Abstract
Purpose
To examine clinical outcomes and employment status in Veterans with and without a dual diagnosis of traumatic brain injury (TBI) and spinal cord injury (SCI).
Methods
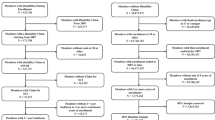
This cross-sectional study examined a national sample of Veterans enrolled in the VA Million Veteran Program who completed the Comprehensive TBI Evaluation (CTBIE) as part of the Veterans Health Administration’s TBI Screening and Evaluation Program. Veterans (N = 12,985) were classified into the following TBI/SCI groups using CTBIE data: those with a dual diagnosis of TBI and SCI (TBI+/SCI+); those with a history of TBI but no SCI (TBI+/SCI−); and those with no history of TBI or SCI (TBI−/SCI−; i.e., the control group). CTBIE-derived outcomes included neurobehavioral symptoms, comorbid psychiatric symptoms, pain and pain interference, and employment status.
Results
Chi-square analyses showed significant associations between TBI/SCI group and all clinical outcomes evaluated (all p’s < .001; V = 0.07–0.11). In general, the TBI+/SCI+ and TBI +/SCI− groups endorsed comparable levels of neurobehavioral symptoms, psychiatric symptoms, and pain, but significantly greater rates of symptoms and pain relative to the TBI−/SCI− group. Effect sizes for all pairwise comparisons were small (φ = 0.01–0.11). Finally, there was no significant association between TBI/SCI group and employment status (p = .170; V = 0.02), with all three groups showing relatively comparable rates of unemployment.
Conclusions
Regardless of SCI status, Veterans with TBI history endorsed poorer clinical outcomes than Veterans without TBI and SCI. However, rates of unemployment were similarly high across all three groups. Findings suggest that any Veteran completing the CTBIE may be at risk for poor clinical and employment outcomes.
Similar content being viewed by others
Data Availability
The data underlying this publication are accessible to researchers with Million Veteran Program (MVP) data access. MVP is currently only accessible to researchers who have a funded MVP project, either through a VA Merit Award or a VA Career Development Award. See https://www.research.va.gov/funding/Guidance-MVP-Data-Access-Merit-Award.pdf for more details.
References
(2021). VA/DoD Clinical Practice Guidelines for the Management of Concussion/Mild Traumatic Brain Injury (mTBI).
(2022). DoD TBI Worldwide Numbers.
Bernstock, J. D., Caples, C. M., Wagner, S. C., Kang, D. G., & Lehman, R. A., Jr. (2015). Characteristics of combat-related spine injuries: A review of recent literature. Military Medicine, 180(5), 503–512.
Creasey, G. H., Lateva, Z. C., Schüssler-Fiorenza Rose, S. M., & Rose, J. (2015). Traumatic brain injury in US veterans with traumatic spinal cord injury. Journal of Rehabilitation Research & Development, 52(6), 669–676.
Budd, M. A., Dixon, T. M., Barnett, S. D., Njoh, E., Goetz, L. L., & Ottomanelli, L. (2017). Examination of traumatic brain injury exposure among veterans with spinal cord injury. Rehabilitation Psychology, 62(3), 345–352.
Schwab, K., et al. (2017). Epidemiology and prognosis of mild traumatic brain injury in returning soldiers: A cohort study. Neurology, 88(16), 1571–1579.
Stein, M. B., et al. (2016). Prognostic indicators of persistent post-concussive symptoms after deployment-related mild traumatic brain injury: A prospective longitudinal study in US Army soldiers. Journal of Neurotrauma, 33(23), 2125–2132.
Cifu, D. X., et al. (2013). Traumatic brain injury, posttraumatic stress disorder, and pain diagnoses in OIF/OEF/OND veterans. Journal of Rehabilitation Research & Development, 50(9), 1169–1176.
Morissette, S. B., et al. (2011). Deployment-related TBI, persistent postconcussive symptoms, PTSD, and depression in OEF/OIF veterans. Rehabilitation Psychology, 56(4), 340–350.
Swan, A. A., et al. (2018). Long-term physical and mental health outcomes associated with traumatic brain injury severity in post-9/11 veterans: A retrospective cohort study. Brain Injury, 32(13–14), 1637–1650.
Clark, J. M., Jak, A. J., & Twamley, E. W. (2020). Cognition and functional capacity following traumatic brain injury in veterans. Rehabilitation Psychology, 65(1), 72–79.
Pogoda, T. K., et al. (2016). Associations between traumatic brain injury, suspected psychiatric conditions, and unemployment in operation enduring freedom/operation Iraqi freedom veterans. Journal of Head Trauma Rehabilitation, 31(3), 191–203.
