Abstract
Objective
To evaluate patient preferences for refractory overactive bladder (OAB) treatments: sacral neuromodulation (SNM), onabotulinum toxin A (Botox®), and percutaneous tibial nerve stimulation (PTNS).
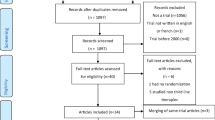
Materials and methods
A cross-sectional Web survey was conducted with UK idiopathic OAB patients, recruited by a market research company. Preference was explored using direct questioning, comparing SNM, Botox, and PTNS, and via best–worst scaling (BWS). In BWS, patients prioritized subsets of 13 treatment characteristics (attributes) across 13 choice tasks, identifying the attribute they considered best and worst in each task. The attributes were those that were identified by patients in previous qualitative interviews as influential in treatment selection. BWS scores for each attribute, ranging from 1.0 (most favourable) to −1.0 (most unfavourable), were calculated based on the rates they were identified as best and as worst. To identify attributes that may influence treatment choice, BWS scores were compared among patients based on their most preferred treatment using analyses of variance; pairwise differences were assessed using Tukey’s multiple comparisons test.
Results
The study population (N = 139) was 77 % female, had a mean age of 49 years, and were diagnosed a mean of 6.1 years ago. All 13 attribute BWS scores were viewed positively (score > 0.0) or negatively (score < 0.0). Among the 127 (91 %) of patients who had experience with OAB medication only, most (≥80 %) were willing to try each of the three treatments; 57, 34, and 9 % most preferred PTNS, SNM, and Botox, respectively. Preferences for the attributes differed based on which treatment that patients preferred. Specifically, patients preferring SNM (PS) favoured ‘implanted device in upper buttock’ more than those preferring PTNS (PP) or Botox (PB). Compared to PB, PS also favoured ‘sends signals between bladder and brain to help restore bladder function’ and ‘test phase’. PB favoured ‘Botox (botulinum toxin) treatment’ and ‘treatment procedure delivered through the urethra’ more than PS and PP. PP favoured the following more than PS and PB: ‘needle inserted into ankle’, ‘minimal side effects’ and ‘treatment requires repeated visits over time’.
Conclusion
This study identified specific characteristics of specialized therapies for refractory OAB that may significantly influence patient preferences, which may be used to help inform treatment decision-making.



Similar content being viewed by others
References
Haylen B, de Ridder D, Freeman RM et al (2010) An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J 21:5–26
Link CL, Steers WD, Kusek JW, McKinlay JB (2011) The Association of Adiposity and Overactive Bladder appears to differ by gender: results from the Boston Area Community Health (BACH) Survey. J Urol 185(3):955–963
Irwin DE, Kopp ZS, Agatep B, Milsom I, Abrams P (2011) Worldwide prevalence estimates of lower urinary tract symptoms, overactive bladder, urinary incontinence and bladder outlet obstruction. BJU Int 108(7):1132–1138
Irwin DE, Milsom I, Hunskaar S et al (2006) Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol 50(6):1306–1314
Lee UJ, Scott VC, Rashid R et al (2013) Defining and managing overactive bladder: disagreement among the experts. Urology 81(2):257–262
Elterman DS, Chughtai B, Kaplan SA, Barkin J (2013) Tolterodine for the treatment of urge urinary incontinence. Expert Opin Pharmacother 14(14):1987–1991
Brubaker L, Gousse A, Sand P et al (2012) Treatment satisfaction and goal attainment with onabotulinumtoxin A in patients with incontinence due to idiopathic OAB. Int Urogynecol J 23(8):1017–1025
Schulte- Baukloh H, Weiss C, Stolze T, Sturzebecher B, Knispel HH (2005) Botulinum-A toxin for treatment of overactive bladder without detrusor overactivity: urodynamic outcome and patient satisfaction. Urology 66(1):82–87
Levy M et al (2014) Patient defined goals of care in treatment of medication refractory overactive bladder. Neurourol Urodyn 33(2):180
