Abstract
Postural instability is a feature that is frequently observed in patients with psychotic disorders. Previous studies applied rating scales or behavioral test to assess postural instabilities. Recently, a pressure-sensitive platform has been used to study detailed characteristics of postural sway and regulation. However, characteristics of posturography indices in patients with psychotic disorders have not been well documented. To integrate the findings from studies that assessed postural sway using posturography in patients with psychotic disorders, we conducted a systematic review. Following database literature search, we identified nine eligible articles. Assessment conditions and indices of postural stability varied between studies. Postural control was associated with negative and general psychopathology in two studies. Two studies reported associations between posturographic variables and medication dose, whereas four studies reported no associations. This review identified the need to develop standards to assess postural sway in patients with psychiatric disorders. Further studies need to report associations between postural sway and confounding factors.

Similar content being viewed by others
References
Green MF, Kern RS, Braff DL, Mintz J. Neurocognitive deficits and functional outcome in schizophrenia: Are we measuring the “right stuff”? Schizophrenia Bulletin 26(1):119–36, 2000.
Leifker FR, Bowie CR, Harvey PD. Determinants of everyday outcomes in schizophrenia: The influences of cognitive impairment, functional capacity, and symptoms. Schizophrenia Research 115(1):82–7, 2009.
Mohamed S, Rosenheck R, Swartz M, Stroup S, Lieberman JA, Keefe RS. Relationship of cognition and psychopathology to functional impairment in schizophrenia. The American Journal of Psychiatry 165(8):978–87, 2008.
Bas TO, Poyraz CA, Bas A, Poyraz BC, Tosun M. The impact of cognitive impairment, neurological soft signs and subdepressive symptoms on functional outcome in bipolar disorder. Journal of Affective Disorders 174C:336–41, 2015.
Bora E, Pantelis C. Meta-analysis of cognitive impairment in first-episode bipolar disorder: Comparison with first-episode schizophrenia and healthy controls. Schizophrenia Bulletin 2015. doi:10.1093/schbul/sbu198.
Keefe RS, Malhotra AK, Meltzer HY, et al. Efficacy and safety of donepezil in patients with schizophrenia or schizoaffective disorder: Significant placebo/practice effects in a 12-week, randomized, double-blind, placebo-controlled trial. Neuropsychopharmacology 33(6):1217–28, 2008.
Biswas P, Malhotra S, Malhotra A, Gupta N. Comparative study of neurological soft signs in schizophrenia with onset in childhood, adolescence and adulthood. Acta Psychiatrica Scandinavica 115(4):295–303, 2007.
Chan RC, Xu T, Heinrichs RW, Yu Y, Wang Y. Neurological soft signs in schizophrenia: A meta-analysis. Schizophrenia Bulletin 36(6):1089–104, 2010.
Dazzan P, Morgan KD, Orr KG, et al. The structural brain correlates of neurological soft signs in AESOP first-episode psychoses study. Brain 127(Pt 1):143–53, 2004.
Jahn T, Hubmann W, Karr M, et al. Motoric neurological soft signs and psychopathological symptoms in schizophrenic psychoses. Psychiatry Research 142(2–3):191–9, 2006.
Keshavan MS, Sanders RD, Sweeney JA, et al. Diagnostic specificity and neuroanatomical validity of neurological abnormalities in first-episode psychoses. The American Journal of Psychiatry 160(7):1298–304, 2003.
Sevincok L, Akoglu A, Topaloglu B, Aslantas H. Neurological soft signs in schizophrenic patients with obsessive-compulsive disorder. The Journal of neuropsychiatry and clinical neurosciences 58(3):274–9, 2004.
Varambally S, Venkatasubramanian G, Thirthalli J, Janakiramaiah N, Gangadhar BN. Cerebellar and other neurological soft signs in antipsychotic-naive schizophrenia. Acta Psychiatrica Scandinavica 114(5):352–6, 2006.
Zhao Q, Ma YT, Lui SS, et al. Neurological soft signs discriminate schizophrenia from major depression but not bipolar disorder. Progress in Neuro-Psychopharmacology and Biological Psychiatry 43:72–8, 2013.
Marvel CL, Schwartz BL, Rosse RB. A quantitative measure of postural sway deficits in schizophrenia. Schizophrenia Research 68(2-3):363–72, 2004.
Sullivan EV, Rose J, Pfefferbaum A. Mechanisms of postural control in alcoholic men and women: Biomechanical analysis of musculoskeletal coordination during quiet standing. Alcoholism: clinical and experimental research 34(3):528–37, 2010.
Braus DF, Weber-Fahr W, Tost H, Ruf M, Henn FA. Sensory information processing in neuroleptic-naive first-episode schizophrenic patients: A functional magnetic resonance imaging study. Archives of General Psychiatry 59(8):696–701, 2002.
Calhoun VD, Sui J, Kiehl K, Turner J, Allen E, Pearlson G. Exploring the psychosis functional connectome: aberrant intrinsic networks in schizophrenia and bipolar disorder. Frontiers in Psychiatry 2:75, 2012.
