Abstract
This supplemental issue describes the individual studies and collaborative efforts of the Helping to End Addiction Long-term Prevention Cooperative’s (HPC’s) innovative approaches to rapidly develop evidence-based prevention programs for widespread dissemination. This introduction succinctly reviews (1) the context that demands the rapid development of efficacious prevention programs and their scale-ups, (2) the unique objectives of the individual HPC research projects, and (3) collective efforts to harmonize research across studies to advance the prevention of opioid misuse and gain insight into opioid misuse etiology to inform improvements in preventive interventions. At the conclusion of HPC studies, we anticipate the availability of multiple evidence-based programs to prevent opioid misuse and use disorder for persons who experience particular sources of risk and for delivery in settings where prevention has traditionally been lacking. By harmonizing and coordinating efforts across 10 distinct outcomes studies of prevention programs and making data available for analysis by non-HPC researchers, the HPC’s efficacy and etiology evidence will far surpass the additive contributions of 10 individual research projects.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
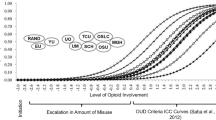
This supplemental issue presents the multidisciplinary strategies being used to rapidly develop prevention interventions to help curb the ongoing epidemics of opioid misuse, opioid use disorder (OUD), and drug use overdose. Until recently, most efforts to curb these epidemics have concentrated on policing, treatment, and harm reduction (e.g., preventing overdose deaths) because of how rapidly and powerfully opioid misuse can lead to OUD and cause both medical and mental health deterioration (Ridenour et al., 2006; Sartor et al., 2014). However, despite advances in each of these areas (Hoffman et al., 2019), the prevalence of opioid misuse has steadily increased since 1999, with an additional ongoing surge in synthetic opioid use that began in 2014 (Mattson et al., 2021). Further adding to the threat of overdose death from illicit drug use is the recent widespread contamination of the illicit drug supply with synthetic opioids and benzodiazepine analogs (Ciccarone, 2021; O'Donnell et al., 2021).
In recent years of the opioid epidemic, adolescents and young adults have been disproportionately impacted by opioid misuse and overdose deaths (Friedman et al., 2022; Hudgins et al., 2019). Adolescent overdose deaths increased by 94% from 2019 to 2020, followed by an additional increase of 20% from 2020 to 2021. Fentanyl played a large part in this trend (e.g., 77% of the 1146 adolescent overdose deaths in 2021 involved fentanyl). Overdose deaths and opioid misuse are more prevalent in subpopulations who experience greater social and structural risks, many of which include large numbers of adolescents and young adults. Individuals in these subpopulations are included in the over 30 million patients who have been prescribed legal opioids (Hudgins et al., 2019), millions of youth and adults involved with the legal system (Kluckow & Zeng, 2022), members of historically marginalized groups (Cano, 2021; Qeadan et al., 2021), the over 500,000 people experiencing homelessness (National Alliance to End Homelessness, 2022), and the over one in five U.S. citizens (over 52 million) who experience a mental health disorder per year (Substance Abuse and Mental Health Services Administration (SAMHSA), 2021). In addition to addressing social and structural barriers, the need to develop strength-based programs to bolster resilience against opioid misuse is especially great among these groups (Bonar et al., 2020).
HEAL Prevention Cooperative
To speed up scientific solutions to the opioid public health crisis, the National Institutes of Health (NIH) funded the Helping to End Addiction Long-term (HEAL) Initiative (National Institutes of Health, 2022). Recognizing the importance of prevention in addressing the opioid public health crisis, NIH funded the Preventing Opioid Use Disorder Research Program (Preventing OUD) as part of the NIH HEAL Initiative in 2019 (National Institutes of Health (NIH), 2022). As discussed by Goldstein, Oudekerk, and Blanco (this issue), Preventing OUD is a growing program of research focused on risk identification, development of preventative interventions, social determinants and policies impacting health equity, and implementation and scale-up of effective services all aiming to understand and prevent opioid misuse and use disorder. This supplemental issue describes one component of preventing OUD, the Preventing Opioid Use Disorder in Older Adolescents and Young Adults Cooperative, referred to as the HEAL Prevention Cooperative or HPC (HEAL Prevention Cooperative (HPC), 2021).
