Abstract
Purpose
Sleep disturbance is common in late life. While social interaction is a basic human concern, few studies have explored the linkage between interpersonal relationships and sleep disturbance. The present study examines the reciprocal associations between weak social networks outside the household and sleep disturbance in elderly, as well as the underlying mechanisms.
Methods
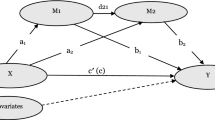
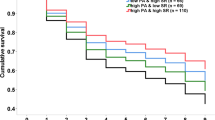
We utilized data from a nationally representative longitudinal survey of community-dwelling elderly in Singapore (n = 1417; ≥ 60 years). Participants were assessed three times over 6 years (2009, 2011, 2015). Measures included strength of social networks outside the household, restless sleep (sleep disturbance), and the mediating variables of depressed mood, chronic diseases, and cognitive impairment. A cross-lagged mediation analysis was conducted.
Results
Bootstrapping results showed that weaker social networks were related to more restless sleep via more depressed mood. Also, restless sleep was negatively associated with social networks through depressed mood. The other mediators examined were not significant.
Conclusions
Weak social networks and restless sleep reciprocally influence each other through depressed mood. Recognition of this interplay can inform efforts in improving elderly’s sleep quality, social networks, and psychological well-being.




Similar content being viewed by others
References
Bassett, E., & Moore, S. (2014). Neighbourhood disadvantage, network capital and restless sleep: Is the association moderated by gender in urban-dwelling adults? Social Science & Medicine, 108, 185–193.
Leggett, A., Burgard, S., & Zivin, K. (2016). The impact of sleep disturbance on the association between stressful life events and depressive symptoms. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(1), 118–128.
Smagula, S. F., Stone, K. L., Fabio, A., & Cauley, J. A. (2016). Risk factors for sleep disturbances in older adults: Evidence from prospective studies. Sleep Medicine Reviews, 25, 21–30.
Zhang, H.-S., Li, Y., Mo, H., Qiu, D.-X., Zhao, J., Luo, J.-L., et al. (2017). A community-based cross-sectional study of sleep quality in middle-aged and older adults. Quality of Life Research, 26(4), 923–933.
National Sleep Foundation. (2003). The 2003 sleep in America poll. Retrieved May 4, 2017, from https://sleepfoundation.org/sleep-polls-data/sleep-in-america-poll/2003-sleep-and-aging.
Baumeister, R. F., & Leary, M. R. (1995). The need to belong: Desire for interpersonal attachments as a fundamental human motivation. Psychological Bulletin, 117(3), 497–529.
Chen, J.-H., Waite, L. J., & Lauderdale, D. S. (2015). Marriage, relationship quality, and sleep among U.S. older adults. Journal of Health and Social Behavior, 56(3), 356–377.
Yang, H. C., Suh, S., Kim, H., Cho, E. R., Lee, S. K., & Shin, C. (2013). Testing bidirectional relationships between marital quality and sleep disturbances: A 4-year follow-up study in a Korean cohort. Journal of Psychosomatic Research, 74(5), 401–406.
Chan, A., Malhotra, C., Malhotra, R., & Ostbye, T. (2011). Living arrangements, social networks and depressive symptoms among older men and women in Singapore. International Journal of Geriatric Psychiatry, 26(6), 630–639.
Yao, K. W., Yu, S., Cheng, S. P., & Chen, I. J. (2008). Relationships between personal, depression and social network factors and sleep quality in community-dwelling older adults. Journal of Nursing Research, 16(2), 131–139.
Ailshire, J. A., & Burgard, S. A. (2012). Family relationships and troubled sleep among U.S. Adults: Examining the influences of contact frequency and relationship quality. Journal of Health and Social Behavior, 53(2), 248–262.
Baker, S., McBeth, J., Chew-Graham, C. A., & Wilkie, R. (2017). Musculoskeletal pain and co-morbid insomnia in adults: A population study of the prevalence and impact on restricted social participation. BMC Family Practice, 18(1), 17.
