Abstract
Purpose
In this study, we developed Danish utility weights for the European Organisation for Research and Treatment of Cancer (EORTC) QLU-C10D, a cancer-specific utility instrument based on the EORTC QLQ-C30.
Methods
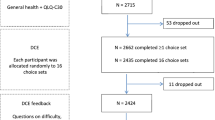
Following a standardized methodology, 1001 adult participants from the Danish general population were quota-sampled and completed a cross-sectional web-based survey and discrete choice experiment (DCE). In the DCE, participants considered 16 choice sets constructed from the key 10 dimensions of the QLU-C10D and chose their preferred health state for each one. Utility weights were calculated using conditional logistic regression with correction for non-monotonicity.
Results
The sample (n = 1001) was representative of the Danish general population with regard to age and gender. The domains with the largest utility decrements, i.e., the domains with the biggest impact on health utility, were physical functioning (− 0.224), pain (− 0.160), and role functioning (− 0.136). The smallest utility decrements were observed for the domains lack of appetite (− 0.024), sleep disorders (− 0.057), and fatigue (− 0.064). Non-monotonicity of severity levels was observed for the domains sleep disturbances, lack of appetite, and bowel problems. Deviations from monotonicity were not statistically significant.
Conclusion
The EORTC QLU-C10D is a relatively new multi-attribute utility instrument and is a promising cancer-specific health technology assessment candidate measure. The country-specific Danish utility weights from this study can be used for cost-utility analyses in Danish patients and for comparison with other country-specific utility data.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
In healthcare systems with finite resources, cost-utility analyses (CUA) are recommended to supplement decision-making on which treatments should be prioritized and reimbursed to maximize societal healthcare benefits [5]. To evaluate the benefits of new or existing treatments in the context of CUA, quality-adjusted life years (QALYs) are used. QALYs consider not only the length of duration spent in a health state (i.e., in cancer often time until death) but also weigh-in individuals’ health-related quality of life (HRQOL). In this framework, individual health states can vary on a level between perfect health (1) and a value equal to being dead (0). Values below 0, indicating a health state perceived as worse than being dead, are possible as well in some instances [10]. In other words, such a health state would be so poor that death would be preferable over living in that state and the utility value assigned to this health state is negative [42]. The QALY metric is used in CUA and provides more comprehensive information on the actual costs and benefits of different treatments. Especially in cancer care, where incremental survival gains of new treatments can be low and treatment costs are steadily rising [37], considering patient HRQOL in CUA is crucial to a comprehensive analysis.
Preference-based measures (PBMS) are frequently used to determine the preferences different populations assign to different aspects of HRQOL. They can be generic, like the EQ-5D [12] or the Short-Form 6 Dimensions (SF-6D) [3, 6], which allows them to be used and compared across different populations and condition groups. At the same time, these PBMs may be less suitable for some cancer populations as they may be less capable to measure specific issues or aspects of diseases that may be particular to certain populations [4, 13, 27]. Disease-specific PBMs can favorably be used to capture such domains [26].
To meet the demand for disease-specific PBMs, the European Organisation for Research and Treatment of Cancer (EORTC) and the Multi-Attribute Utility in Cancer (MAUCa) Consortium have jointly developed a new, cancer-specific PBM, the EORTC Quality of Life Core 10 Dimensions (EORTC QLU-C10D) [23]. It is based on the most widely used questionnaire in cancer clinical trials [in 66% of registered trials [17]], the EORTC Quality of Life Core Questionnaire (EORTC QLQ-C30 [1]. Based on this questionnaire, the QLU-C10D covers both general functioning domains and cancer-specific symptoms.
To calculate health utilities for different populations, utility weights, which represent the health preferences of that population, are required. Utility weights can be calculated on the general population level by using preference-based methods such as standard gamble, time trade-off, and discrete choice experiments (DCEs), where DCEs are one of the most widely used methods in diverse populations [5]. As different countries and healthcare systems have different approaches to health economic evaluations and CUA [11] and health state preferences are known to differ between countries [15], country-specific utility weights should be used where available and required by agencies. For the QLU-C10D, utility weights have already been established for a number of European countries [14, 15, 18, 20, 30], Australia [24], the United States [36], Canada [29], and first Asian countries [28].