Amick, M. M., Meterko, M., Fortier, C. B., Fonda, J. R., Milberg, W. P., & McGlinchey, R. E. (2018). The deployment trauma phenotype and employment status in veterans of the wars in Iraq and Afghanistan. The Journal of Head Trauma Rehabilitation, 33(2), E30–E40.
Putzke, J. D., Richards, J. S., Hicken, B. L., & DeVivo, M. J. (2002). Interference due to pain following spinal cord injury: Important predictors and impact on quality of life. Pain, 100(3), 231–242.
Watson, J. D., McDonald, S. D., Henry, R. S., Pugh, M., Jr., Kuzu, D., & Perrin, P. B. (2022). Pain, mental health, life satisfaction, and understanding from others in veterans with spinal cord injury. Rehabilitation Psychology, 67(3), 337–343.
Ullrich, P. M., et al. (2013). Pain and post-traumatic stress disorder symptoms during inpatient rehabilitation among operation enduring freedom/operation Iraqi freedom veterans with spinal cord injury. Archives of Physical Medicine and Rehabilitation, 94(1), 80–85.
McDonald, S. D., Mickens, M. N., Goldberg-Looney, L. D., Mutchler, B. J., Ellwood, M. S., & Castillo, T. A. (2018). Mental disorder prevalence among US Department of Veterans Affairs outpatients with spinal cord injuries. The Journal of Spinal Cord Medicine, 41(6), 691–702.
Saadat, S., et al. (2010). Health-related quality of life among individuals with long-standing spinal cord injury: A comparative study of veterans and non-veterans. BMC Public Health, 10(1), 1–7.
Ebrahimzadeh, M. H., Soltani-Moghaddas, S. H., Birjandinejad, A., Omidi-Kashani, F., & Bozorgnia, S. (2014). Quality of life among veterans with chronic spinal cord injury and related variables. Archives of Trauma Research, 3(2), e17917.
Meade, M. A., Barrett, K., Ellenbogen, P. S., & Jackson, M. N. (2006). Work intensity and variations in health and personal characteristics of individuals with spinal cord injury (SCI). Journal of Vocational Rehabilitation, 25(1), 13–19.
Goetz, L. L., Ottomanelli, L., Barnett, S. D., Sutton, B., & Njoh, E. (2018). Relationship between comorbidities and employment among veterans with spinal cord injury. Topics in Spinal Cord Injury Rehabilitation, 24(1), 44–53.
Rintala, D. H., Holmes, S. A., Fiess, R. N., Courtade, D., & Loubser, P. G. (2005). Prevalence and characteristics of chronic pain in veterans with spinal cord injury. Journal of Rehabilitation Research & Development, 42(5), 573–584.
Ottomanelli, L., & Lind, L. (2009). Review of critical factors related to employment after spinal cord injury: Implications for research and vocational services. The Journal of Spinal Cord Medicine, 32(5), 503–531.
Bradbury, C. L., et al. (2008). Traumatic brain injury in patients with traumatic spinal cord injury: Clinical and economic consequences. Archives of Physical Medicine and Rehabilitation, 89(12), S77–S84.
Macciocchi, S. N., Bowman, B., Coker, J., Apple, D., & Leslie, D. (2004). Effect of co-morbid traumatic brain injury on functional outcome of persons with spinal cord injuries. American Journal of Physical Medicine & Rehabilitation, 83(1), 22–26.
Mollayeva, T., Sutton, M., Escobar, M., Hurst, M., & Colantonio, A. (2021). The impact of a comorbid spinal cord injury on cognitive outcomes of male and female patients with traumatic brain injury. PM&R, 13(7), 683–694.
Reid, M. W., & Velez, C. S. (2015). Discriminating military and civilian traumatic brain injuries. Molecular and Cellular Neuroscience, 66, 123–128.
Armistead-Jehle, P., Soble, J. R., Cooper, D. B., & Belanger, H. G. (2017). Unique aspects of traumatic brain injury in military and veteran populations. Physical Medicine and Rehabilitation Clinics, 28(2), 323–337.
D. S. Loughran, Why is veteran unemployment so high? Washington, DC: RAND Corporation, 2014.
Trivedi, R. B., et al. (2015). Prevalence, comorbidity, and prognosis of mental health among US veterans. American Journal of Public Health, 105(12), 2564–2569.
Wallen, E. S., et al. (2023). Utilization of whole health services among veterans with spinal cord injuries and disorders (SCI/D): Early insights from the VA SCI/D system of care. The Journal of Spinal Cord Medicine. https://doi.org/10.1080/10790268.2023.2183325
Gaziano, J. M., et al. (2016). Million veteran program: A mega-biobank to study genetic influences on health and disease. Journal of Clinical Epidemiology, 70, 214–223.
(2007). Screening and evaluation of possible traumatic brain injury in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) Veterans.
