Abstract
Purpose
Acute kidney injury (AKI) is a common organ dysfunction in ICU and up to now there is no good way to predict the AKI progression and patient prognosis. Blood electrolyte tests are common in ICU, but there are few studies on early blood electrolytes and the AKI progression and patient prognosis. Therefore, we concentrated on the serum sodium and potassium levels before AKI diagnosis and evaluated the relationship between serum sodium and potassium levels and the severity and prognosis of AKI.
Methods
This study included data of all patients from the MIMIC-III. We used the urine output criteria in the KDIGO as diagnostic criteria for oliguric AKI. Patients admitted to the ICU several times only included their initial ICU admission results. Patients younger than 18 years old, diagnosed with AKI stage 3, ICU stays less than 24 h or without corresponding laboratory results or data were excluded. The included patients were divided into four groups based on the interquartile range of serum sodium and potassium. We evaluated the serum sodium and potassium levels before AKI diagnosis and AKI severity and prognosis through retrospective analysis.
Results
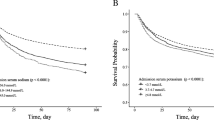
Patients with serum potassium > 4.6 mmol/L were more likely to progress to AKI stage 3 or death than patients with serum potassium ≤ 4.6 mmol/L (overall p < 0.0001). Patients with sodium < 137 mmol/L or > 141 mmol/L had a higher risk of progressing to AKI stage 3 (overall p = 0.00023) and risk of death (overall p < 0.0001) than other patients. In the Cox regression model, after adjusting for age, sex, and BMI, serum sodium or potassium were associated with AKI progression and prognosis (p < 0.01). After continuing to adjust for comorbidities, serum potassium was still associated with AKI progression and prognosis (p < 0.01), but serum sodium was only associated with prognosis (p = 0.027). After adjusting for other indicators, there was no statistically significant correlation between serum sodium or potassium and AKI progression and prognosis. After adjusting for serum sodium or potassium, the corresponding results were not significantly different from those before adjustment.
Conclusion
This study found that abnormal serum sodium or potassium levels before AKI diagnosis were more likely to lead to AKI progression and poor prognosis, of which lower serum sodium and higher serum potassium were more likely to progress to AKI stage 3 or death.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Wonnacott A, Meran S, Amphlett B, Talabani B, Phillips A (2014) Epidemiology and outcomes in community-acquired versus hospital-acquired AKI. Clin J Am Soc Nephrol CJASN 9(6):1007–1014. https://doi.org/10.2215/CJN.07920713
Levey AS, James MT (2018) Acute kidney injury. Ann Intern Med 168(11):837. https://doi.org/10.7326/L18-0017
Kellum JA, Lameire N, KDIGO AKI Guideline Work Group (2013) Diagnosis, evaluation, and management of acute kidney injury: a KDIGO summary (part 1). Crit Care Lond Engl 17(1):204. https://doi.org/10.1186/cc11454
Sancho-Martínez SM, Sánchez-Juanes F, Blanco-Gozalo V et al (2020) Urinary TCP1-eta: a cortical damage marker for the pathophysiological diagnosis and prognosis of acute kidney injury. Toxicol Sci Off J Soc Toxicol 174(1):3–15. https://doi.org/10.1093/toxsci/kfz242
Tomašev N, Glorot X, Rae JW et al (2019) A clinically applicable approach to continuous prediction of future acute kidney injury. Nature 572(7767):116–119. https://doi.org/10.1038/s41586-019-1390-1
Lima C, Macedo E (2018) Urinary biochemistry in the diagnosis of acute kidney injury. Dis Markers 2018:4907024. https://doi.org/10.1155/2018/4907024