In this study, we developed utility weights for the EORTC QLU-C10D for Denmark. Historically, Danish regulators and payers consider CUA for health policy decision-making, but CUA are not mandatory for the approval or prescription of treatments [8, 38]. Notably, in 2021, the Danish Health Technology Council (Behandlingsrådet) was founded with the goal to target healthcare resources at the technologies and treatments that provide the best value for money [8]. It is expected that the evaluations by the Health Technology Council will have a major impact on the future use of technologies and healthcare devices in Denmark [8]. Regarding the assessment of HRQOL and QALYs, the Health Technology Council states that “it is not possible to give a standardized approach to how applicants can or should collect data on patients’ health-related quality of life, including which instruments are best suited for specific evaluations” [7]. However, instrument-specific validation studies in the Danish population are required for an instrument to be considered [7], which we aim to provide in the present study.
Methods
Study design and sample
For this study, we followed the methods for the generation of utility weights established by King et al. [24] which were also used in the valuation surveys for other countries [14, 15, 18, 20, 30]. In this cross-sectional valuation survey, participants from the Danish general population were recruited via a third-party provider online panel (https://surveyengine.com/). Participants of the survey received a small payment for their participation. We used quota sampling to obtain representativeness of the sample with regard to sex and age based on United Nations census data for Denmark [40].
All participants provided electronically signed informed consent and the study was approved by the Ethics Committee of the Medical University of Innsbruck (approval number 1079/2023).
Survey
The survey comprised the assessment of sociodemographic data, basic clinical data (chronic diseases), the EORTC QLQ-C30, the DCE to establish Danish utility weights, the EQ-5D-5L [34], and the Kessler psychological distress scale [22]. The EQ-5D-5L and the K10 were not evaluated in this paper.
EORTC QLQ-C30 and EORTC QLU-C10D
The EORTC QLU-C10D is a utility scoring algorithm that was developed by the MAUCa Consortium and the EORTC based on the EORTC QLQ-C30 [23]. The QLQ-C30 is a 30-item questionnaire for patients with cancer. It assesses functional health (physical functioning, role functioning, social functioning, emotional functioning, cognitive functioning), symptom burden (fatigue, pain, nausea/vomiting, sleep disturbances, dyspnea, appetite loss, constipation, diarrhea, financial impact), and global health/quality of life. For the QLU-C10D, 10 key domains from the QLQ-C30 were selected: physical functioning, role functioning, social functioning, emotional functioning, pain, fatigue, sleep disturbances, appetite loss, nausea, and bowel problems (which merges the constipation and diarrhea scales from the QLQ-C30). As in the QLQ-C30, items in the QLU-C10D have four possible levels ranging from “Not at all” to “Very much” impairment in that domain. With 10 domains with each four levels of severity, the QLU-C10D covers a total of 4^10 = 1,048,576 different health states. Supplementary Table 1 shows the classification system of the QLU-C10D. The robustness of the QLU-C10D methodology and its psychometric properties like test–retest reliability have been demonstrated in past studies [16, 31, 33].
Due to its basis on the QLQ-C30, the QLU-C10D is backward-compatible with the QLQ-C30, meaning that health utilities can be calculated from QLQ-C30 data if utility weights for the respective population are available.
Discrete choice experiment (DCE)
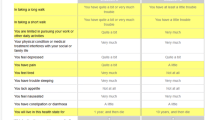
Utilities were elicited by DCE in this study, which was constructed analogously to the one used by King et al. [24]. Out of a set of 960 possible choice sets, participants were randomly assigned to complete 16 choice sets to limit participant burden. For each choice set, participants had to choose one of two scenarios. Scenarios were set up and described based on the 10 domains from the QLU-C10D and also included survival time as an anchor. Survival time varied between 1, 2, 5, or 10 years (wording: “You live in this health state for X years, and then die”). To keep the choice sets comparable and participant burden acceptable, the scenarios of a single choice set only differed in 5 out of the 11 aspects (10 QLU-10D domains and survival time) which was previously found to be an adequate format [33]. The differing aspects were highlighted to increase their visibility for participants. See Supplementary Fig. 1 for an example of the DCE display in English language.
In the DCE section of the survey, randomization occurred at two levels: (i) each participant was assigned 16 choice sets out of the 960 available without duplication; (ii) the assignment of options as Situation A or B within each choice set was randomized to minimize potential ordering biases. It is worth noting that the presentation order of dimensions remained consistent, as prior research indicated that dimension order did not consistently impact the utility weights for the QLU-C10D [31].