(2010). Screening and Evaluation of Possible Traumatic Brain Injury in Operation Enduring Freedom (OEF) and Operation Iraqi Freedom (OIF) Veterans.
Vanderploeg, R. D., et al. (2014). Screening for postdeployment conditions: Development and cross-validation of an embedded validity scale in the neurobehavioral symptom inventory. The Journal of Head Trauma Rehabilitation, 29(1), 1–10.
Fihn, S. D., et al. (2014). Insights from advanced analytics at the Veterans Health Administration. Health Affairs, 33(7), 1203–1211.
Belanger, H. G., Vanderploeg, R. D., & Sayer, N. (2016). Screening for remote history of mild traumatic brain injury in VHA: A critical literature review. Journal of Head Trauma Rehabilitation, 31(3), 204–214.
Belanger, H. G., Vanderploeg, R. D., Soble, J. R., Richardson, M., & Groer, S. (2012). Validity of the Veterans Health Administration’s traumatic brain injury screen. Archives of Physical Medicine and Rehabilitation, 93(7), 1234–1239.
Donnelly, K. T., et al. (2011). Reliability, sensitivity, and specificity of the VA traumatic brain injury screening tool. The Journal of Head Trauma Rehabilitation, 26(6), 439–453.
Fortier, C. B., Amick, M. M., Kenna, A., Milberg, W. P., & McGlinchey, R. E. (2015). Correspondence of the Boston Assessment of Traumatic Brain Injury-Lifetime (BAT-L) clinical interview and the VA TBI screen. The Journal of Head Trauma Rehabilitation, 30(1), E1–E7.
Pape, T. L. B., et al. (2018). Diagnostic accuracy of the veteran affairs’ traumatic brain injury screen. Archives of Physical Medicine and Rehabilitation, 99(7), 1370–1382.
Radigan, L., McGlinchey, R. E., Milberg, W. P., & Fortier, C. B. (2018). Correspondence of the Boston Assessment of Traumatic Brain Injury-Lifetime (BAT-L) and the VA Comprehensive TBI Evaluation (CTBIE). The Journal of Head Trauma Rehabilitation, 33(5), E51–E55.
(2016). VA/DoD Clinical Practice Guidelines for the Management of Concussion/Mild Traumatic Brain Injury (mTBI).
Cicerone, K., & Kalmar, K. (1995). Persistent postconcussion syndrome: The structure of subjective complaints after mild traumatic brain injury. The Journal of Head Trauma Rehabilitation, 10(3), 1–17. https://doi.org/10.1097/00001199-199510030-00002
Soble, J. R., et al. (2014). Normative data for the Neurobehavioral Symptom Inventory (NSI) and post-concussion symptom profiles among TBI, PTSD, and nonclinical samples. The Clinical Neuropsychologist, 28(4), 614–632.
King, P. R., et al. (2012). Psychometric study of the neurobehavioral symptom inventory. Journal of Rehabilitation Research & Development, 49(6), 879–888.
Vanderploeg, R. D., et al. (2015). The structure of postconcussion symptoms on the Neurobehavioral Symptom Inventory: A comparison of alternative models, (in eng). Journal of Head Trauma Rehabilitation, 30(1), 1–11. https://doi.org/10.1097/HTR.0000000000000009
Meterko, M., Baker, E., Stolzmann, K. L., Hendricks, A. M., Cicerone, K. D., & Lew, H. L. (2012). Psychometric assessment of the neurobehavioral symptom inventory-22: The structure of persistent postconcussive symptoms following deployment-related mild traumatic brain injury among veterans. The Journal of Head Trauma Rehabilitation, 27(1), 55–62.
Silva, M. A. (2021). Review of the neurobehavioral symptom inventory. Rehabilitation Psychology, 66(2), 170–182.
Scholten, J. D., Sayer, N. A., Vanderploeg, R. D., Bidelspach, D. E., & Cifu, D. X. (2012). Analysis of US Veterans health administration comprehensive evaluations for traumatic brain injury in operation enduring freedom and operation Iraqi freedom veterans. Brain Injury, 26(10), 1177–1184.
Ozturk, E. D., Chanfreau-Coffinier, C., Sakamoto, M. S., Delano-Wood, L., & Merritt, V. C. (2022). Characterization of Million Veteran Program (MVP) enrollees with Comprehensive Traumatic Brain Injury Evaluation (CTBIE) data: An analysis of neurobehavioral symptoms. Journal of Psychiatric Research, 145, 230–242.
Smith-Seemiller, L., Fow, N. R., Kant, R., & Franzen, M. D. (2003). Presence of post-concussion syndrome symptoms in patients with chronic pain vs mild traumatic brain injury. Brain Injury, 17(3), 199–206.