The HPC includes 10 research projects supported by a coordinating center, nine of which are funded through cooperative agreement awards administered by the National Institute on Drug Abuse (NIDA). The HPC aims to develop and test a diverse set of preventative interventions while simultaneously preparing the interventions found to be effective for rapid dissemination and implementation. The HPC interventions are being tested among older adolescents and young adults aged 15 to 30, given the well-documented increases in opioid misuse rates in individuals during the transition into young adulthood (Hudgins et al., 2019) and the dearth of interventions shown to prevent opioid misuse among young people. As a set, the 10 interventions are being designed for delivery within or in partnership with a variety of service systems that reach young people who experience risk for opioid misuse, including social services (e.g., child welfare, self-sufficiency, housing), the legal system, and health care systems (e.g., behavioral health, emergency department, school-based health center). In addition, two interventions are designed for and being tested within American Indian/Alaska Native communities.
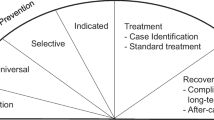
Ultimately, this initiative is positioned to develop evidence-based interventions that increase the likelihood of reaching young people with diverse risk profiles, leading to reduced opioid-related risks and improving overall health among populations that are often under-resourced and underrepresented in prevention. As further discussed in Cance et al. (this issue), the interventions all include a key focus on prevention, but provide a range of services from health promotion to treatment along the continuum of care. The recent trajectory of the opioid crisis makes clear the urgent need for effective interventions to be implemented and scaled across the nation. To bridge the known gap between research and translating findings into practice, the HPC is working to develop and disseminate similar information about each intervention, including the intervention costs, economic outcomes, and implementation experiences. This information will be important for policymakers and practitioners deciding whether to adopt the program. The innovative strategy to summarize implementation approaches and considerations for comparison across HPC interventions is discussed in Patel (this issue).
HEAL Prevention Cooperative Outcomes Studies
The articles in this supplemental issue integrate knowledge across the 10 HPC research projects on a variety of topics key to advancing the prevention field. The 10 studies are unique in many ways, including the research designs, targeted groups (those who experience greater risk), interventions and programs, and delivery settings. Even among the subsets of the 10 HPC studies that are designed for similar contexts, some are highly comparable whereas others are largely distinct. A strength of the diversity of HPC studies is that–relative to cooperative studies with a single design and intervention–they can better address the assortment of real-world needs for a variety of interventions across community systems, as well as the diverse challenges that need to be met to prevent opioid misuse, OUD, and drug overdoses. One of the noted limitations to coordinating such distinct studies is that there are challenges and relatively few opportunities to harmonize across them, which are discussed later.
Legal Systems
Youth involved in the legal system (YILS) are more likely to engage in substance use generally, and opioid misuse specifically, compared with the general youth population (Jones et al., 2020; Vaughn et al., 2012). However, given the many challenges associated with implementing programs within settings such as juvenile detention centers, much work is needed to develop evidence-based prevention programs (Ahrens et al., under review). Two HPC research projects are implementing and evaluating innovative programming to increase connections between YILS and caring adults throughout the reentry transition from residential facilities to the community.
Researchers at Texas Christian University (PI: Danica Knight) implemented the Leveraging Safe Adults (LeSA) project, a hybrid type 1 effectiveness-implementation design testing the effectiveness of Trust-Based Relational Intervention® (TBRI) with with a randomized control trial component in which youth-caregiver dyads being assigned to one of 3 in-home support conditions (Knight et al., 2021). A delayed-start design is being used so that each facility serves as its own control group to estimate TBRI efficacy. Using tenets from attachment theory, this trauma-informed prevention intervention targeted individual, interpersonal, and organizational/agency risk and protective factors associated with opioid misuse and OUD among youth.
The Positive Outcomes through Supported Transition (POST) study (MPIs: Kym Ahrens, Seattle Children’s Hospital; Kevin Haggerty, University of Washington) is using a Sequential Multiple Assignment Randomized Trial (SMART) design to test the effectiveness of an intervention based on the Adolescent Community Reinforcement Approach with Assertive Continuing Care (ACRA-ACC). Similar to the LeSA project, POST targets multiple levels of influence–including individual, interpersonal, organizational, and community factors–for post-adjudicated youth at risk for developing an OUD. Youth are first randomized between two conditions with higher or lower intensity, delivered pre- and post release. One month after release, all youth are assessed and some are re-randomized, depending on self-reports of current problematic substance use.