Statistical analysis
Descriptive statistics are reported for the sample characteristics (i.e., demographic information, clinical information). Chi-square tests were used to compare the sample characteristics of gender, age, and education with national census data [39]. To calculate utility weights, we followed an established procedure [2] that was also used in previous studies on the EORTC QLU-C10D, [15, 18, 33]. The utility (U) of an option j in the choice set s for a respondent i can be described by the following formula:
TIMEisj is the survival time in option j and X’isj is a set of dummies related to the levels of the corresponding health state. Errors (εisj) are assumed to be independent and identically Gumbel-distributed [2, 24]. DCE data were analyzed using a conditional logit model with cluster sandwich estimators to adjust for correlated observations within respondents. Analogous to previous valuation studies, estimates were converted into utility decrements based on the ratio of health state parameters (β) and the time coefficient (α) to reflect the trade-off between HRQOL and survival. Finally, we ran an additional analysis to correct for non-monotonic levels in the EORTC QLU-C10D utility weights (i.e., for domains where the severity levels did not show an increasing decrement in utility weight) in line with previous valuation studies.
In a recent review of DCE studies in health state valuation by Wang et al. [41], the majority of studies (48/65, 74%) used conditional logit models. In our study, we also relied on a conditional logit models because its parameterization is more suited our purpose (for public decision-making) compared to mixed logit models that focus on the distribution of individual preferences. Analyses were run using SPSS version 27.0 (IBM Corp., Armonk, NY, USA).
Data quality checks
We recorded the total time it took respondents to complete the survey and the number of participants that only chose the A or only chose the B option in the DCE. We also computed an additional model in which we excluded the fastest 10% of participants and compared that to the model with all participants.
Results
Survey completion
Between 04.08.2021 and 24.08.2021, 1744 participants initiated the survey. Of those, 269 (15.4%) participants were excluded due to the quota sampling, 417 (23.9%) were excluded due to timing out (being idle mid-survey for too long and not progressing further in the survey), and 57 (3.3%) were excluded because they did not finish the survey (actively closed the survey before completion). The final sample consisted of 1001 participants.
Socio-demographic characteristics
Socio-demographic and data on chronic diseases are shown in Table 1. For gender and age, the sample was representative of the Danish general population (both p > 0.975). Regarding education, the sample showed significantly higher education levels compared to the general population (p < 0.001) and most participants had upper secondary (47.8%) or tertiary education (41.9%). Most participants (59.9%) reported being married or in a steady relationship. About one-third (35.5%) of participants reported having at least one chronic disease. The most commonly reported diseases were arthritis or rheumatism (11.0%), respiratory diseases (10.4%), and diabetes (8.7%).
Feedback question regarding the discrete choice experiments
Participants reported using various strategies to choose between health states. The most common strategies were focusing on the highlighted aspects which differed between the two health states (33%), thinking about most of the aspects (25%) and focusing on only a few selected aspects (15%). Among those who used a different strategy (n = 165), most reported via open text that they focused on the desire to live as long as possible (68%) or live with less symptom burden (13%).
Utility decrements and calculation of QLU-C10D utilities
The DCE analyses without correction for monotonicity are shown in Fig. 1 and Table 2. The analyses with correction for monotonicity are shown in Fig. 2 and Table 2. We report the utility decrements for each domain and severity level. For the level “not at all” (i.e., no impairment), the decrement is, by definition, 0. Actual utilities corresponding to individual health states can be calculated by subtracting the decrements from Table 2 from 1. For example, the utility for a health state where all domains would have a severity level of “quite a bit” (33333 33333), based on the utility decrements with correction for monotonicity, would be calculated as follows:
The utility score for the worst possible health state (44444 44444), or PITS state (i.e., worst attainable health), is calculated as follows:
The largest utility decrements for the severity level “very much” were observed for the domains physical functioning (− 0.224), pain (− 0.160), role functioning (− 0.136), and emotional functioning (− 0.124). Notably, the cancer-specific domains nausea (− 0.101) and bowel problems (− 0.102) also had decrements around − 0.1. The smallest utility decrements for the severity level “very much” were observed for the domains lack of appetite (− 0.024), sleep disorders (− 0.057), and fatigue (− 0.064). The overall rank order of domains for the other severity levels was similar.
Non-monotonicity of levels was observed for the domains sleep disorders, lack of appetite, and bowel problems. However, none of the deviations from monotonicity were statistically significant. In the model adjusted for monotonicity, the levels showing non-monotonicity were set to be equal (e.g., sleep disorders level 3 = level 4).
Data quality checks
The mean time to complete the survey was 16.0 min with a standard deviation of 10.0 min (median 13.6, inter-quartile range 9.5–19.7 min). Excluding the fastest 10% of respondents (≤ 7.03 min) from the analysis did not change the utility decrements and results were almost identical with the analysis that included all respondents (complete data available upon request from the authors).
Few respondents (1.7% of 1001) chose either only the A or only the B option in the DCE, which is comparable to our previous studies [36].