Chan, R. C. (2001). Base rate of post-concussion symptoms among normal people and its neuropsychological correlates. Clinical Rehabilitation, 15(3), 266–273.
Iverson, G. L., & Lange, R. T. (2003). Examination of “postconcussion-like” symptoms in a healthy sample. Applied Neuropsychology, 10(3), 137–144.
Greer, N., et al. (2020). Prevalence and severity of psychiatric disorders and suicidal behavior in service members and veterans with and without traumatic brain injury: Systematic review. The Journal of Head Trauma Rehabilitation, 35(1), 1–13.
Banerjea, R., Findley, P., Smith, B., Findley, T., & Sambamoorthi, U. (2009). Co-occurring medical and mental illness and substance use disorders among veteran clinic users with spinal cord injury patients with complexities. Spinal Cord, 47(11), 789–795.
Findley, P. A., Banerjea, R., & Sambamoorthi, U. (2011). Excess mortality associated with mental illness and substance use disorders among veteran clinic users with spinal cord injury. Disability and Rehabilitation, 33(17–18), 1608–1615.
Brady, K. T., Tuerk, P., Back, S. E., Saladin, M. E., Waldrop, A. E., & Myrick, H. (2009). Combat posttraumatic stress disorder, substance use disorders, and traumatic brain injury. Journal of Addiction Medicine, 3(4), 179–188.
Carlson, K. F., Nelson, D., Orazem, R. J., Nugent, S., Cifu, D. X., & Sayer, N. A. (2010). Psychiatric diagnoses among Iraq and Afghanistan war veterans screened for deployment-related traumatic brain injury. Journal of Traumatic Stress, 23(1), 17–24.
Cooper, D. B., et al. (2015). Treatment of persistent post-concussive symptoms after mild traumatic brain injury: A systematic review of cognitive rehabilitation and behavioral health interventions in military service members and veterans. Brain Imaging and Behavior, 9(3), 403–420.
Venkatesan, U. M., & Ramanathan-Elion, D. M. (2022). Psychoeducation as precision health in military-related mild traumatic brain injury. Archives of Physical Medicine and Rehabilitation, 103(6), 1222–1232.
Whittaker, R., Kemp, S., & House, A. (2007). Illness perceptions and outcome in mild head injury: A longitudinal study. Journal of Neurology, Neurosurgery & Psychiatry, 78(6), 644–646.
Merritt, V. C., et al. (2020). Post-concussive symptom endorsement and symptom attribution following remote mild traumatic brain injury in combat-exposed Veterans: An exploratory study. Journal of Psychiatric Research, 130, 224–230.
Ottomanelli, L., Goetz, L. L., Barnett, S. D., Njoh, E., & Fishalow, J. (2022). Factors associated with past and current employment of veterans with spinal cord injury. The Journal of Spinal Cord Medicine, 45(1), 137–147.
Amara, J. H., Stolzmann, K. L., Iverson, K. M., & Pogoda, T. K. (2019). Predictors of employment status in male and female post-9/11 veterans evaluated for traumatic brain injury. The Journal of Head Trauma Rehabilitation, 34(1), 11–20.
Carlson, K. F., et al. (2018). Supported employment for veterans with traumatic brain injury: Patient perspectives. Archives of Physical Medicine and Rehabilitation, 99(2), S4-S13.e1.
Wyse, J. J., Pogoda, T. K., Mastarone, G. L., Gilbert, T., & Carlson, K. F. (2020). Employment and vocational rehabilitation experiences among veterans with polytrauma/traumatic brain injury history. Psychological Services, 17(1), 65.
Krist, A. H., South-Paul, J. E., & Meisnere, M. (2023). Achieving whole health for veterans and the nation: A National Academies of Sciences, Engineering, and Medicine report. JAMA Health Forum, 4(5), e230874.
Acknowledgements
The authors sincerely thank the Veterans who volunteered to participate in the Million Veteran Program. This research is based on data from the Million Veteran Program, Office of Research and Development, Veterans Health Administration, and was supported by award # IK2 CX001952. This publication does not represent the views of the Department of Veteran Affairs or the United States Government.
Funding
This work was supported by a Career Development Award awarded to Victoria C. Merritt from the VA Clinical Science Research & Development Service (IK2 CX001952).
Author information
Authors and Affiliations
Consortia
Contributions
All authors contributed to the study conception and design. Data curation and cleaning were performed by CC-C, and data analysis was performed by VM, in consultation with JC. The first draft of the manuscript was written by JC and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of the VA Central IRB.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Clark, J.M.R., Ozturk, E.D., Chanfreau-Coffinier, C. et al. Evaluation of clinical outcomes and employment status in veterans with dual diagnosis of traumatic brain injury and spinal cord injury. Qual Life Res 33, 229–239 (2024). https://doi.org/10.1007/s11136-023-03518-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-023-03518-7