Abstract
Objective
This study aimed to translate and culturally adapt the standardized outcomes in nephrology–hemodialysis fatigue (SONG–HD fatigue) scale and to assess the psychometric properties of the Chinese version of the SONG–HD fatigue (C-SONG–HD fatigue) scale.
Methods
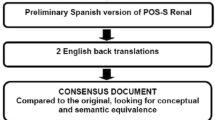
Forward and back translations were used to translate the SONG–HD fatigue scale into Chinese. We used the C-SONG–HD fatigue scale to survey Chinese patients undergoing hemodialysis (HD) in China. We examined the distribution of responses and floor and ceiling effects. Cronbach’s alpha and McDonald’s omega coefficient, intraclass coefficients, and Spearman correlations were used to assess internal consistency reliability, test–retest reliability, and convergent validity, respectively. Responsiveness was also evaluated.
Results
In total, 489 participants across southeast China, northwest China, and central China completed the study. The C-SONG–HD fatigue scale had good internal consistency (Cronbach’s alpha coefficient 0.861, omega coefficient 0.916), test–retest reliability (intraclass correlation coefficient 0.695), and convergent validity (Spearman correlation 0.691). The analysis of all first-time HD patients did not show notable responsiveness, and only patients with temporary vascular access had good responsiveness with an effect size (ES) of 0.54, a standardized response mean (SRM) of 0.85, and a standard error of measurement (SEM) of 0.77.
Conclusion
The Chinese version of the SONG–HD fatigue scale showed satisfactory reliability and validity in patients undergoing hemodialysis (HD) in China. It could be used as a tool to measure the fatigue of Chinese HD patients.
Similar content being viewed by others
Data availability
The data underlying this article are available in the article and in its online supplementary material.
References
Weisbord, S. D., Fried, L. F., Arnold, R. M., et al. (2005). Prevalence, severity, and importance of physical and emotional symptoms in chronic hemodialysis patients. Journal of the American Society of Nephrology, 16, 2487–2494.
Artom, M., Moss-Morris, R., Caskey, F., & Chilcot, J. (2014). fatigue in advanced kidney disease. Kidney International, 86, 497–505.
Jhamb, M., Pike, F., Ramer, S., Argyropoulos, C., et al. (2011). Impact of fatigue on outcomes in the hemodialysis (HEMO) study. American Journal of Nephrology, 33, 515–523.
Bossola, M., Di Stasio, E., Antocicco, M., et al. (2015). fatigue is associated with increased risk of mortality in patients on chronic hemodialysis. Nephron, 130, 113–118.
Jhamb, M., Argyropoulos, C., Steel, J. L., et al. (2009). Choices for healthy outcomes in caring for end-stage renal disease (CHOICE) study: Correlates and outcomes of fatigue among incident dialysis patients. Clinical Journal of the American Society of Nephrology, 4, 1779–1786.
Jacobson, J., Ju, A., Baumgart, A., et al. (2019). Patient perspectives on the meaning and impact of fatigue in hemodialysis: A systematic review and thematic analysis of qualitative studies. American Journal of Kidney Diseases, 74, 179–192.
Urquhart-Secord, R., Craig, J. C., Hemmelgarn, B., et al. (2016). Patient and caregiver priorities for outcomes in hemodialysis: An international nominal group technique study. American Journal of Kidney Diseases, 68, 444–454.
Kalantar-Zadeh, K., Lockwood, M. B., Rhee, C. M., et al. (2022). Patient-centred approaches for the management of unpleasant symptoms in kidney disease. Nature Reviews Nephrology. https://doi.org/10.1038/s41581-021-00518-z
Sakkas, G. K., & Karatzaferi, C. (2012). Hemodialysis fatigue just simple fatigue or a syndrome on its own right. Frontiers in Physiology, 31(3), 306.
Jhamb, M., Liang, K., Yabes, J., et al. (2013). Prevalence and correlates of fatigue in chronic kidney disease and end-stage renal disease: Are sleep disorders a key to understanding fatigue? American Journal of Nephrology, 38, 489–495.
Gregg, L. P., Jain, N., Carmody, T., et al. (2019). fatigue in non-dialysis chronic kidney disease: Correlates and association with kidney outcomes. American Journal of Nephrology, 50, 37–47.
Jhamb, M., Weisbord, S. D., Steel, J. L., & Unruh, M. (2008). fatigue in patients receiving maintenance dialysis: A review of definitions, measures, and contributing factors. American Journal of Kidney Diseases, 52(2), 353–365.
Ju, A., Teixeira-Pinto, A., Tong, A., et al. (2020). Validation of a core patient-reported outcome measure for fatigue in patients receiving hemodialysis: The SONG–HD fatigue instrument. Clinical Journal of the American Society of Nephrology, 15, 1614–1621.
Guillemin, F., Bombardier, C., & Beaton, D. (1993). Cross-cultural adaptation of health-related quality of life measures: Literature review and proposed guidelines. Journal of Clinical Epidemiology, 46(12), 1417–1432.
Wild, D., Grove, A., Martin, M., et al. (2005). Principles of good practice for the translation and cultural adaptation process for patient-reported outcomes (PRO) measures: Report of the ISPOR task force for translation and cultural adaptation. Value Health., 8(2), 94–104.
Terwee, C. B., Bot, S. D., de Boer, M. R., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42.
Yellen, S. B., Cella, D. F., Webster, K., et al. (1997). Measuring fatigue and other anemia-related symptoms with the functional assessment of cancer therapy (FACT) measurement system. Journal of Pain and Symptom Management, 13(2), 63–74.
