Abstract
Purpose
Validity is a contextual aspect of a scale which may differ across sample populations and study protocols. The objective of our study was to validate the Care-Related Quality of Life Instrument (CarerQol) across two different study design features, sampling framework (general population vs. different care settings) and survey mode (interview vs. written questionnaire).
Methods
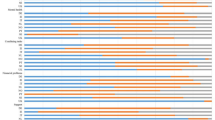
Data were extracted from The Older Persons and Informal Caregivers Minimum DataSet (TOPICS-MDS, www.topics-mds.eu), a pooled public-access data set with information on >3,000 informal caregivers throughout the Netherlands. Meta-correlations and linear mixed models between the CarerQol’s seven dimensions (CarerQol-7D) and caregiver’s level of happiness (CarerQol-VAS) and self-rated burden (SRB) were performed.
Results
The CarerQol-7D dimensions were correlated to the CarerQol-VAS and SRB in the pooled data set and the subgroups. The strength of correlations between CarerQol-7D dimensions and SRB was weaker among caregivers who were interviewed versus those who completed a written questionnaire. The directionality of associations between the CarerQol-VAS, SRB and the CarerQol-7D dimensions in the multivariate model supported the construct validity of the CarerQol in the pooled population. Significant interaction terms were observed in several dimensions of the CarerQol-7D across sampling frame and survey mode, suggesting meaningful differences in reporting levels.
Conclusions
Although good scientific practice emphasises the importance of re-evaluating instrument properties in individual research studies, our findings support the validity and applicability of the CarerQol instrument in a variety of settings. Due to minor differential reporting, pooling CarerQol data collected using mixed administration modes should be interpreted with caution; for TOPICS-MDS, meta-analytic techniques may be warranted.


Similar content being viewed by others
References
Robine, J. M., Michel, J. P., & Herrmann, F. R. (2007). Who will care for the oldest people in our ageing society? BMJ, 334(7593), 570–571.
Agree, E. M., & Glaser, K. (2009). Demography of informal caregiving. In P. Uhlenberg (Ed.), International handbook of population aging (pp. 647–668). Netherlands: Springer.
Ward, B. W., & Schiller, J. S. (2013). Prevalence of multiple chronic conditions among US adults: Estimates from the National Health Interview Survey, 2010. Preventing Chronic Disease, 10, E65.
Caughey, G. E., Vitry, A. I., Gilbert, A. L., & Roughead, E. E. (2008). Prevalence of comorbidity of chronic diseases in Australia. BMC Public Health, 8, 221.
Uijen, A. A., & van de Lisdonk, E. H. (2008). Multimorbidity in primary care: Prevalence and trend over the last 20 years. European Journal of General Practice, 14(Suppl 1), 28–32.
Bevans, M., & Sternberg, E. M. (2012). Caregiving burden, stress, and health effects among family caregivers of adult cancer patients. JAMA, 307(4), 398–403.
Schulz, R., & Beach, S. R. (1999). Caregiving as a risk factor for mortality: The Caregiver Health Effects Study. JAMA, 282(23), 2215–2219.
Joling, K. J., van Hout, H. P., Schellevis, F. G., van der Horst, H. E., Scheltens, P., Knol, D. L., et al. (2010). Incidence of depression and anxiety in the spouses of patients with dementia: A naturalistic cohort study of recorded morbidity with a 6-year follow-up. The American Journal of Geriatric Psychiatry, 18(2), 146–153.
Bobinac, A., van Exel, N. J., Rutten, F. F., & Brouwer, W. B. (2011). Health effects in significant others: Separating family and care-giving effects. Medical Decision Making, 31(2), 292–298.
Mestheneos, E., & Triantafillou, J. (Eds.). (2005). Supporting family carers of older people in Europe: The Pan-European background report. Empirical evidence, policy trends and future perspectives. Hamburg: Lit Verlag.
Lutomski, J. E., Baars, M. A., Schalk, B. W., Boter, H., Buurman, B. M., den Elzen, W. P., et al. (2013). The development of the older persons and informal caregivers survey minimum dataset (TOPICS-MDS): A large-scale data sharing initiative. PLoS ONE, 8(12), e81673.
Martin, P., & Lynn, P. (2011). The effects of mixed mode survey designs on simple and complex analyses. Centre for comparative social surveys working paper series: Paper no. 04: Centre for comparative social surveys, City University London.