Social Services
Prevention efforts targeting OUD require multidisciplinary approaches, many of which occur in community-based settings and need to address social determinants of health; however, there is limited research addressing prevention efforts in social service settings (Fraser & Plescia, 2019). To address this gap, three HPC research projects are evaluating preventive interventions that are delivered within or through referrals from agencies that serve young families or individuals. Within these studies, efforts to address opioid misuse ranged from targeting young adults aged 18 to 24 experiencing homelessness (The Ohio State University; Kelleher and Slesnick, MPIs), rural young parents or guardians aged 18 to 30 with a history of substance use disorders (SUDs) and opioid misuse (University of Oregon; Stormshak, PI) and young parents aged 16 to 30 involved with child welfare or self-sufficiency services (Oregon Social Learning Center, Saldana, PI). These preventive interventions represent creative approaches to lowering the risk of some of the most under-resourced parents in late adolescence/young adulthood.
The Ohio State University Housing Opportunities, Motivation, and Engagement project developed a comprehensive program that connects young adults experiencing homelessness with independent housing and opioid and other substance use prevention services. Housing assistance and prevention services are delivered by advocates, are strengths-based, attend to potential mental health conditions that are known to exacerbate risk for opioid misuse in this population, and address a critical need in broader health care provision–how to address social determinants of health.
Two studies recognize the interplay among substance use, mental health, parenting needs, and social determinants that impact health and parenting outcomes in young adults. The University of Oregon team adapted the well-established evidence-based Family-Checkup program (Stormshak et al., 2019) specifically for under-resourced young parents with a child under age 5. This intervention is designed to reduce risk behavior, enhance parenting skills, and prevent the onset of substance use. Their adaptation includes developing an online platform and telehealth approach to reach individuals in remote and rural areas, attending to the limited prevention and intervention services in proximity to these areas. There are also specific modules in the adaptation, which include increasing safety in the home, responsible substance use while parenting, and conflict management.
The Oregon Social Learning Center team targeted young parents involved with child welfare or self-sufficiency recruited to participate in the Families Actively Improving Relationships for Prevention (PRE-FAIR) program. PRE-FAIR is an adaptation of FAIR (Saldana et al., 2021) that uses a community-based model to combine evidence-based techniques that target four key treatment components: parental substance use, maladaptive parenting, mental health symptoms, and contextual problems such as housing and employment. Families receive PRE-FAIR services in their natural environments (e.g., home, school, court) and receive incentives related to healthy households for meeting individualized treatment goals. This project develops, tests, and implements PRE-FAIR to prevent the onset and escalation of opioid misuse and methamphetamine use in young parents referred by child welfare or self-sufficiency services. As part of this project, researchers are using a hybrid implementation focus to assess the feasibility of large-scale implementation while testing the clinical effectiveness of an evidence-based program adapted for prevention. This provides the opportunity to test what is necessary under real-world condition to implement the PRE-FAIR preventive intervention.
Health Care
Many health care services are provided to individuals who experience risk for opioids misuse, including treatment for pain or mental health conditions. Three health care system-based HPC projects focus respectively on reducing risk in ED patients who are at risk for opioid misuse/OUD, screening for OUD/SUD in behavioral health clinics, and offering a prevention intervention in school-based health centers. Due to the challenges in transitioning youth from pediatric to primary care, the ED serves as a regularly location to provide services to youth and young adults who experience greater risk of opioid misuse. The University of Michigan team (MPIs: Walton and Bonar) developed interventions to be delivered to ED patients that integrate motivational interviewing (Miller & Rollnick, 2013) and cognitive behavioral therapy (Waldron & Kaminer, 2004) to prevent misusing opioids or OUD for young people aged 16 to 30. In addition, they utilize health coaches who deliver tailored supportive messages via a portal-like platform to participants.