Cella, D., Lai, J. S., Chang, C. H., et al. (2002). fatigue in cancer patients compared with fatigue in the general United States population. Cancer, 94, 528–538.
Cella, D., Yount, S., Sorensen, M., et al. (2005). Validation of the functional assessment of chronic illness therapy fatigue scale relative to other instrumentation in patients with rheumatoid arthritis. Journal of Rheumatology, 32, 811–819.
Ju, A., Unruh, M., Davison, S., et al. (2018). SONG–HD fatigue workshop collaborators: Establishing a core outcome measure for fatigue in patients on hemodialysis: A standardized outcomes in nephrology–hemodialysis (SONG–HD) consensus workshop report. American Journal of Kidney Diseases, 72, 104–112.
Wang, S. Y., Zang, X. Y., Liu, J. D., Gao, M., Cheng, M., & Zhao, Y. (2015). Psychometric properties of the functional assessment of chronic illness therapy-fatigue (FACIT-fatigue) in Chinese patients receiving maintenance dialysis. Journal of Pain and Symptom Management, 49(1), 135–143.
Cappelleri, J. C., & Bushmakin, A. G. (2014). Interpretation of patient-reported outcomes. Statistical Methods in Medical Research, 23(5), 460–483.
Green, S. B., & Yang, Y. (2008). Commentary on coefficient alpha: A cautionary tale. Psychometrika, 74, 121–135.
Flora, D. B. (2020). Your coefficient alpha is probably wrong, but which coefficient omega is right? A tutorial on using R to obtain better reliability estimates. AMPPS, 3, 484–501.
Altman Dg, S. K. M. D., & Pc, L. T. C. G. (2001). The revised CONSORT statement for reporting randomized trials: Explanation and elaboration. Annals of Internal Medicine, 134, 663–694.
Streiner, D. L., & Norman, G. R. (2003). Health measurement scales: A practical guide to their development and use (3rd ed.). Oxford University Press.
Cohen, J. (1988). Statistical power analysis for the behavioural sciences (2nd ed.). Lawrence Erlbaum Associates.
Liang, M. H., Fossel, A. H., & Larson, M. G. (1990). Comparisons of five health status instruments for orthopedic evaluation. Medical Care, 28(7), 632–642.
Fang, J. (2006). Quality of life: measurement method and application. Peking University Medical Press. in Chinese.
Crosby, R. D., Kolotkin, R. L., & Williams, G. R. (2003). Defining clinically meaningful change in health-related quality of life. Journal of Clinical Epidemiology, 56(5), 395–407.
Association, W. M. (2013). World medical association declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA, 310(20), 2191–2194.
Weldring, T., & Smith, S. M. (2013). Patient-reported outcomes (PROs) and patient-reported outcome measures (PROMs). Health Services Insights, 6, 61–68.
Erek, E., Su¨leymanlar, G., Serdengec¸ti, K., et al. (2002). Registry of the nephrologist, dialysis and transplantation in Turkey. Registry 2001. Turkish Society of Nephrology.
Letchmi, S., Das, S., Halim, H., et al. (2011). fatigue experienced by patients receiving maintenance dialysis in hemodialysis units. Nursing and Health Sciences, 13, 60–64.
Liu, H. E. (2006). fatigue and associated factors in hemodialysis patients in Taiwan. Research in Nursing and Health, 29, 40–50.
Zheng, X.-Y., Zhang, Z.-H., Cheng, Y.-M., et al. (2023). Factors associated with subgroups of fatigue in maintenance hemodialysis patients: A cross-sectional study. Renal Failure, 45(1), 2221129.
Bossola, M., & Tazza, L. (2006). Postdialysis fatigue: A frequent and debilitating symptom. Seminars in Dialysis, 29(3), 222–227.
Sklar, A. H., Riesenberg, L. A., Silber, A. K., Ahmed, W., & Ali, A. (1996). Postdialysis fatigue. American Journal of Kidney Diseases, 28, 732–736.
Horigan, A. E., & Barroso, J. V. (2016). A comparison of temporal patterns of fatigue in patients on hemodialysis. Nephrology Nursing Journal, 43, 129–138.
Acknowledgements
We are greatly indebted to Angela Ju from the Faculty of Medicine and Health, Sydney School of Public Health, the University of Sydney in Australia for her valuable guidance and great support in the process of translation, cultural adaptation, and validation of the Chinese version of the SONG–HD fatigue. The authors acknowledge all the translators’ support during the translation and cross-cultural adaption process. The authors express their appreciation to all respondents taking part in the present study and some friends for offering support in data collection.
Funding
This work was sponsored by the Fund of the Fujian Science and Technology Department (2021J01363).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
Nothing to disclose.
Ethical approval
All procedures performed in studies involving human participants followed the institutional and/or national research committee at which the studies were conducted (IRB approval number K2021-09-046) with the 1964 Helsinki Declaration and its later amendments comparable ethical standards.
Consent to participate
Informed consent was obtained from all participants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Huang, Lt., Zheng, Xy., Zhang, Zh. et al. Translation, cultural adaptation, and validation of the Chinese standardized outcomes in nephrology–hemodialysis fatigue (C-SONG–HD fatigue) scale: a study of Chinese patients undergoing hemodialysis. Qual Life Res 33, 745–752 (2024). https://doi.org/10.1007/s11136-023-03561-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03561-4