Discussion
In this study, we developed Danish utility weights for the EORTC QLU-C10D from a sample of the general population. We recruited a panel sample that was representative of the Danish general population in regard to age and gender. The domains with the largest utility decrements that had the biggest impact on health utility were physical functioning, pain, and role functioning.
The EORTC QLU-C10D and relevance for Denmark
The Danish healthcare system combines universal protection and equal access to healthcare for all citizens, providing high-quality services free of charge. It promotes, among other things, preventive examinations for some diseases, especially to detect cancer in early stages and provide better treatments to patients. The total socioeconomic cost of Danish cancer patients is approximately DKK 12 billion (or roughly € 1.6 billion) over a 5-year period, including direct healthcare costs, and lost income for patients and potential partners [25]. These costs are expected to increase due to the increased incidence of cancer, and therefore, the EORTC QLU-C10D may facilitate cost-utility analysis of cancer interventions in different healthcare settings. Further instructions on how to use the EORTC QLU-C10D can be found in the EORTC user manual by Gamper et al. (https://qol.eortc.org/manual/eortc-qlu-c10d-manual/).
The EORTC QLU-C10D is a relatively new multi-attribute utility instrument (MAUI) and is a promising candidate measure that is cancer-specific. Compared to generic MAUIs like the EQ-5D which offer the advantage of making comparisons between certain condition groups, specific MAUIs might more effectively capture aspects that are particular to a certain condition or disease. A 2020 review of health utility instruments that are used and recommended by national health technology assessment (HTA) guidelines found that generic MAUIs (meaning not focused on a specific disease) like the EQ-5D are still preferred in half of the reviewed guidelines [21]. However, the review also found that about half of the national guidelines do not express a preference for a specific MAUI but do recommend calculating utilities using national preference weights. This highlights the necessity for national utility weights for different countries. In this context, two Danish value sets are available for the EQ-5D-3L [43] and the EQ-5D-5L [19] but so far, no dataset was available for the EORTC QLU-C10D. One considerable advantage of the EORTC QLU-C10D is that it can be used in any cancer trial that assesses the EORTC QLQ-C30, which is the most commonly used quality of life questionnaire in published and registered clinical trials by a large margin [17]. In other words, the EORTC QLU-C10D health utilities can be calculated using patients' EORTC QLQ-C30 scores, even retrospectively for trials that have already been closed. We strongly encourage future analyses of trials using EORTC QLQ-C30 data based on the growing body of utility weights available for the EORTC QLU-C10D [15, 18, 20, 24, 30, 32, 36].
As part of the ongoing efforts to provide utility weights for the EORTC QLU-C10D, we calculated national utility weights for Denmark. The Danish Medicines Council guidelines for methods to assess new pharmaceutical states that QALYs should be used to summarize findings from health economic analyses [9] based on national weights. Sensitivity analyses are recommended if both a generic MAUI (like the EQ-5D) and disease-specific MAUI like the EORTC QLU-C10D are available [9]. With the foundation of the Danish Health Technology Council in 2021 [7], we expect a growing importance of HTA in Denmark in the near future.
Danish utility weights and comparison to other countries
Generally, utility decrements for the EORTC QLU-C10D and the rank order of domains were similar to other European countries. Several of the findings merit in-depth discussion. In our sample, the utility decrement for physical functioning was the largest, which was also the domain with the largest decrement for many other countries; the decrement was comparable to Austria [15], Australia [24], and smaller when compared to Italy and Poland [15]. Following physical functioning, the domain with the second largest decrement was pain, which is a pattern that was, for example, also observed in, for example, Austria [15], Germany [20], Spain [14], France [30], and the United Kingdom [32].
Compared to many other countries however [14, 15], the domain with the third largest decrement in the Danish utility weights was not role functioning but emotional functioning. In general, the decrement for emotional functioning was large with − 0.124, indicating that emotional outcomes are more highly valued or considered to have a strong impact on health in the Danish population. In international comparison, only France [30], the United Kingdom [32], and Australia [24] show larger decrements for emotional functioning. Most other countries have a lower decrement for this domain [15, 18, 20, 36]. This might also be influenced by the translation of the domain, which was “Du føler dig deprimeret” and is a strong wording considered a paronym for depression in a more clinical or diagnostic sense compared to “feeling down.” However, similar wordings were also used in other countries that did not show large decrements for this domain, like the USA (“You feel depressed”) [36] or Italy (“Soffre di depressione”) [15]. Social functioning was also valued similarly high as emotional functioning at − 0.104 for the highest level, with the decrements for the lower two levels being slightly larger than the corresponding levels for emotional functioning.
