Abstract
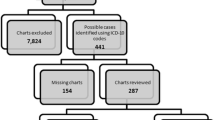
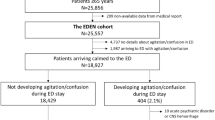
Background Although delirium is one of the most common adverse drug reactions observed in hospitalized older people, it remains underdiagnosed. Aim To estimate the prevalence of hospitalization of older people with potential medication-induced hyperactive delirium in the emergency department (ED); to identify the risk factors and the medicines frequently associated with the occurrence of the syndrome. Method A cross-sectional, retrospective study was performed with older people (age ≥ 60) admitted in 2018 to a Brazilian ED. The hospitalizations with suspected hyperactive delirium were screened with the aid of trigger-tools: International Code of Diseases-10th Revision, intra-hospital prescriptions of antipsychotics, and trigger-words related to the syndrome. A chart-review and medication review were developed to establish the causality assessment between adverse event and medicine. Logistic regression was used to determine risk factors for occurrence. Results Among the hospitalizations included, 67.5% (193/286) were screened by at least one trigger-tool. Of these, potential medication-induced hyperactive delirium was observed in 26.0% (50/193). The prevalence estimated in the ward was 17.5% (50/286). Opioids (31.9%), benzodiazepines (18.8%) and corticosteroids (10.6%) were the commonest medicines associated with delirium. Long-lived patients (p = 0.005), potentially inappropriate medicines (PIMs) (p = 0.025), and high weighted deliriogenic load (p = 0.014) were associated with potential medication-induced hyperactive delirium. Conclusion Approximately one in six hospitalizations of older people in the ED showed potential medication-induced hyperactive delirium. Data suggest PIMs and high weighted deliriogenic load, rather than polypharmacy or anticholinergic burden, are considered the most important characteristics of pharmacotherapy associated with avoidable hyperactive delirium among long-lived patients.

Similar content being viewed by others
References
Dani M, Owen LH, Jackson TA, et al. Delirium, frailty, and mortality: interactions in a prospective study of hospitalized older people. J Gerontol A Biol Sci Med Sci. 2018;73(3):415–8.
Oh ES, Fong TG, Hshieh TT, et al. Delirium in older persons: advances in diagnosis and treatment. JAMA. 2017;318(12):1161–74.
Minden SL, Carbone LA, Barsky A, et al. Predictors and outcomes of delirium. Gen Hosp Psychiatr. 2005;27(3):209–14.
Leslie DL, Marcantonio ER, Zhang Y, et al. One-year health care costs associated with delirium in the elderly population. Arch Intern Med. 2008;168(1):27–32.
Hshieh TT, Inouye SK, Oh ES. Delirium in the elderly. Clin Geriatr Med. 2020;36(2):183–99.
Ahmed S, Leurent B, Sampson EL. Risk factors for incident delirium among older people in acute hospital medical units: a systematic review and meta-analysis. Age Ageing. 2014;43(3):326–33.
Silva LOJE, Berning MJ, Stanich JA, et al. Risk factors for delirium in older adults in the emergency department: a systematic review and meta-analysis. Ann Emerg Med. 2021;78(4):549–65.
Carter GL, Dawson AH, Lopert R. Drug-induced delirium. Incidence, management and prevention. Drug Saf. 1996;15(4):291–330.
Catic AG. Identification and management of in-hospital drug-induced delirium in older patients. Drugs Aging. 2011;28(9):737–48.
Jennings ELM, Murphy KD, Gallagher P, et al. In-hospital adverse drug reactions in older adults; prevalence, presentation and associated drugs- a systematic review and meta-analysis. Age Ageing. 2020;49(6):948–58.
Egberts A, Moreno-Gonzáles R, Alan H, et al. Anticholinergic drug burden and delirium: a systematic review. J Am Med Dir Assoc. 2021;22(1):65–73.
Kassie GM, Ellet LMK, Nguyen TA, et al. Use of medicines that may precipitate delirium prior to hospitalisation in older Australians with delirium: an observational study. Australas J Ageing. 2019;38(2):124–31.