Johnson AEW, Pollard TJ, Shen L et al (2016) MIMIC-III, a freely accessible critical care database. Sci Data 3:160035. https://doi.org/10.1038/sdata.2016.35
Johnson AE, Stone DJ, Celi LA, Pollard TJ (2018) The MIMIC code repository: enabling reproducibility in critical care research. J Am Med Inf Assoc JAMIA 25(1):32–39. https://doi.org/10.1093/jamia/ocx084
Satirapoj B, Kongthaworn S, Choovichian P, Supasyndh O (2016) Electrolyte disturbances and risk factors of acute kidney injury patients receiving dialysis in exertional heat stroke. BMC Nephrol 17(1):55. https://doi.org/10.1186/s12882-016-0268-9
Belcher JM, Garcia-Tsao G, Sanyal AJ et al (2014) Urinary biomarkers and progression of AKI in patients with cirrhosis. Clin J Am Soc Nephrol CJASN 9(11):1857–1867. https://doi.org/10.2215/CJN.09430913
Albuquerque PLMM, da Silva Junior GB, Meneses GC et al (2019) Acute kidney injury induced by Bothrops venom: insights into the pathogenic mechanisms. Toxins 11(3):148. https://doi.org/10.3390/toxins11030148
Gao X-P, Zheng C-F, Liao M-Q et al (2019) Admission serum sodium and potassium levels predict survival among critically ill patients with acute kidney injury: a cohort study. BMC Nephrol 20(1):311. https://doi.org/10.1186/s12882-019-1505-9
du Cheyron D, Lesage A, Daubin C, Ramakers M, Charbonneau P (2003) Hyperreninemic hypoaldosteronism: a possible etiological factor of septic shock-induced acute renal failure. Intensive Care Med 29(10):1703–1709. https://doi.org/10.1007/s00134-003-1986-6
Woitok BK, Funk G-C, Walter P, Schwarz C, Ravioli S, Lindner G (2020) Dysnatremias in emergency patients with acute kidney injury: a cross-sectional analysis. Am J Emerg Med. https://doi.org/10.1016/j.ajem.2020.01.009 ((Published online January 7))
Shum H-P, Kong HH-Y, Chan K-C, Yan W-W, Chan TM (2016) Septic acute kidney injury in critically ill patients—a single-center study on its incidence, clinical characteristics, and outcome predictors. Ren Fail 38(5):706–716. https://doi.org/10.3109/0886022X.2016.1157749
Bagshaw SM, George C, Bellomo R, ANZICS Database Management Committee (2008) Early acute kidney injury and sepsis: a multicentre evaluation. Crit Care Lond Engl 12(2):R47. https://doi.org/10.1186/cc6863
Burns AR, Ho KM (2018) Urinary potassium excretion and its association with acute kidney injury in the intensive care unit. J Crit Care 46:58–62. https://doi.org/10.1016/j.jcrc.2018.04.009
Korgaonkar S, Tilea A, Gillespie BW et al (2010) Serum potassium and outcomes in CKD: insights from the RRI-CKD cohort study. Clin J Am Soc Nephrol CJASN 5(5):762–769. https://doi.org/10.2215/CJN.05850809
Moore BJ, White S, Washington R, Coenen N, Elixhauser A (2017) Identifying increased risk of readmission and in-hospital mortality using hospital administrative data: the AHRQ Elixhauser Comorbidity Index. Med Care 55(7):698–705. https://doi.org/10.1097/MLR.0000000000000735
Bernardi MH, Schmidlin D, Ristl R et al (2016) Serum creatinine back-estimation in cardiac surgery patients: misclassification of AKI Using existing formulae and a data-driven model. Clin J Am Soc Nephrol CJASN 11(3):395–404. https://doi.org/10.2215/CJN.03560315
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix
See Tables 4, 5, 6, 7, 8, 9 and 10.
Rights and permissions
About this article
Cite this article
Chen, DN., Du, J., Xie, Y. et al. Relationship between early serum sodium and potassium levels and AKI severity and prognosis in oliguric AKI patients. Int Urol Nephrol 53, 1171–1187 (2021). https://doi.org/10.1007/s11255-020-02724-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-020-02724-3