Abstract
Purpose
To synthesize evidence on the impact of bronchopulmonary dysplasia (BPD) on the Quality of Life (QoL) of affected individuals from three perspectives: (i) QoL of caregiver; (ii) caregiver’s perception of BPD patient’s QoL; and (iii) BPD patient’s self-reported QoL.
Methods
Quantitative studies (case–control, cohort, and case series) on the QoL of BPD patients or their caregivers were considered. We conducted a systematic literature search of 6 databases (PubMed, Embase, World of Science, CINAHL, PsycINFO, and Chinese National Knowledge Infrastructure) for relevant studies. All databases were searched from the date of inception of the databases to 31 March 2022. Populations of interest were caregivers with preterm babies with BPD, or children/adults who were born premature and diagnosed with BPD. The main outcome measures were total and subdomain QoL scores, and factors affecting QoL.
Results
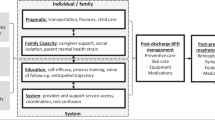
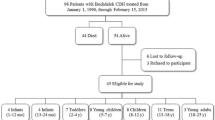
A total of 1078 articles were found; 10 were eligible for analysis, which included 247 caregivers and 1632 patients with BPD. The QoL of patients differed by domains—some were poorer or similar, but none of the QoL domains was better than QoL of healthy controls. Poor sleep and acute care needs of BPD patients negatively affected caregiver’s QoL, while increasing illness acuity negatively affected the QoL of BPD patients. The QoL of BPD patients and their caregivers was most adversely affected during the immediate post-discharge period and tended to improve with time. The physical QoL of BPD patients was similar to that of preterm babies without BPD when assessed during late childhood and early adulthood.
Conclusion
QoL assessment should be performed as an outcome measure and incorporated in the care plan for BPD patients and their caregivers.
Systematic Review Registration PROSPERO CRD42021292253.

Similar content being viewed by others
Data availability
Available upon reasonable request.
Code availability
Provided in Supplementary Information.
References
World Health Organisation (WHO). (2018). Preterm birth (Fact sheet). https://www.who.int/news-room/fact-sheets/detail/preterm-birth [Accessed 16 June 2022].
Thébaud, B., Goss, K. N., Laughon, M., Whitsett, J. A., Abman, S. H., Steinhorn, R. H., Aschner, J. L., Davis, P. G., McGrath-Morrow, S. A., Soll, R. F., & Jobe, A. H. (2019). Bronchopulmonary dysplasia. Nature Reviews Disease Primers, 5, 78. https://doi.org/10.1038/s41572-019-0127-7
Siffel, C., Kistler, K. D., Lewis, J. F. M., & Sarda, S. P. (2021). Global incidence of bronchopulmonary dysplasia among extremely preterm infants: A systematic literature review. The Journal of Maternal-Fetal & Neonatal Medicine, 34(11), 1721–1731. https://doi.org/10.1080/14767058.2019.1646240
Jobe, A. H., & Bancalari, E. (2001). Bronchopulmonary dysplasia. American Journal of Respiratory and Critical Care Medicine, 163(7), 1723–1729. https://doi.org/10.1164/ajrccm.163.7.2011060
Ehrenkranz, R.A., Walsh, M.C., Vohr, B.R., Jobe, A.H., Wright, L.L., Fanaroff, A.A., Wrage, L.A., Poole, K., National Institutes of Child Health and Human Development Neonatal Research Network. (2005). Validation of the national institutes of health consensus definition of bronchopulmonary dysplasia. Pediatrics, 116(6), 1353–1360. https://doi.org/10.1542/peds.2005-0249
World Health Organization (WHO). (1995). The World Health Organization Quality of Life assessment (WHOQOL): Position paper from the World Health Organization. Social Science & Medicine, 41(10), 1403–1409. https://doi.org/10.1016/0277-9536(95)00112-k
Revicki, D. A., Osoba, D., Fairclough, D., Barofsky, I., Berzon, R., Leidy, N. K., & Rothman, M. (2000). Recommendations on health-related quality of life research to support labeling and promotional claims in the United States. Quality of Life Research, 9(8), 887–900. https://doi.org/10.1023/a:1008996223999
