous nephropathy. Int J Nephrol 2022:5962195. https://doi.org/10.1155/2022/5962195
Li Y, Shen Z, Zhu B, Zhang H, Zhang X, Ding X (2021) Demographic, regional and temporal trends of hyperuricemia epidemics in mainland China from 2000 to 2019: a systematic review and meta-analysis. Glob Health Action 14(1):1874652. https://doi.org/10.1080/16549716.2021.1874652
Deng W, Tan X, Zhou Q, Ai Z, Liu W, Chen W, Yu X, Yang Q (2018) Gender-related differences in clinicopathological characteristics and renal outcomes of Chinese patients with IgA nephropathy. BMC Nephrol 19(1):31. https://doi.org/10.1186/s12882-018-0829-1
Bellomo G, Venanzi S, Verdura C, Saronio P, Esposito A, Timio M (2010) Association of uric acid with change in kidney function in healthy normotensive individuals. Am J Kidney Dis 56(2):264–272. https://doi.org/10.1053/j.ajkd.2010.01.019
Uchida S, Chang WX, Ota T, Tamura Y, Shiraishi T, Kumagai T, Shibata S, Fujigaki Y, Hosoyamada M, Kaneko K, Shen ZY, Fujimori S (2015) Targeting uric acid and the inhibition of progression to end-stage renal disease–a propensity score analysis. PLoS ONE 10(12):e0145506. https://doi.org/10.1371/journal.pone.0145506
Mortada I (2017) Hyperuricemia, type 2 diabetes mellitus, and hypertension: an emerging association. Curr Hypertens Rep 19(9):69. https://doi.org/10.1007/s11906-017-0770-x
Jin M, Yang F, Yang I, Yin Y, Luo JJ, Wang H, Yang XF (2012) Uric acid, hyperuricemia and vascular diseases. Front Biosci (Landmark Ed) 17:656–669. https://doi.org/10.2741/3950
Li Q, Zhang Y, Cao J, Zhang J, Nie J, Liang M, Li J, Zhang Y, Wang B, Huo Y, Wang X, Hou FF, Xu X, Qin X (2020) Degree of blood pressure control and the risk of new-onset hyperuricemia in treated hypertensive patients. Ann Transl Med 8(21):1434. https://doi.org/10.21037/atm-20-3017
Lv Q, Meng XF, He FF, Chen S, Su H, Xiong J, Gao P, Tian XJ, Liu JS, Zhu ZH, Huang K, Zhang C (2013) High serum uric acid and increased risk of type 2 diabetes: a systemic review and meta-analysis of prospective cohort studies. PLoS ONE 8(2):e56864. https://doi.org/10.1371/journal.pone.0056864
Chaudhary K, Malhotra K, Sowers J, Aroor A (2013) Uric acid—key ingredient in the recipe for cardiorenal metabolic syndrome. Cardiorenal Med 3(3):208–220. https://doi.org/10.1159/000355405
Cai Q, Hendricks AR (2020) Membranous nephropathy: a ten-year journey of discoveries. Semin Diagn Pathol 37(3):116–120. https://doi.org/10.1053/j.semdp.2020.01.001
Nirula A, Glaser SM, Kalled SL, Taylor FR (2011) What is IgG4? A review of the biology of a unique immunoglobulin subtype. Curr Opin Rheumatol 23(1):119–124. https://doi.org/10.1097/BOR.0b013e3283412fd4
Ma H, Sandor DG, Beck LH Jr (2013) The role of complement in membranous nephropathy. Semin Nephrol 33(6):531–542. https://doi.org/10.1016/j.semnephrol.2013.08.004
Zhang MF, Cui Z, Zhang YM, Qu Z, Wang X, Wang F, Meng LQ, Cheng XY, Liu G, Zhao MH (2018) Clinical and prognostic significance of glomerular C1q deposits in primary MN. Clin Chim Acta 485:152–157. https://doi.org/10.1016/j.cca.2018.06.050
Jin SM, Hong YJ, Jee JH, Bae JC, Hur KY, Lee MK, Kim JH (2016) Change in serum albumin concentration is inversely and independently associated with risk of incident metabolic syndrome. Metabolism 65(11):1629–1635. https://doi.org/10.1016/j.metabol.2016.08.006
Hou YL, Yang XL, Wang CX, Zhi LX, Yang MJ, You CG (2019) Hypertriglyceridemia and hyperuricemia: a retrospective study of urban residents. Lipids Health Dis 18(1):81. https://doi.org/10.1186/s12944-019-1031-6
Lippi G, Montagnana M, Luca Salvagno G, Targher G, Cesare Guidi G (2010) Epidemiological association between uric acid concentration in plasma, lipoprotein(a), and the traditional lipid profile. Clin Cardiol 33(2):E76-80. https://doi.org/10.1002/clc.20511
Chen JH, Pan WH, Hsu CC, Yeh WT, Chuang SY, Chen PY, Chen HC, Chang CT, Huang WL (2013) Impact of obesity and hypertriglyceridemia on gout development with or without hyperuricemia: a prospective study. Arthritis Care Res (Hoboken) 65(1):133–140. https://doi.org/10.1002/acr.21824
Mazza A, Lenti S, Schiavon L, Monte AD, Townsend DM, Ramazzina E, Rubello D, Casiglia E (2017) Asymptomatic hyperuricemia is a strong risk factor for resistant hypertension in elderly subjects from general population. Biomed Pharmacother 86:590–594. https://doi.org/10.1016/j.biopha.2016.11.104
Nakanishi N, Tatara K, Nakamura K, Suzuki K (1999) Risk factors for the incidence of hyperuricaemia: a 6 year longitudinal study of middle-aged Japanese men. Int J Epidemiol 28(5):888–893. https://doi.org/10.1093/ije/28.5.888
Balasubramanian T (2003) Uric acid or 1-methyl uric acid in the urinary bladder increases serum glucose, insulin, true triglyceride, and total cholesterol levels in Wistar rats. ScientificWorldJournal 3:930–936. https://doi.org/10.1100/tsw.2003.90
Da J, Xie X, Wolf M, Disthabanchong S, Wang J, Zha Y, Lv J, Zhang L, Wang H (2015) Serum phosphorus and progression of ckd and mortality: a meta-analysis of cohort studies. Am J Kidney Dis 66(2):258–265. https://doi.org/10.1053/j.ajkd.2015.01.009
Funding
This work was supported by Shandong Medicine and Health Science Technology Development Project [NO. 2017WS689], College Students’ Innovative Entrepreneurial Training Plan Program [NO. X202110440283].
Author information
Authors and Affiliations
Contributions
LD, ZH and LQY: contributed to manuscript drafting. WXH and CZM: collected the clinical data. YM: analyzed the collected data. DH and WYN: led the renal biopsy. LYQ and ZXM: helped to write the manuscript. ZXM: supervised the entire project. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no competing interests to declare that are relevant to the content of this article.
Ethics approval
The study protocol was consistent with the ethical principles of the Helsinki and was approved by the Ethics Committee of the Affiliated Hospital of Binzhou Medical University (Approval No.: 2021-LW-010) and individual consent for this retrospective analysis was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liang, D., Zhang, H., Lin, Q. et al. Clinicopathological characteristics and associated factors of idiopathic membranous nephropathy with hyperuricemia: a single-centered cross-sectional study. Int Urol Nephrol 55, 2275–2283 (2023). https://doi.org/10.1007/s11255-023-03523-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-023-03523-2