Some of the domains that are considered cancer-specific like bowel problems (diarrhea, constipation) and nausea had decrements around − 0.1. These are larger than in other countries like Germany [20], Austria, Italy, and Poland [15] and similar to the Netherlands [18] and Australia [24]. Three other domains fatigue, lack of appetite, and sleep disturbances were associated with smaller utility decrements. This was also observed in other countries [15, 18, 20]. One potential explanation is that, while people from the general population do experience occasional fatigue-like symptoms or lack of appetite or sleep disturbances, they cannot relate to severe, cancer or therapy-induced fatigue or lack of appetite [36]. It is possible that patients with cancer who have actually experienced those symptoms as a consequence of antineoplastic therapy would assign a different weight to these domains. Evaluations to derive comparable utility weights from a patient population are currently ongoing.
The worst possible health state (PITS state) with the highest level of impairments in all domains had a negative value of − 0.096, indicating that it was perceived as worse than being dead in our population. This is similar to the value of the PITS state in Australia (− 0.096) [24] and the United Kingdom (− 0.083) [32].
Strengths and limitations
One strength of our study is the large sample that was representative of the Danish general population with regard to age and gender. Moreover, we followed an established methodology to calculate the utility weights [23]. This enables cross-country comparisons of utility weights as preferences have been shown to differ between countries [35]. One limitation of our study is that the sample had a higher proportion of highly educated people compared to the general population which was also found in the evaluations of other countries [20, 36] and it is unknown if different health preferences exist in different subpopulations (e.g., in groups with different education levels). Another limitation is that we do not have sociodemographic information on respondents that did not complete the survey and who were excluded from the analysis as those respondents mostly did not complete the questions on sociodemographic information.
Non-monotonicity was found for some of the domains with smaller weights. However, none of these deviations from monotonicity were statistically significant and all could be corrected in the analysis. Finally, another possible limitation of this study is the potential cognitive burden of participants due to the length of the questionnaires included in the survey, since about a third of those who began the survey did not complete it and were excluded from the analysis.
Conclusion
In this study, we successfully developed Danish general population utility weights that can be used for CUA. Our study adds to a growing body of literature on the EORTC QLU-C10D, a cancer-specific utility instrument based on the EORTC QLQ-C30.
Data availability
Data for this study are available upon reasonable request from the EORTC Headquarters. Available at: https://www.eortc.be/services/forms/erp/request.aspx.
References
Aaronson, N. K., Ahmedzai, S., Bergman, B., Bullinger, M., Cull, A., Duez, N. J., Filiberti, A., Flechtner, H., Fleishman, S. B., & de Haes, J. C. (1993). The European Organization for Research and Treatment of Cancer QLQ-C30: A quality-of-life instrument for use in international clinical trials in oncology. Journal of the National Cancer Institute, 85(5), 365–376. https://doi.org/10.1093/jnci/85.5.365
Bansback, N., Brazier, J., Tsuchiya, A., & Anis, A. (2012). Using a discrete choice experiment to estimate health state utility values. Journal of Health Economics, 31(1), 306–318. https://doi.org/10.1016/j.jhealeco.2011.11.004
Brazier, J. E., & Roberts, J. (2004). The estimation of a preference-based measure of health from the SF-12. Medical Care, 42(9), 851–859. https://doi.org/10.1097/01.mlr.0000135827.18610.0d
Brazier, J. E., Rowen, D., Mavranezouli, I., Tsuchiya, A., Young, T., Yang, Y., Barkham, M., & Ibbotson, R. (2012). Developing and testing methods for deriving preference-based measures of health from condition-specific measures (and other patient-based measures of outcome). Health Technology Assessment (Winchester, England), 16(32), 1–114. https://doi.org/10.3310/hta16320
Brazier, J., Ratcliffe, J., Saloman, J., & Tsuchiya, A. (2017). Measuring and valuing health benefits for economic evaluation. Oxford University Press.
Brazier, J., Roberts, J., & Deverill, M. (2002). The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics, 21(2), 271–292.
Danish Health Technology Council. (2021a). The Danish Health Technology Council’s methods guide for the evaluation of health technology. https://behandlingsraadet.dk/media/otjfhhzw/the-danish-health-technology-council-s-methods-guide-for-the-evaluation-of-health-technology.pdf
Danish Health Technology Council. (2021b). The Danish Health Technology Council’s process guide. https://behandlingsraadet.dk/media/2tubtbn2/the-danish-health-technology-council-s-process-guide.pdf
Danish Medicines Council. (2021). The Danish Medicines Council methods guide for assessing new pharmaceuticals. https://medicinraadet.dk/media/wq0dxny2/the_danish_medicines_council_methods_guide_for_assessing_new_pharmaceuticals_version_1-2_adlegacy.pdf
Drummond, M. F., Aguiar-Ibanez, R., & Nixon, J. (2006). Economic evaluation. Singapore Medical Journal, 47(6), 456–461; quiz 462.