Hood, K., Robling, M., Ingledew, D., Gillespie, D., Greene, G., Ivins, R., et al. (2012). Mode of data elicitation, acquisition and response to surveys: A systematic review. Health Technology Assessment, 16(27), 1–162.
Groves, R. M., & Peytcheva, E. (2008). The impact of nonresponse rates on nonresponse bias: A meta-analysis. Public Opinion Quarterly, 72(2), 167–189.
Streiner, D. L., & Norman, G. R. (2008). Health measure scales: A pratical guide to their development and use (4th ed., pp. 167–210). Oxford University Press: New York.; 247–276.
Hoefman, R. J., van Exel, N. J., Foets, M., & Brouwer, W. B. (2011). Sustained informal care: The feasibility, construct validity and test–retest reliability of the CarerQol-instrument to measure the impact of informal care in long-term care. Aging & Mental Health, 15(8), 1018–1027.
Hoefman, R. J., van Exel, N. J., Looren de Jong, S., Redekop, W. K., & Brouwer, W. B. (2011). A new test of the construct validity of the CarerQol instrument: Measuring the impact of informal care giving. Quality of Life Research, 20(6), 875–887.
Brouwer, W. B., van Exel, N. J., van Gorp, B., & Redekop, W. K. (2006). The CarerQol instrument: A new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Quality of Life Research, 15(6), 1005–1021.
Hoefman, R. J., van Exel, J., Rose, J. M., van de Wetering, E. J., & Brouwer, W. B. (2014). A discrete choice experiment to obtain a tariff for valuing informal care situations measured with the CarerQol instrument. Medical Decision Making, 34(1), 84–96.
Hoefman, R. J., van Exel, J., & Brouwer, W. (2013). How to include informal care in economic evaluations. Pharmacoeconomics, 31(12), 1105–1119.
van Exel, N. J., Scholte op Reimer, W. J., Brouwer, W. B., van den Berg, B., Koopmanschap, M. A., & van den Bos, G. A. (2004). Instruments for assessing the burden of informal caregiving for stroke patients in clinical practice: A comparison of CSI, CRA, SCQ and self-rated burden. Clinical Rehabilitation, 18(2), 203–214.
Brouwer, W. B., van Exel, N. J., van den Berg, B., van den Bos, G. A., & Koopmanschap, M. A. (2005). Process utility from providing informal care: The benefit of caring. Health Policy, 74(1), 85–99.
Searle, S. D., Mitnitski, A., Gahbauer, E. A., Gill, T. M., & Rockwood, K. (2008). A standard procedure for creating a frailty index. BMC Geriatrics, 8, 24.
Lutomski, J. E., Baars, M. A., van Kempen, J. A., Buurman, B. M., den Elzen, W. P., Jansen, A. P., et al. (2013). Validation of a frailty index from the older persons and informal caregivers survey minimum data set. Journal of the American Geriatrics Society, 61(9), 1625–1627.
Terwee, C. B., Bot, S. D., de Boer, M. R., van der Windt, D. A., Knol, D. L., Dekker, J., et al. (2007). Quality criteria were proposed for measurement properties of health status questionnaires. Journal of Clinical Epidemiology, 60(1), 34–42.
Mokkink, L. B., Terwee, C. B., Patrick, D. L., Alonso, J., Stratford, P. W., Knol, D. L., et al. (2010). The COSMIN study reached international consensus on taxonomy, terminology, and definitions of measurement properties for health-related patient-reported outcomes. Journal of Clinical Epidemiology, 63(7), 737–745.
Schwarzer, G. (2013). meta: Meta-analysis with R. http://cran.r-project.org/web/packages/meta/meta.pdf. Version = 3.1-2.
Hopkins, W. G. (2002). A new view of statistics: Effect magnitudes. Retrieved from http://www.sportsci.org/resource/stats/effectmag.html on 27 February 2014.
Singer, J. D. (1998). Using SAS PROC MIXED to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics, 23(4), 323–355.
De Leeuw, E. D. (2005). To mix or not to mix data collection modes in surveys. Journal of Official Statistics, 21, 233–255.
van Praag, B. M. S., Frijters, P., & Ferrer-i-Carbonell, A. (2003). The anatomy of subjective well-being. Journal of Economic Behavior & Organization, 51, 29–49.
Bobinac, A., van Exel, N. J. A., Rutten, F. F. H., & Brouwer, W. B. F. (2010). Caring for and caring about: Disentangling the caregiver effect and the family effect. Journal of Health Economics, 29, 549–556.
van den Berg, B., & Ferrer-i-Carbonell, A. (2007). Monetary valuation of informal care: The well-being valuation method. Health Economics, 16, 1227–1244.