Jacobsen LK, Giedd JN, Berquin PC, et al. Quantitative morphology of the cerebellum and fourth ventricle in childhood-onset schizophrenia. American Journal of Psychiatry 154(12):1663–9, 1997.
Prasad KM, Patel AR, Muddasani S, Sweeney J, Keshavan MS. The entorhinal cortex in first-episode psychotic disorders: A structural magnetic resonance imaging study. American Journal of Psychiatry 161(9):1612–9, 2004.
Levitt JJ, McCarley RW, Nestor PG, et al. Quantitative volumetric MRI study of the cerebellum and vermis in schizophrenia: Clinical and cognitive correlates. American Journal of Psychiatry 156(7):1105–7, 1999.
Picard H, Amado I, Mouchet-Mages S, Olie JP, Krebs MO. The role of the cerebellum in schizophrenia: An update of clinical, cognitive, and functional evidences. Schizophrenia Bulletin 34(1):155–72, 2008.
Ho BC, Mola C, Andreasen NC. Cerebellar dysfunction in neuroleptic naive schizophrenia patients: Clinical, cognitive, and neuroanatomic correlates of cerebellar neurologic signs. Biological Psychiatry 55(12):1146–53, 2004.
Horak FB, Shupert CL, Mirka A. Components of postural dyscontrol in the elderly: A review. Neurobiology of Aging ;10(6):727–38, 1989.
Mancini M, Horak FB. The relevance of clinical balance assessment tools to differentiate balance deficits. European Journal of Physical and Rehabilitation Medicine 46(2):239–48, 2010.
Chaudhry H, Bukiet B, Ji Z, Findley T. Measurement of balance in computer posturography: Comparison of methods–A brief review. Journal of Bodywork and Movement Therapies 15(1):82–91, 2011.
Era P, Sainio P, Koskinen S, Haavisto P, Vaara M, Aromaa A. Postural balance in a random sample of 7,979 subjects aged 30 years and over. Gerontology 52(4):204–13, 2006.
Nardone A, Grasso M, Schieppati M. Balance control in peripheral neuropathy: Are patients equally unstable under static and dynamic conditions? Gait & posture 23(3):364–73, 2006.
Piirtola M, Era P. Force platform measurements as predictors of falls among older people - a review. Gerontology 52(1):1–16, 2006.
de Haart M, Geurts AC, Huidekoper SC, Fasotti L, van Limbeek J. Recovery of standing balance in postacute stroke patients: A rehabilitation cohort study. Archives of Physical Medicine and Rehabilitation 85(6):8869–5, 2004.
Mandarakas M, Hiller CE, Rose KJ, Burns J. Measuring ankle instability in pediatric Charcot-Marie-Tooth disease. Journal of Child Neurology 28(11):1456–62, 2013.
Snapp-Childs W, Mon-Williams M, Bingham GP. A sensorimotor approach to the training of manual actions in children with developmental coordination disorder. Journal of Child Neurology 28(2):204–12, 2013.
Sullivan EV, Rosenbloom MJ, Pfefferbaum A. Balance and gait deficits in schizophrenia compounded by the comorbidity of alcoholism. American Journal of Psychiatry 161(4):751–5, 2004.
Ahlgren-Rimpilainen A, Lauerma H, Kahkonen S, et al. Effect of visual information on postural control in patients with schizophrenia. The Journal of Nervous and Mental Disease 198(8):601–3, 2010.
Bernard JA, Dean DJ, Kent JS, et al. Cerebellar networks in individuals at ultra high-risk of psychosis: Impact on postural sway and symptom severity. Human Brain Mapping 35(8):4064–78, 2014.
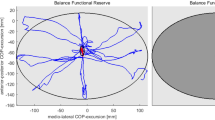
Bolbecker AR, Hong SL, Kent JS, Klaunig MJ, O’Donnell BF, Hetrick WP. Postural control in bipolar disorder: Increased sway area and decreased dynamical complexity. PLoS One 6(5):e19824, 2011.
Dean DJ, Kent JS, Bernard JA, et al. Increased postural sway predicts negative symptom progression in youth at ultrahigh risk for psychosis. Schizophrenia Research 162(1–3):86–9, 2015.
Ikai S, Uchida H, Suzuki T, Tsunoda K, Mimura M, Fujii Y. Effects of yoga therapy on postural stability in patients with schizophrenia-spectrum disorders: A single-blind randomized controlled trial. Journal of Psychiatric Research 47(11):1744–50, 2013.
Kent JS, Hong SL, Bolbecker AR, et al. Motor deficits in schizophrenia quantified by nonlinear analysis of postural sway. PLoS One 7(8):e41808, 2012.
Koreki A, Tsunoda K, Suzuki T, et al. Clinical and demographic characteristics associated with postural instability in patients with schizophrenia. Journal of Clinical Psychopharmacology 31(1):16–21, 2011.
Stensdotter AK, Loras HW, Flovig JC, Djupsjobacka M. Postural control in quiet standing in patients with psychotic disorders. Gait & Posture 38(4):918–22, 2013.