EUnetHTA Joint Action 2, Work Package 7, Subgroup 3, Heintz, E., Gerber-Grote, A., Ghabri, S., Hamers, F. F., Rupel, V. P., Slabe-Erker, R., & Davidson, T. (2016). Is there a European view on health economic evaluations? Results from a synopsis of methodological guidelines used in the EUnetHTA partner countries. PharmacoEconomics, 34(1), 59–76. https://doi.org/10.1007/s40273-015-0328-1
EuroQol Group. (1990). EuroQol—a new facility for the measurement of health-related quality of life. Health Policy, 16(3), 199–208.
Finch, A. P., Brazier, J. E., & Mukuria, C. (2018). What is the evidence for the performance of generic preference-based measures? A systematic overview of reviews. The European Journal of Health Economics, 19(4), 557–570. https://doi.org/10.1007/s10198-017-0902-x
Finch, A. P., Gamper, E., Norman, R., Viney, R., Holzner, B., King, M., Kemmler, G., EORTC Quality of Life Group. (2021). Estimation of an EORTC QLU-C10 value SET for Spain using a discrete choice experiment. PharmacoEconomics, 39(9), 1085–1098. https://doi.org/10.1007/s40273-021-01058-x
Gamper, E. M., King, M. T., Norman, R., Efficace, F., Cottone, F., Holzner, B., Kemmler, G., European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group. (2020). EORTC QLU-C10D value sets for Austria, Italy, and Poland. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 29(9), 2485–2495. https://doi.org/10.1007/s11136-020-02536-z
Gamper, E.-M., Holzner, B., King, M. T., Norman, R., Viney, R., Nerich, V., & Kemmler, G. (2018). Test–retest reliability of discrete choice experiment for valuations of QLU-C10D health states. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 21(8), 958–966. https://doi.org/10.1016/j.jval.2017.11.012
Giesinger, J. M., Efficace, F., Aaronson, N., Calvert, M., Kyte, D., Cottone, F., Cella, D., & Gamper, E.-M. (2021). Past and current practice of patient-reported outcome measurement in randomized cancer clinical trials: A systematic review. Value in Health, 24(4), 585–591. https://doi.org/10.1016/j.jval.2020.11.004
Jansen, F., Verdonck-de Leeuw, I. M., Gamper, E., Norman, R., Holzner, B., King, M., Kemmler, G., European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group. (2021). Dutch utility weights for the EORTC cancer-specific utility instrument: The Dutch EORTC QLU-C10D. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 30(7), 2009–2019. https://doi.org/10.1007/s11136-021-02767-8
Jensen, C. E., Sørensen, S. S., Gudex, C., Jensen, M. B., Pedersen, K. M., & Ehlers, L. H. (2021). The Danish EQ-5D-5L value set: A hybrid model using cTTO and DCE data. Applied Health Economics and Health Policy, 19(4), 579–591. https://doi.org/10.1007/s40258-021-00639-3
Kemmler, G., Gamper, E., Nerich, V., Norman, R., Viney, R., Holzner, B., King, M., European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group. (2019). German value sets for the EORTC QLU-C10D, a cancer-specific utility instrument based on the EORTC QLQ-C30. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 28(12), 3197–3211. https://doi.org/10.1007/s11136-019-02283-w
Kennedy-Martin, M., Slaap, B., Herdman, M., van Reenen, M., Kennedy-Martin, T., Greiner, W., Busschbach, J., & Boye, K. S. (2020). Which multi-attribute utility instruments are recommended for use in cost-utility analysis? A review of national health technology assessment (HTA) guidelines. The European Journal of Health Economics: HEPAC: Health Economics in Prevention and Care, 21(8), 1245–1257. https://doi.org/10.1007/s10198-020-01195-8
Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S.-L.T., Walters, E. E., & Zaslavsky, A. M. (2002). Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32(6), 959–976. https://doi.org/10.1017/S0033291702006074
King, M. T., Costa, D. S. J., Aaronson, N. K., Brazier, J. E., Cella, D. F., Fayers, P. M., Grimison, P., Janda, M., Kemmler, G., Norman, R., Pickard, A. S., Rowen, D., Velikova, G., Young, T. A., & Viney, R. (2016). QLU-C10D: A health state classification system for a multi-attribute utility measure based on the EORTC QLQ-C30. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 25(3), 625–636. https://doi.org/10.1007/s11136-015-1217-y
King, M. T., Viney, R., Simon Pickard, A., Rowen, D., Aaronson, N. K., Brazier, J. E., Cella, D., Costa, D. S. J., Fayers, P. M., Kemmler, G., McTaggart-Cowen, H., Mercieca-Bebber, R., Peacock, S., Street, D. J., Young, T. A., Norman, R., MAUCa Consortium. (2018). Australian utility weights for the EORTC QLU-C10D, a multi-attribute utility instrument derived from the Cancer-Specific Quality of Life Questionnaire, EORTC QLQ-C30. PharmacoEconomics, 36(2), 225–238. https://doi.org/10.1007/s40273-017-0582-5