Gellert, G. A. (1993). The importance of quality of life research for health care reform in the USA and the future of public health. Quality of Life Research, 2(5), 357–361. https://doi.org/10.1007/bf00449431
Gray, P. H., O’Callaghan, M. J., & Poulsen, L. (2008). Behaviour and quality of life at school age of children who had bronchopulmonary dysplasia. Early Human Development, 84(1), 1–8. https://doi.org/10.1016/j.earlhumdev.2007.01.009
Gough, A., Linden, M., Spence, D., Patterson, C. C., Halliday, H. L., & McGarvey, L. P. A. (2014). Impaired lung function and health status in adult survivors of bronchopulmonary dysplasia. European Respiratory Journal, 43(3), 808–816. https://doi.org/10.1183/09031936.00039513
McGrath-Morrow, S. A., Ryan, T., Riekert, K., Lefton-Greif, M. A., Eakin, M., & Collaco, J. M. (2013). The impact of bronchopulmonary dysplasia on caregiver health related quality of life during the first 2 years of life. Pediatric Pulmonology, 48(6), 579–586. https://doi.org/10.1002/ppul.22687
Bozzetto, S., Carraro, S., Tomasi, L., Berardi, M., Zanconato, S., & Baraldi, E. (2016). Health-related quality of life in adolescent survivors of bronchopulmonary dysplasia. Respirology, 21(6), 1113–1117. https://doi.org/10.1111/resp.12811
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., et al. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. https://doi.org/10.1136/bmj.n71
Harrison, H., Griffin, S. J., Kuhn, I., & Usher-Smith, J. A. (2020). Software tools to support title and abstract screening for systematic reviews in healthcare: An evaluation. BMC Medical Research Methodology, 20, 7. https://doi.org/10.1186/s12874-020-0897-3
The Ottawa Hospital Research Institute (OHRI). (2021). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. https://www.ohri.ca//programs/clinical_epidemiology/oxford.asp [Accessed 16 June 2022].
Feeley, C. A., Turner-Henson, A., Christian, B. J., Avis, K. T., Heaton, K., Lozano, D., & Su, X. (2014). Sleep quality, stress, caregiver burden, and quality of life in maternal caregivers of young children with bronchopulmonary dysplasia. Journal of Pediatric Nursing, 29(1), 29–38. https://doi.org/10.1016/j.pedn.2013.08.001
Sriram, S., Schreiber, M.D., Msall, M.E., Kuban, K.C.K., Joseph, R.M., O’Shea, T.M., Allred, E.N., Leviton, A., ELGAN Study Investigators. (2018). Cognitive development and quality of life associated with BPD in 10-year-olds born preterm. Pediatrics, 141(6), e20172719. https://doi.org/10.1542/peds.2017-2719
Brady, J. M., Zhang, H., Kirpalani, H., & DeMauro, S. B. (2019). Living with severe bronchopulmonary dysplasia-parental views of their child’s quality of life. The Journal of Pediatrics, 207, 117–122. https://doi.org/10.1016/j.jpeds.2018.10.001
Raat, H., Botterweck, A. M., Landgraf, J. M., Hoogeveen, W. C., & Essink-Bot, M. (2005). Reliability and validity of the short form of the child health questionnaire for parents (CHQ-PF28) in large random school based and general population samples. Journal of Epidemiology and Community Health, 59(1), 75–82. https://doi.org/10.1136/jech.2003.012914
Ronkainen, E., Kaukola, T., Marttila, R., Hallman, M., & Dunder, T. (2016). School-age children enjoyed good respiratory health and fewer allergies despite having lung disease after preterm birth. Acta Paediatrica, 105(11), 1298–1304. https://doi.org/10.1111/apa.13526
O’Shea, T. M., Allred, E. N., Dammann, O., Hirtz, D., Kuban, K. C. K., Paneth, N., Leviton, A., & ELGAN study investigators. (2009). The ELGAN study of the brain and related disorders in extremely low gestational age newborns. Early Human Development, 85(11), 719–725. https://doi.org/10.1016/j.earlhumdev.2009.08.060
Palta, M., & Sadek-Badawi, M. (2008). PedsQL relates to function and behavior in very low and normal birth weight 2- and 3-year-olds from a regional cohort. Quality of Life Research, 17(5), 691–700. https://doi.org/10.1007/s11136-008-9346-1