Due to the prevalence of mental health comorbidities, and that youth and young adults with mental health conditions experience greater risk of OUD, screening for mental health and SUD and coordinating care is a priority among many of the HPC projects (Yule et al., this issue). The Massachusetts General Hospital (MPI: Wilens) and Boston Medical Center (MPI: Yule) project is focused on screening and monitoring mental health symptoms and substance use, and examining the impact of treating psychopathology on later risk for developing an OUD. To improve systematic screening for substance use they have implemented validated patient-reported outcome measures (PROMs) in their electronic health record system to screen and monitor for OUD/SUD, anxiety, and depression as part of routine outpatient clinical care across several behavioral health clinics. They are also following patients longitudinally who are seen in these clinics between the ages of 16 and 30 years to examine the impact of treating psychopathology on the later risk for OUD/SUD. They are using a combination of self-report measures including PROMs collected during treatment and information from the electronic health record such as health service utilization (e.g., ED visits, medication prescriptions, billing diagnoses, number of behavioral health visits and type) to examine this research question. The goal of this project is to highlight how a more streamlined approach to screening and treatment may help identify and overcome challenges with opioid or other substance misuse in individuals who are experiencing early-onset mental health symptoms.
Building on their considerable work in creating and evaluating digital games targeting adolescent health outcomes (Fiellin et al., 2017), the play2PREVENT Lab (p2P) at the Yale Center for Health & Learning Games (PI: Fiellin) developed PlaySmart, a videogame intervention, to prevent the initiation of opioid misuse and promote mental health among adolescents aged 16 to 19. Their randomized controlled trial is evaluating PlaySmart’s impact on the perception of great risk of harm from opioid misuse as the primary outcome in 532 adolescents in over 10 school-based health programs. Given the increased access and engagement with videogames, this work has considerable potential for greater implementation, reach, and impact on adolescents inside schools and elsewhere.
American Indian/Alaska Native
American Indian/Alaska Native (AI/AN) communities have been disproportionately impacted by the opioid crisis compared to other racial and ethnic groups, despite having similar rates of use (Center for Behavioral Health Statistics and Quality, 2021). Two HPC research projects are testing strategies to prevent OUD among AI/AN youth and young adults (Komro, this issue) by respectively increasing social connection and indigenous cultural values.
Researchers at Emory University (PI: Komro) partnered with Cherokee Nation Behavioral Health (CNBH) to implement a multilevel (community- and school-level) intervention targeting older adolescents (aged 15 to 20) residing in rural areas in or near the Cherokee Nation. High schools were randomized to receive connect, a school-based intervention. One component of connect is universal computer-based screening and brief intervention using motivational interviewing techniques with follow-up sessions conducted by outside coaches hired by CNBH. Caregivers of students receive Family Action Kits to promote positive parenting and social support, and communities Communities Mobilizing for Change and Action (CMCA), a community organization intervention.
In partnership with the Sacred Path Indigenous Wellness Center, researchers at RAND Corporation (MPI: D’Amico) and UCLA (MPI: Dickerson) developed Traditions and Connections for Urban Native Americans (TACUNA) to prevent OUD among AI/AN emerging adults aged 18 to 25 and living in urban areas. This virtual intervention includes three workshops that combine prevention programming, cultural activities (e.g., Native American cooking, prayer, and the four sacred medicines), and discussions about the attributes of participants’ social networks, focusing on both risk and protective factors within the network.
Coordination and Harmonization across HEAL Prevention Cooperative
Coordinating Center objectives include gathering and disseminating insights into the HPC approach to accelerate the process of testing interventions through to the scale-up stage; facilitate cross-disciplinary learning and research for improved problem-solving of unforeseen study challenges (e.g., participant recruitment during COVID-19 surges); compare regional trends in the study populations; and coordinate cross-study data analyses and research dissemination. As described by Ridenour et al. (this issue), Coordinating Center staff facilitated the HPC prospective harmonization of a subset of measures collected across HPC studies and created supporting documentation. Ultimately, HPC data will be deposited into the National Addiction and HIV Data Archive Program (National Addiction & HIV Data Archive Program (NAHDAP)) (National Addiction & HIV Data Archive Program (NAHDAP), n.d.), allowing other scientists’ access for secondary data analysis. Additional Coordinating Center activities are guided by the following aims:
-
facilitate coordination and communication across the HPC, including the conduct and dissemination of systematic reviews and other scholarly works;
-
provide implementation science consultation and facilitate implementation research;
-
establish data infrastructure;
-
provide data harmonization and methodological consultation and lead and facilitate cross-project investigations on etiology and prevention of opioid misuse and OUD; and
-
support economic evaluation across research projects.
This intentional cross-study engagement requires committee and workgroup involvement aimed at supporting the research projects in specific methodological, implementation science, cost, and dissemination aims. The Coordinating Center organizes these activities, provides support to, and engages with research project teams to allow their efforts to focus on testing prevention programs.