Troxel, W. M., Robles, T. F., Hall, M., & Buysse, D. J. (2007). Marital quality and the marital bed: Examining the covariation between relationship quality and sleep. Sleep Medicine Reviews, 11(5), 389–404.
Li, T., & Zhang, Y. (2015). Social network types and the health of older adults: Exploring reciprocal associations. Social Science & Medicine, 130, 59–68.
Bao, Y.-P., Han, Y., Ma, J., Wang, R.-J., Shi, L., Wang, T.-Y., et al. (2017). Cooccurrence and bidirectional prediction of sleep disturbances and depression in older adults: Meta-analysis and systematic review. Neuroscience & Biobehavioral Reviews, 75, 257–273.
Coyle, C. E., & Dugan, E. (2012). Social isolation, loneliness and health among older adults. Journal of Aging and Health, 24(8), 1346–1363.
Lemola, S., & Richter, D. (2013). The course of subjective sleep quality in middle and old adulthood and its relation to physical health. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68(5), 721–729.
Holtzman, R. E., Rebok, G. W., Saczynski, J. S., Kouzis, A. C., Wilcox Doyle, K., & Eaton, W. W. (2004). Social network characteristics and cognition in middle-aged and older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 59(6), P278-P284.
Hita-Yanez, E., Atienza, M., & Cantero, J. L. (2013). Polysomnographic and subjective sleep markers of mild cognitive impairment. Sleep, 36(9), 1327–1334.
Yaffe, K., Falvey, C. M., & Hoang, T. (2014). Connections between sleep and cognition in older adults. Lancet Neurology, 13(10), 1017–1028.
Pfeiffer, E. (1975). A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatrics Society, 23(10), 433–441.
MacCallum, R. C., Browne, M. W., & Sugawara, H. M. (1996). Power analysis and determination of sample size for covariance structure modeling. Psychological Methods, 1(2), 130–149.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2 ed.). Hillsdale, NJ: Lawrence Erlbaum Associates.
Lubben, J., & Gironda, M. (2004). Measuring social networks and assessing their benefits. In C. Phillipson, G. Allan, & D. Morgan (Eds.), Social networks and social exclusion: Sociological and policy perspectives (pp. 20–34). Burlington, VT: Ashgate.
Burgard, S. A., & Ailshire, J. A. (2009). Putting work to bed: Stressful experiences on the job and sleep quality. Journal of Health and Social Behavior, 50(4), 476–492.
Devins, G. M., Edworthy, S. M., Paul, L. C., Mandin, H., Seland, T. P., Klein, G., et al. (1993). Restless sleep, illness intrusiveness, and depressive symptoms in three chronic illness conditions: Rheumatoid arthritis, end-stage renal disease, and multiple sclerosis. Journal of Psychosomatic Research, 37(2), 163–170.
Kutner, N. G., Bliwise, D. L., Brogan, D., & Zhang, R. (2001). Race and restless sleep complaint in older chronic dialysis patients and nondialysis community controls. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 56(3), P170-P175.
Kohout, F. J., Berkman, L. F., Evans, D. A., & Cornoni-Huntley, J. (1993). Two shorter forms of the CES-D depression symptoms index. Journal of Aging and Health, 5(2), 179–193.
Malhotra, C., Chan, A., Matchar, D., Seow, D., Chuo, A., & Do, Y. K. (2013). Diagnostic performance of short portable mental status questionnaire for screening dementia among patients attending cognitive assessment clinics in Singapore. Annals of the Academy of Medicine, Singapore, 42(7), 315–319.
Lin, X., & Leung, K. (2010). Differing effects of coping strategies on mental health during prolonged unemployment: A longitudinal analysis. Human Relations, 63(5), 637–665.
Newsom, J. T. (2015). Longitudinal structural equation modeling: A comprehensive introduction. New York: Routledge.
Wang, J., & Wang, X. (2012). Structural equation modeling: Applications using Mplus. Chichester: Wiley.
Kline, R. B. (2016). Principles and practice of structural equation modeling (4 ed.). New York: The Guilford Press.