Stensdotter AK, Wanvik AK, Loras HW. Postural control in quiet standing with a concurrent cognitive task in psychotic conditions. Journal of Motor Behavior 45(4):279–87, 2013.
Kayser J, Tenke CE, Kroppmann CJ, et al. A neurophysiological deficit in early visual processing in schizophrenia patients with auditory hallucinations. Psychophysiology 49(9):1168–78, 2012.
Perez VB, Shafer KM, Cadenhead KS. Visual information processing dysfunction across the developmental course of early psychosis. Psychological Medicine 42(10):2167–79, 2012.
Asslander L, Peterka RJ. Sensory reweighting dynamics in human postural control. Journal of Neurophysiology 111(9):1852–64, 2014.
Wada M, Sunaga N, Nagai M. Anxiety affects the postural sway of the antero-posterior axis in college students. Neuroscience Letters 302(2–3):157–9, 2001.
Le Clair K, Riach C. Postural stability measures: what to measure and for how long. Clin Biomech (Bristol, Avon) . 11(3):176–8, 1996.
King DJ, Wilson A, Cooper SJ, Waddington JL. The clinical correlates of neurological soft signs in chronic schizophrenia. The British Journal of Psychiatry 158:770–5, 1991.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 339:b2535, 2009.
Fujino H, Sumiyoshi C, Sumiyoshi T, et al. Performance on the Wechsler Adult Intelligence Scale-III in Japanese patients with schizophrenia. Psychiatry and Clinical Neurosciences 68(7):534–41, 2014.
Keefe RS, Bilder RM, Harvey PD, et al. Baseline neurocognitive deficits in the CATIE schizophrenia trial. Neuropsychopharmacology 31(9):2033–46, 2006.
Lysaker PH, Whitney KA, Davis LW. Awareness of illness in schizophrenia: Associations with multiple assessments of executive function. The Journal of Neuropsychiatry and Clinical Neurosciences 18(4):516–20, 2006.
Inada T, Inagaki A. Psychotropic dose equivalence in Japan. Psychiatry and Clinical Neurosciences 2015. doi:10.1111/pcn.12275.
Casey DE. Implications of the CATIE trial on treatment: Extrapyramidal symptoms. CNS Spectrums 11(7 Suppl 7):25–31, 2006.
Tandon R, Jibson MD. Extrapyramidal side effects of antipsychotic treatment: Scope of problem and impact on outcome. Annals of Clinical Psychiatry 14(2):123–9, 2002.
Kasparek T, Rehulova J, Kerkovsky M, Sprlakova A, Mechl M, Mikl M. Cortico-cerebellar functional connectivity and sequencing of movements in schizophrenia. BMC Psychiatry 12:17, 2012.
Laidi C, d’Albis MA, Wessa M, et al. Cerebellar volume in schizophrenia and bipolar I disorder with and without psychotic features. Acta Psychiatrica Scandinavica 131(3):223–33, 2015.
O’Halloran CJ, Kinsella GJ, Storey E. The cerebellum and neuropsychological functioning: A critical review. Journal of Clinical and Experimental Neuropsychology 34(1):35–56, 2012.
Szeszko PR, Gunning-Dixon F, Goldman RS, et al. Lack of normal association between cerebellar volume and neuropsychological functions in first-episode schizophrenia. American Journal of Psychiatry 160(10):1884–7, 2003.
Bernard JA, Mittal VA. Cerebellar-motor dysfunction in schizophrenia and psychosis-risk: The importance of regional cerebellar analysis approaches. Frontiers in Psychiatry 5:160, 2014.
Farb NA, Anderson AK, Mayberg H, Bean J, McKeon D, Segal ZV. Minding one’s emotions: Mindfulness training alters the neural expression of sadness. Emotion 10(1):25–33, 2010.
Fernros L, Furhoff AK, Wandell PE. Improving quality of life using compound mind-body therapies: Evaluation of a course intervention with body movement and breath therapy, guided imagery, chakra experiencing and mindfulness meditation. Quality of Life Research 17(3):367–76, 2008.
Fujino H. Effects of Dohsa-hou relaxation on body awareness and psychological distress. Japanese Psychological Research 54(4):388–99, 2012.
Fujino H. Subjective experience of Dohsa-hou relaxation: A qualitative study. Asia Pacific Journal of Counselling and Psychotherapy 4(1):66–75, 2013.
Schieppati M, Tacchini E, Nardone A, Tarantola J, Corna S. Subjective perception of body sway. Journal of Neurology, Neurosurgery & Psychiatry 66(3):313–22, 1999.
Acknowledgments
This study was supported in part by research grants from JSPS KAKENHI (Grant Number: 26860924) and the Program for Creating Future Wisdom at Osaka University selected in 2014. No additional external funding was received for this study. The funders had no role in the study design, data collection and analyses, decision to publish, or preparation of the manuscript.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fujino, H., Imura, O. Postural Sway and Clinical Characteristics in Patients with Psychotic Disorders: A Review. Psychiatr Q 86, 603–614 (2015). https://doi.org/10.1007/s11126-015-9355-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11126-015-9355-5