HEAL Prevention Cooperative Research Harmonization
Harmonizing research efforts among the HPC studies focused on outcome measures, economic analyses, and implementation research. At minimum, collecting the same data and doing so in the same manner among HPC studies facilitates comparisons among them. Although outcomes data harmonization expands the research that can be conducted using HPC data, economic and implementation research inform adoption and applied uses of the HPC programs.
No two HPC interventions targeted the same mechanisms of change. Indeed, their original proposals were to measure their single common outcome–opioid misuse–in 10 different ways. Ridenour et al. (this issue) describe the process and statistical strategies being used in the HPC to prospectively harmonize outcomes measures and data. This represents a rare opportunity to harmonize data prospectively among such distinct studies; to date, harmonization efforts have largely consisted of retrospective efforts to secondarily analyze preexisting datasets. Long after HPC studies are completed, their data may be useful for opioid misuse and OUD etiology and prevention research. The harmonized measures across HPC studies increase the statistical power and expand the research questions that can be addressed far beyond what is possible with any individual HPC study. This unique prospective harmonization approach can guide future research as we move toward open science (Lochman, 2022).
Costs to start up and maintain a new program weigh heavily into administrator decisions about whether and which program to adopt. To support the adoption of the HPC programs in new locales, the HPC economic evaluation will yield each research project’s startup costs and ongoing intervention delivery costs, collected prospectively using an activity-based costing approach (Dunlap et al., this issue). In turn, the results will provide economic data to inform substance use prevention, including investments required to deliver a range of programs. The HPC budget impact analysis will estimate the broad economic impact of HPC interventions for several years following the intervention.
Research on HPC program implementation will provide information to assist their adoption elsewhere (Patel et al., this issue). In addition to cost considerations, understanding the key aspects of how a study aligns with real-world settings in which it may be adopted can lead to more effective implementation of a novel program. To this end, the HPC implementation research strategy is designed to garner a study’s setting-specific and implementation strategies, participants and their study contributions, stakeholder engagement, which original features can (not) be adapted for other locations, and elements of the study implementation that differ from applied implementation.
Conclusion
Cooperative efforts among multiple research projects have significant value for the rapid development of evidence-based prevention programs in response to the opioid epidemic. To illustrate, when facing challenges while conducting a study (e.g., lulls in recruitment, having to pivot in research design due to COVID-19 social restrictions), members of one research project have been able to draw from the expertise and experience of researchers in nine other research projects. Conducting clinical trials and other outcomes studies requires considerable effort from many team members that restrict the extent to which additional evaluation can be layered on top of the outcomes research. The addition of a coordinating center supported HPC research projects in multiple ways including cross-project measurement harmonization, community learning on challenges that occur during a study or other topics chosen by research team members, supporting economics evaluations, collecting implementation data, and disseminating cross-project findings. As mentioned earlier and detailed in other papers of this issue, we anticipate that having commensurate evidence from multiple research projects will yield far greater insights into prevention program impacts and etiology of opioid misuse and use disorder than any single research project could generate. To capitalize on the harmonized data even further, HPC data are planned to be accessible through the National Addiction and HIV Data Archive Program (National Addiction & HIV Data Archive Program (NAHDAP)) (National Addiction & HIV Data Archive Program (NAHDAP), n.d.). In turn, the innovative research and data collected by the HPC should contribute to the prevention and etiology research of opioid misuse and OUD long after the studies are completed.