Kruse, M. H. G., & Hostenkamp, G. (2016). De samfundsøkonomiske omkostninger ved kræft. Societal Economic Cost of Cancer. COHERE, Center for Sundhedsøkonomisk Forskning, Syddansk (in Danish)
Lin, F.-J., Longworth, L., & Pickard, A. S. (2013). Evaluation of content on EQ-5D as compared to disease-specific utility measures. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 22(4), 853–874. https://doi.org/10.1007/s11136-012-0207-6
Longworth, L., Yang, Y., Young, T., Mulhern, B., Hernández Alava, M., Mukuria, C., Rowen, D., Tosh, J., Tsuchiya, A., Evans, P., DevianeeKeetharuth, A., & Brazier, J. (2014). Use of generic and condition-specific measures of health related quality of life in NICE decision-making: Systematic review, statistical modeling and survey. Health Technology Assessment, 18(9), 1–224. https://doi.org/10.3310/hta18090
Luo, N. (2019). Preferences for quality of life in oncology: Are cancer patients and the general population different? In Abstract presented at the 26th ISOQOL annual conference.
McTaggart-Cowan, H., King, M. T., Norman, R., Costa, D. S. J., Pickard, A. S., Regier, D. A., Viney, R., & Peacock, S. J. (2019). The EORTC QLU-C10D: The Canadian Valuation Study and algorithm to derive cancer-specific utilities from the EORTC QLQ-C30. MDM Policy & Practice, 4(1), 2381468319842532. https://doi.org/10.1177/2381468319842532
Nerich, V., Gamper, E. M., Norman, R., King, M., Holzner, B., Viney, R., & Kemmler, G. (2021). French value-set of the QLU-C10D, a cancer-specific utility measure derived from the QLQ-C30. Applied Health Economics and Health Policy, 19(2), 191–202. https://doi.org/10.1007/s40258-020-00598-1
Norman, R., Kemmler, G., Viney, R., Pickard, A. S., Gamper, E., Holzner, B., Nerich, V., & King, M. (2016). Order of presentation of dimensions does not systematically bias utility weights from a discrete choice experiment. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 19(8), 1033–1038. https://doi.org/10.1016/j.jval.2016.07.003
Norman, R., Mercieca-Bebber, R., Rowen, D., Brazier, J. E., Cella, D., Pickard, A. S., Street, D. J., Viney, R., Revicki, D., King, M. T., On behalf of the European Organisation for Research and Treatment of Cancer (EORTC) Quality of Life Group and the MAUCa Consortium. (2019). U.K. utility weights for the EORTC QLU-C10D. Health Economics, 28(12), 1385–1401. https://doi.org/10.1002/hec.3950
Norman, R., Viney, R., Aaronson, N. K., Brazier, J. E., Cella, D., Costa, D. S. J., Fayers, P. M., Kemmler, G., Peacock, S., Pickard, A. S., Rowen, D., Street, D. J., Velikova, G., Young, T. A., & King, M. T. (2016). Using a discrete choice experiment to value the QLU-C10D: Feasibility and sensitivity to presentation format. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation, 25(3), 637–649. https://doi.org/10.1007/s11136-015-1115-3
Pickard, A. S., De Leon, M. C., Kohlmann, T., Cella, D., & Rosenbloom, S. (2007). Psychometric comparison of the standard EQ-5D to a 5 level version in cancer patients. Medical Care, 45(3), 259–263. https://doi.org/10.1097/01.mlr.0000254515.63841.81
Pilz, M. J., Nolte, S., Liegl, G., King, M., Norman, R., McTaggart-Cowan, H., Bottomley, A., Rose, M., Kemmler, G., Holzner, B., Gamper, E. M., EORTC Quality of Life Group. (2022). The European Organisation for Research and Treatment of Cancer Quality of Life Utility-Core 10 dimensions: Development and investigation of general population utility norms for Canada, France, Germany, Italy, Poland, and the United Kingdom. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, S1098–3015(22), 04783. https://doi.org/10.1016/j.jval.2022.12.009
Revicki, D. A., King, M. T., Viney, R., Pickard, A. S., Mercieca-Bebber, R., Shaw, J. W., Müller, F., & Norman, R. (2021). United States utility algorithm for the EORTC QLU-C10D, a multi-attribute utility instrument based on a cancer-specific quality-of-life instrument. Medical Decision Making: An International Journal of the Society for Medical Decision Making, 41(4), 485–501. https://doi.org/10.1177/0272989X211003569
Saluja, R., Arciero, V. S., Cheng, S., McDonald, E., Wong, W. W. L., Cheung, M. C., & Chan, K. K. W. (2018). Examining trends in cost and clinical benefit of novel anticancer drugs over time. Journal of Oncology Practice, 14(5), e280–e294. https://doi.org/10.1200/JOP.17.00058
Sigmund, H., & Kristensen, F. B. (2002). Does health technology assessment benefit health services and politics? The experiences of an established HTA institution: The Danish Centre for Evaluation and HTA. The European Journal of Health Economics, 3(1), 54–58.