Varni, J. W., Limbers, C. A., Neighbors, K., Schulz, K., Lieu, J. E. C., Heffer, R. W., Tuzinkiewicz, K., Mangione-Smith, R., Zimmerman, J. J., & Alonso, E. M. (2011). The PedsQL™ Infant Scales: Feasibility, internal consistency reliability, and validity in healthy and ill infants. Quality of Life Research, 20(1), 45–55. https://doi.org/10.1007/s11136-010-9730-5
Beaudoin, S., Tremblay, G. M., Croitoru, D., Benedetti, A., & Landry, J. S. (2013). Healthcare utilization and health-related quality of life of adult survivors of preterm birth complicated by bronchopulmonary dysplasia. Acta Paediatrica, 102(6), 607–612. https://doi.org/10.1111/apa.12217
Pérez-Tarazona, S., Rueda Esteban, S., García-García, M. L., et al. (2021). Respiratory outcomes of “new” bronchopulmonary dysplasia in adolescents: A multicenter study. Pediatric Pulmonology, 56(5), 1205–1214. https://doi.org/10.1002/ppul.25226
Serra-Sutton, V., Ferrer, M., Rajmil, L., Tebé, C., Simeoni, M., & Ravens-Sieberer, U. (2009). Population norms and cut-off-points for suboptimal health related quality of life in two generic measures for adolescents: The Spanish VSP-A and KINDL-R. Health and Quality of Life Outcomes, 7, 35. https://doi.org/10.1186/1477-7525-7-35
Tugade, M. M., & Fredrickson, B. L. (2004). Resilient individuals use positive emotions to bounce back from negative emotional experiences. Journal of Personality and Social Psychology, 86(2), 320–333. https://doi.org/10.1037/0022-3514.86.2.320
Patrick, D. L., & Deyo, R. A. (1989). Generic and disease-specific measures in assessing health status and quality of life. Medical Care, 27(3), S217–S232. https://doi.org/10.1097/00005650-198903001-00018
Seow, L. S. E., Tan, T. H. G., Abdin, E., Chong, S. A., & Subramaniam, M. (2019). Comparing disease-specific and generic quality of life measures in patients with schizophrenia. Psychiatry Research, 273, 387–393. https://doi.org/10.1016/j.psychres.2019.01.034
de Vries, M., Ouwendijk, R., Kessels, A. G., de Haan, M. W., Flobbe, K., Hunink, M. G. M., et al. (2005). Comparison of generic and disease-specific questionnaires for the assessment of quality of life in patients with peripheral arterial disease. Journal of Vascular Surgery, 41(2), 261–268. https://doi.org/10.1016/j.jvs.2004.11.022
Meijer-Schaap, L., Dubois, A. E. J., Kollen, B. J., Tijmens-van der Hulst, J., Flokstra-de Blok, B. M. J., & Vrijlandt, E. J. L. E. (2019). Development and construct validation of a parent-proxy quality of life instrument in children with bronchopulmonary dysplasia aged 4–8 years old. Quality of Life Research, 28(2), 523–533. https://doi.org/10.1007/s11136-018-2029-7
Acknowledgements
We thank Ms Sheena Nishanti D/O Ramasamy for providing help with manuscript submission.
Funding
The authors declare that no funds, grants, or other support was received for the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Literature search, data extraction, and analysis were performed by Deborah M.X. Lee and Ashton K.S. Tan. The first draft of the manuscript was jointly written by Deborah M.X. Lee and Ashton K.S. Tan. All authors commented on previous versions of the manuscript and read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
As this was a review of existing literature, ethics approval was not required.
Consent to participate
Not applicable as the study did not involve any human subjects.
Consent to publish
Not applicable as the study did not involve any human subjects.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Lee, D.M.X., Tan, A.K.S., Ng, Y.P.M. et al. Quality of life of patients and caregivers affected by bronchopulmonary dysplasia: a systematic review. Qual Life Res 32, 1859–1869 (2023). https://doi.org/10.1007/s11136-022-03311-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-022-03311-y