Hoefman, R. J., Van Exel, N. J. A., & Brouwer, W. B. F. (2011) iMTA Valuation of Informal Care Questionnaire (iVICQ). Version 1.0 (December 2011). Rotterdam: iBMG/iMTA, 2011. Retrieved from www.bmg.eur.nl/english/imta/publications/manuals_questionnaires/ on 25 September 2013.
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., & Group, P. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ, 339, b2535.
Higgins, J. P. T., & Green, S. (eds) (2009). Cochrane handbook for systematic reviews of interventions version 5.0.2 [updated September 2009]. The Cochrane Collaboration, 2009. www.cochrane-handbook.org.
Riley, R. D., Lambert, P. C., & Abo-Zaid, G. (2010). Meta-analysis of individual participant data: Rationale, conduct, and reporting. BMJ, 340, c221.
Boulton, G., Rawlins, M., Vallance, P., & Walport, M. (2011). Science as a public enterprise: The case for open data. Lancet, 377(9778), 1633–1635.
Riley, R. D. (2010). Commentary: Like it and lump it? Meta-analysis using individual participant data. International Journal of Epidemiology, 39(5), 1359–1361.
Ahmed, I., Sutton, A. J., & Riley, R. D. (2012). Assessment of publication bias, selection bias, and unavailable data in meta-analyses using individual participant data: A database survey. BMJ, 344, d7762.
Acknowledgments
The authors thank TOPICS-MDS Consortium members for their contribution to this research. The National Care for the Elderly Programme on behalf of the Organisation of Health Research and Development (ZonMw—The Netherlands). TOPICS-MDS Consortium: Project Group W.P.J. den Elzen (Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, Netherlands); A.P.D. Jansen (Department of General Practice and Elderly Care Medicine/EMGO + Institute for Health and Care Research, VU University Medical Center, Amsterdam, Netherlands); G.I.J.M. Kempen (CAPHRI School for Public Health and Primary Care, Department of Health Services Research, Maastricht University, Netherlands), P.F.M. Krabbe (Department of Epidemiology, University of Groningen, University Medical Center Groningen, Netherlands); R.J.F. Melis (Department of Geriatric Medicine, Radboud University Medical Center, Nijmegen, Netherlands); E.P. Moll van Charante (Department of General Medicine, Academic Medical Center, Amsterdam, Netherlands); B. Steunenberg (Julius Center for Health Sciences and Primary Care, UMC Utrecht, Netherlands); E.W. Steyerberg (Department of Public Health, Erasmus MC University Medical Center, Rotterdam, Netherlands); Steering Committee E. Buskens (Department of Epidemiology, University of Groningen, University Medical Center, Groningen, Netherlands), J. Gussekloo (Department of Public Health and Primary Care, Leiden University Medical Center, Leiden, Netherlands); H.E. van der Horst (Department of General Practice and Elderly Care Medicine, EMGO Institute for Health and Care Research, VU University Medical Centre Amsterdam, Netherlands); M.G.M. Olde-Rikkert, (Department of Geriatric Medicine, Radboud University Medical Center, Nijmegen, Netherlands); S.E.J.A. de Rooij (Department of Internal Medicine, Academic Medical Center, Amsterdam, Netherlands); J.M.G.A. Schols (Department of Family Medicine and Department of Health Services Research, CAPHRI School for Public Health and Primary Care, Maastricht University, Maastricht, Netherlands); M.J. Schuurmans (Department of Rehabilitation, Nursing Science and Sports, University Medical Center Utrecht, Netherlands); D. Smilde (Department of Research Policy, Erasmus MC University Medical Centre, Rotterdam, Netherlands); R.G.J. Westendorp (Leyden Academy on Vitality and Ageing, Leiden University Medical Center); Working group D. van den Brink, J.E. Lutomski, L. Qin (Department of Geriatric Medicine, Radboud University Medical Center, Nijmegen, Netherlands).
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of TOPICS-MDS Consortium.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Lutomski, J.E., van Exel, N.J.A., Kempen, G.I.J.M. et al. Validation of the Care-Related Quality of Life Instrument in different study settings: findings from The Older Persons and Informal Caregivers Survey Minimum DataSet (TOPICS-MDS). Qual Life Res 24, 1281–1293 (2015). https://doi.org/10.1007/s11136-014-0841-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11136-014-0841-2