References
Bonar, E. E., Coughlin, L., Roche, J. S., Philyaw-Kotov, M. L., Bixler, E. A., Sinelnikov, S., & Walton, M. A. (2020). Prescription opioid misuse among adolescents and emerging adults in the United States: A scoping review. Preventive Medicine, 132, 105972. https://doi.org/10.1016/j.ypmed.2019.105972
Cano, M. (2021). Racial/ethnic differences in US drug overdose mortality, 2017–2018. Addictive Behaviours, 112, 106625. https://doi.org/10.1016/j.addbeh.2020.106625
Center for Behavioral Health Statistics and Quality. (2021). Racial/ethnic differences in substance use, substance use disorders, and substance use treatment utilization among people aged 12 or older (2015-2019). (Publication No. PEP21-07-01-001). Substance Abuse and Mental Health Services Administration. Retrieved February 2, 2023, from https://www.samhsa.gov/data/sites/default/files/reports/rpt35326/2021NSDUHSUChartbook.pdf
Ciccarone, D. (2021). The rise of illicit fentanyls, stimulants and the fourth wave of the opioid overdose crisis. Current Opinion in Psychiatry, 34(4), 344–350. https://doi.org/10.1097/YCO.0000000000000717
HEAL Prevention Cooperative (HPC). (2021). HPC profiles. National Institutes of Health. Retrieved January 10 2022, from, https://heal.nih.gov/files/2021-12/NIH_HEAL_Profiles_11%20%282%29%20%281%29.pdf
Fiellin, L. E., Hieftje, K. D., Pendergrass, T. M., Kyriakides, T. C., Duncan, L. R., Dziura, J. D., ... & Fiellin, D. A. (2017). Video game intervention for sexual risk reduction in minority adolescents: randomized controlled trial. Journal of medical Internet research, 19(9), e314.
Fraser, M., & Plescia, M. (2019). The opioid epidemic’s prevention problem. American Journal of Public Health, 109(2), 215–217. https://doi.org/10.2105/AJPH.2018.304859
Friedman, J., Godvin, M., Shover, C. L., Gone, J. P., Hansen, H., & Schriger, D. L. (2022). Trends in drug overdose deaths among US adolescents, January 2010 to June 2021. JAMA, 327(14), 1398–1400. https://doi.org/10.1001/jama.2022.2847
Hoffman, K. A., Ponce Terashima, J., & McCarty, D. (2019). Opioid use disorder and treatment: Challenges and opportunities. BMC Health Services Research, 19, 1–5.
Hudgins, J. D., Porter, J. J., Monuteaux, M. C., & Bourgeois, F. T. (2019). Prescription opioid use and misuse among adolescents and young adults in the United States: A national survey study. PLoS Medicine, 16(11), e1002922. https://doi.org/10.1371/journal.pmed.1002922
Jones, C. M., Clayton, H. B., Deputy, N. P., Roehler, D. R., Ko, J. Y., Esser, M. B., Brookmeyer, K. A., & Feldman Hertz, M. (2020). Prescription opioid misuse and use of alcohol and other substances among high school students – Youth Risk Behavior Survey, United States, 2019. MMWR, 69(1), 38–46. https://doi.org/10.15585/mmwr.su6901a5
Kluckow, R., & Zeng, Z. (2022). Correctional populations in the United States, 2020 – Statistical tables. https://bjs.ojp.gov/library/publications/correctional-populations-united-states-2020-statistical-tables
Knight, D. K., Yang, Y., Joseph, E. D., Tinius, E., Young, S., Shelley, L. T., Cross, D. R., & Knight, K. (2021). Preventing opioid use among justice-involved youth as they transition to adulthood: leveraging safe adults (LeSA). BMC Public Health, 21(1), 2133. https://doi.org/10.1186/s12889-021-12127-3
Lochman, J. E. (2022). Open science and intervention research: A program developer’s and researcher’s perspective on issues and concerns. Prevention Science, 23(5), 844–851. https://doi.org/10.1007/s11121-021-01219-6
Mattson, C. L., Tanz, L. J., Quinn, K., Kariisa, M., Patel, P., & Davis, N. L. (2021). Trends and geographic patterns in drug and synthetic opioid overdose deaths - United States, 2013–2019. MMWR Morbility and Mortality Weekly Report, 70(6), 202–207. https://doi.org/10.15585/mmwr.mm7006a4
Miller, W. R., & Rollnick, S. (2013). Motivational interviewing: Helping people change (3rd ed.). Guilford Press.