Statistics Denmark. (2022). Population figures. https://www.dst.dk/en/Statistik/emner/borgere/befolkning/befolkningstal
UNdata. (2022). Population by age, sex and urban/rural residence. http://data.un.org/Data.aspx?d=POP&f=tableCode%3a22
Wang, H., Rowen, D. L., Brazier, J. E., & Jiang, L. (2023). Discrete choice experiments in health state valuation: A systematic review of progress and new trends. Applied Health Economics and Health Policy, 21(3), 405–418. https://doi.org/10.1007/s40258-023-00794-9
Weinstein, M. C., Torrance, G., & McGuire, A. (2009). QALYs: The basics. Value in Health: The Journal of the International Society for Pharmacoeconomics and Outcomes Research, 12(Suppl 1), S5–S9. https://doi.org/10.1111/j.1524-4733.2009.00515.x
Wittrup-Jensen, K. U., Lauridsen, J., Gudex, C., & Pedersen, K. M. (2009). Generation of a Danish TTO value set for EQ-5D health states. Scandinavian Journal of Public Health, 37(5), 459–466. https://doi.org/10.1177/1403494809105287
Acknowledgements
The authors thank all participants for their valuable time and effort. The authors thank the European Organisation for Research and Treatment of Cancer Quality of Life Group (EORTC QLG), specifically the health technology assessment workgroup, for support with the study. The study followed an established methodology that was developed by the MAUCa Consortium and the EORTC QLG. Multi-Attribute Utility in Cancer (MAUCa) Consortium members: Neil Aaronson, John Brazier, David Cella, Daniel Costa, Peter Fayers, Peter Grimison, Monika Janda, Georg Kemmler, Madeleine King (Chair), Nan Luo, Helen McTaggart-Cowan, Rebecca Mercieca-Bebber, Richard Norman, Dennis Revicki, Stuart Peacock, Simon Pickard, Donna Rowen, Galina Velikova, Rosalie Viney, Deborah Street, and Tracey Young.
Funding
Open access funding provided by University of Innsbruck and Medical University of Innsbruck. Funding for this study was provided by the EORTC Quality of Life Group (Grant Number 001-2018). The EORTC Quality of Life Group business model involves charges for commercial companies using EORTC instruments. Academic use of EORTC instruments is free of charge.
Author information
Authors and Affiliations
Consortia
Contributions
JL participated in the analysis of data, wrote the first version of the manuscript, and was study coordinator on the project. LRC wrote the first version of the manuscript and participated in the analysis of data. MAP, BH, RN, and MK participated in study conceptualization and preparation, analysis of the data and critically revised the manuscript. GK supervised the study, lead the study conceptualization and preparation, analysis of the data, and critically revised the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
R.N. is a member of the EuroQol Group. L.R.C., M.A.P., B.H., M.K., J.L., and G.K. are members of the EORTC Quality of Life Group. The authors declare no conflicts of interest.
Ethical approval
The study was conducted in accordance with the Declaration of Helsinki.
Informed consent
All participants provided electronically signed informed consent. The study was approved by the Medical University of Innsbruck Ethics Committee (Approval Number 1079/2023).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lehmann, J., Rojas-Concha, L., Petersen, M.A. et al. Danish value sets for the EORTC QLU-C10D utility instrument. Qual Life Res 33, 831–841 (2024). https://doi.org/10.1007/s11136-023-03569-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03569-w