Leong RK, Marcelissen TA, Nieman FH, De Bie RA, Van Kerrebroeck PE, De Wachter SG (2011) Satisfaction and patient experience with sacral neuromodulation: results from a single center sample survey. J Urol 185(2):588–592
Bauer RM et al (2011) Patient-reported side effects of intradetrusor botulinum toxin type A for idiopathic overactive bladder syndrome. Urol Int 86(1):68–72
El-Azab AS, Moeen AM (2013) The satisfaction of patients with refractory idiopathic overactive bladder with onabotulinumtoxinA and augmentation cystoplasty. Arab J Urol 11(4):344–349
Imam H (2011) Patient satisfaction after intravesical botulinum toxin type a injection for refractory detrusor overactivity. Neurourol Urodyn 30(2):266
Urinary incontinence in women: the management of urinary incontinence in women [Internet], 2nd ed. The Royal College of Obstetricians and Gynaecologists, London 2013 http://www.nice.org.uk/guidance/cg171/resources/cg171-urinary-incontinence-in-women-full-guideline3
Balchandra P, Rogerson L (2014) Women’s perspective: intra-detrusor Botox® versus sacral neuromodulation for overactive bladder symptoms after unsuccessful anticholinergic treatment. Int Urogynecol J 25(8):1059–1064
Rudd I, Kavia R, Jenks J et al (2012) Patient treatment preferences for symptomatic refractory urodynamic idiopathic detrusor overactivity (IDO) [Abstract]. BJU Int 109(Suppl. 7):45
Flynn TN (2010) Valuing citizen and patient preferences in health: recent developments in three types of best–worst scaling. Expert Rev Pharmacoecon Outcomes Res 10(3):259–267
Bridges J, Kinter E, Schmeding A et al (2011) Can patients diagnosed with schizophrenia complete choice-based conjoint analysis tasks. Patient 4:267–275
Umberger W, Stringer R, Mueller SC (2010) Selected paper prepared for presentation at the agricultural & applied economics. Using Best–Worst Scaling to Determine Market Channel Choice by Small Farmers in Indonesia. Association 2010 AAEA, CAES, & WAEA Joint Annual Meeting, Denver, Colorado, 25–27 July 2010
IBM Corp. Released (2013) IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp http://www-01.ibm.com/support/docview.wss?uid=swg21476197
Peay HL, Hollin I, Fischer R, Bridges JF (2014) A community-engaged approach to quantifying caregiver preferences for the benefits and risks of emerging therapies for Duchenne muscular dystrophy. Clin Ther 36(5):624–637
Reed Johnson F, Van Houtven G, Ozdemir S et al (2009) Multiple sclerosis patients benefit-risk preferences serious adverse event risks versus treatment efficacy. J Neurol 256:554–562
Beusterien K, Davies J, Leach M et al (2010) Population preference values for treatment outcomes in chronic lymphocytic leukaemia: a cross-sectional utility study. Health Qual Life Outcomes 8:50
Beusterien K, Szabo S, Kotapati S et al (2009) Societal preference values for advanced melanoma health states in the United Kingdom and Australia. Br J Cancer 101(3):387–389
Acknowledgments
The authors would like to thank Global Perspectives for their assistance with patient recruitment.
Funding
This study was funded by Medtronic (Minneapolis, MN). Medtronic manufactures equipment for sacral nerve stimulation, which is one of the treatment options studied.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Hashim Hashim has served as a Mentor for Medtronic and as a Speaker and Mentor for Allergan. Kathleen Beusterien is founder of ORS Health, which consults for Medtronic. Kaitlan Amos works for ORS Health, which provides consulting services to Medtronic. John Bridges declares that he has no conflict of interest. Linda Cardozo declares that she has no conflict of interest.
Ethical approval
All procedures performed were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by a commercial IRB that covers studies in the UK (Magil IRB; Rockville, MD).
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Handling editor: Dr. Ananias C. Diokno.
Rights and permissions
About this article
Cite this article
Hashim, H., Beusterien, K., Bridges, J.F.P. et al. Patient preferences for treating refractory overactive bladder in the UK. Int Urol Nephrol 47, 1619–1627 (2015). https://doi.org/10.1007/s11255-015-1100-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11255-015-1100-3