Geiser, C. (2013). Data analysis with Mplus. New York: The Guilford Press.
Kondratova, A. A., & Kondratov, R. V. (2012). The circadian clock and pathology of the ageing brain. Nature Reviews Neuroscience, 13(5), 325–335.
Buckley, T. M., & Schatzberg, A. F. (2005). Aging and the role of the HPA axis and rhythm in sleep and memory-consolidation. American Journal of Geriatric Psychiatry, 13(5), 344–352.
Belvederi Murri, M., Pariante, C., Mondelli, V., Masotti, M., Atti, A. R., Mellacqua, Z., et al. (2014). HPA axis and aging in depression: Systematic review and meta-analysis. Psychoneuroendocrinology, 41, 46–62.
Zetsche, U., D’Avanzato, C., & Joormann, J. (2012). Depression and rumination: Relation to components of inhibition. Cognition and Emotion, 26(4), 758–767.
Thomsen, D. K., Mehlsen, M. Y., Hokland, M., Viidik, A., Olesen, F., Avlund, K., et al. (2004). Negative thoughts and health: Associations among rumination, immunity, and health care utilization in a young and elderly sample. Psychosomatic Medicine, 66(3), 363–371.
Thomsen, D. K., Yung Mehlsen, M., Christensen, S., & Zachariae, R. (2003). Rumination—relationship with negative mood and sleep quality. Personality and Individual Differences, 34(7), 1293–1301.
Wong, J. Y.-H., Fong, D. Y.-T., & Chan, K. K.-W. (2015). Anxiety and insomnia as modifiable risk factors for somatic symptoms in Chinese: A general population-based study. Quality of Life Research, 24(10), 2493–2498.
Sadler, P., McLaren, S., & Jenkins, M. (2013). A psychological pathway from insomnia to depression among older adults. International Psychogeriatrics, 25(8), 1375–1383.
Riva, P., & Eck, J. (Eds.). (2016). Social exclusion: Psychological approaches to understanding and reducing its impact. Cham: Springer.
Yang, P. Y., Ho, K. H., Chen, H. C., & Chien, M. Y. (2012). Exercise training improves sleep quality in middle-aged and older adults with sleep problems: A systematic review. Journal of Physiotherapy, 58(3), 157–163.
Quan, S. F., Katz, R., Olson, J., Bonekat, W., Enright, P. L., Young, T., et al. (2005). Factors associated with incidence and persistence of symptoms of disturbed sleep in an elderly cohort: The Cardiovascular Health Study. American Journal of the Medical Sciences, 329(4), 163–172.
Zimmerman, M. E., Bigal, M. E., Katz, M. J., Derby, C. A., & Lipton, R. B. (2013). Are sleep onset/maintenance difficulties associated with medical or psychiatric comorbidities in nondemented community-dwelling older adults? Journal of Clinical Sleep Medicine, 9(4), 363–369.
Buysse, D. J., Reynolds, C. F. III, Monk, T. H., Berman, S. R., & Kupfer, D. J. (1989). The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Research, 28(2), 193–213.
Acknowledgements
This research was supported by Singapore Ministry of Social and Family Development; Singapore Ministry of Health’s National Medical Research Council under its Singapore Translational Research Investigator Award as part of the project “Establishing a Practical and Theoretical Foundation for Comprehensive and Integrated Community, Policy and Academic Efforts to Improve Dementia Care in Singapore” (NMRC-STAR-0005-2009), and its Clinician Scientist - Individual Research Grant—New Investigator Grant (NMRC-CNIG-1124-2014); Duke-NUS Geriatric Research Fund. We thank Irene Teo and Rebecca Lau for their comments on the draft of this paper.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Data collection/analysis was approved by the Institutional Review Board at National University of Singapore. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Cheng, G.HL., Malhotra, R., Chan, A. et al. Weak social networks and restless sleep interrelate through depressed mood among elderly. Qual Life Res 27, 2517–2524 (2018). https://doi.org/10.1007/s11136-018-1895-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-018-1895-3