National Addiction & HIV Data Archive Program (NAHDAP). (n.d.). Retrieved November 30, 2022, from https://www.icpsr.umich.edu/web/pages/NAHDAP/index.html
National Alliance to End Homelessness. (2022). State of homelessness: 2022 Edition. https://endhomelessness.org/homelessness-in-america/homelessness-statistics/state-of-homelessness/
National Institutes of Health, HEAL Initiative. (2022). About. Retrieved November 30 from, https://heal.nih.gov/about
National Institutes of Health (NIH). (2022). Preventing opioid use disorder. U.S. Department of Health and Human Services. Retrieved January 10 from, https://heal.nih.gov/research/new-strategies/preventing-opioid-use-disorder
O'Donnell, J., Tanz, L. J., Gladden, R. M., Davis, N. L., & Bitting, J. (2021). Trends in and characteristics of drug overdose deaths involving illicitly manufactured fentanyls - United States, 2019–2020. MMWR Morbility and Mortality Weekly Report, 70(50), 1740–1746. https://doi.org/10.15585/mmwr.mm7050e3
Qeadan, F., Madden, E. F., Bern, R., Parsinejad, N., Porucznik, C. A., Venner, K. L., & English, K. (2021). Associations between opioid misuse and social relationship factors among American Indian, Alaska Native, and Native Hawaiian college students in the US. Drug and Alcohol Dependence, 222, 108667.
Ridenour, T. A., Lanza, S. T., Donny, E. C., & Clark, D. B. (2006). Different lengths of times for progressions in adolescent substance involvement. Addictive Behaviors, 31(6), 962–983. https://doi.org/10.1016/j.addbeh.2006.03.015
Saldana, L., Chapman, J. E., Campbell, M., Alley, Z., Schaper, H., & Padgett, C. (2021). Meeting the needs of families involved in the child welfare system for parental substance abuse: Outcomes from an effectiveness trial of the Families Actively Improving Relationships Program. Frontiers in Psychology, 12, Article 689483. https://doi.org/10.3389/FPSYG.2021.689483
Sartor, C. E., Kranzler, H. R., & Gelernter, J. (2014). Rate of progression from first use to dependence on cocaine or opioids: A cross-substance examination of associated demographic, psychiatric, and childhood risk factors. Addictive Behaviors, 39(2), 473–479. https://doi.org/10.1016/j.addbeh.2013.10.021
Stormshak, E., Seeley, J. R., Caruthers, A. S., Cardenas, L., Moore, K. J., Tyler, M. S., Fleming, C. M., Gau, J., & Danaher, B. (2019). Evaluating the efficacy of the family check-up online: A school-based, eHealth model for the prevention of problem behavior during the middle school years. Development and Psychopathology, 31(5), 1873–1886. https://doi.org/10.1017/s0954579419000907
Substance Abuse and Mental Health Services Administration (SAMHSA). (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health. NSDUH Series H-56. HHS Publication No. PEP21–07–01–003. Center for behavioral health statistics and quality, substance abuse and mental health services administration. Retrieved November 30, 2022, from https://www.samhsa.gov/data/
Vaughn, M. G., Fu, Q., Perron, B. E., & Wu, L. T. (2012). Risk profiles among adolescent nonmedical opioid users in the United States. Addictive Behaviors, 37(8), 974–977. https://doi.org/10.1016/j.addbeh.2012.03.015
Waldron, H. B., & Kaminer, Y. (2004). On the learning curve: The emerging evidence supporting cognitive-behavioral therapies for adolescent substance abuse. Addiction, 99(Suppl 2), 93–105. https://doi.org/10.1111/j.1360-0443.2004.00857.x
Funding
This research was supported by the National Institutes of Health through the NIH HEAL Initiative as part of the HEAL Preventing Opioid Use Disorder Research Program. The authors gratefully acknowledge the collaborative contributions of the National Institute on Drug Abuse (NIDA) and support from the following awards: RTI International (U24DA050182; MPIs Phillip Graham, Ty Ridenour) and Yale University (UH3DA050251; PI Lynn Fiellin).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
All studies that are described or referenced herein have been reviewed and approved by the Investigators’ respective Institutional Review Boards. All procedures with human subjects were performed in accordance with the ethical standards of the institute and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to Participate
Not applicable.
Conflict of Interest
The authors declare that they have no conflict of interest.
Disclaimer
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or its NIH HEAL Preventing Opioid Use Disorder Research Program. Dr. Barbara Oudekerk was substantially involved in U24DA050182, consistent with her role as Scientific Officer for the coordination center. She had no substantial involvement in the other cited grants.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ridenour, T.A., Saavedra, L.M., Fernandes, CS.F. et al. Introduction to Helping to End Addiction Long-Term Prevention Cooperative: Overview and Strategies. Prev Sci 24 (Suppl 1), 1–7 (2023). https://doi.org/10.1007/s11121-023-01503-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11121-023-01503-7