Rawle MJ, McCue L, Sampson EL, et al. Anticholinergic burden does not influence delirium subtype or the delirium-mortality association in hospitalized older adults: results from a prospective cohort study. Drugs Aging. 2021;38(3):233–42.
Pasina L, Colzani L, Cortesi L, et al. Relation between delirium and anticholinergic drug burden in a cohort of hospitalized older patients: an observational study. Drugs Aging. 2019;36(1):85–91.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5®). 5th ed. Arlington, VA, American Psychiatric Association, 2013.
Puelle MR, Kosar CM, Xu G, et al. The language of delirium: key words for identifying delirium from medical records. J Geront Nurs. 2015;41(8):34–42.
Nguyen PVQ, Pelletier L, Payot I, et al. Drug Delirium Scale (DDS): a tool to evaluate drugs as a risk factor for delirium. Int J Innov Res Med Sci. 2016;1(06):232–7.
Nery RT, Reis AM. Desenvolvimento de uma escala brasileira de medicamentos com atividade anticolinérgica. Einstein (São Paulo). 2019;17(2):eA4435.
AGS. American Geriatrics Society 2019 Updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2019; 67(4):674–694.
Melchiors AC, Correr CJ, Fernández-Llimos F. Translation and validation into Portuguese language of the medication regimen complexity index. Arq Bras Cardiol. 2007;89(4):191–6.
Forgerini M, Herdeiro MT, Galduróz JCF, et al. Risk factors associated with drug therapy among elderly people with Alzheimer’s disease: a cross-sectional study. Sao Paulo Med J. 2020;138(3):216–8.
Nguyen PVQ, Pelletier L, Payot I, et al. The delirium drug scale is associated to delirium incidence in the emergency department. Int Psychogeriatr. 2018;30(4):503–10.
Clegg A, Young JB. Which medications to avoid in people at risk of delirium: a systematic review. Age Ageing. 2011;40:23–9.
Swart LM, van der Zanden V, Spies PE, et al. The comparative risk of delirium with different opioids: a systematic review. Drugs Aging. 2017;34(6):437–43.
Alagiakrishnan K, Wiens CA. An approach to drug induced delirium in the elderly. Postgrad Med J. 2004;80(945):388–93.
Hwang S, Jun K, Ah YM, et al. Impact of anticholinergic burden on emergency department visits among older adults in Korea: a national population cohort study. Arch Gerontol Geriatr. 2019;85:103912.
World Health Organization. The use of the WHO-UMC system for standardised case causality assessment. http://www.who-umc.org/graphics/4409.pdf. Accessed 23 Oct 2019.
Gautron S, Wentzell J, Kanji S, et al. Characterization of serious adverse drug reactions in hospital to determine potential implications of mandatory reporting. Can J Hosp Pharm. 2018;71(5):316–23.
Daoust R, Paquet J, Boucher V, et al. Relationship between pain, opioid treatment, and delirium in older emergency department patients. Acad Emerg Med. 2020;27(8):708–16.
Kennedy M, Koehl J, Shenvi CL, et al. The agitated older adult in the emergency department: a narrative review of common causes and management strategies. J Am Coll Emerg Phys Open. 2020;1(5):812–23.
Pourmand A, Lombardi KM, Roberson J, et al. Patterns of benzodiazepine administration and prescribing to older adults in U.S. emergency departments. Aging Clin Exp Res. 2020;32(12):2621–8.
Sillner AY, Holle CL, Rudolph JL. The overlap between falls and delirium in hospitalized older adults. Clin Geriatri Med. 2019;35(2):221–36.
Crowe SF, Strankes EK. The residual medium and long-term cognitive effects of benzodiazepine use: an updated meta-analysis. Arch Clin Neuropsychol. 2018;33(7):901–11.
Zhong G, Wang Y, Zhang Y, et al. Association between benzodiazepine use and dementia: a meta-analysis. PLoS ONE. 2015;10(5):e0127836.
Pottie K, Thompson W, Davies S, et al. Deprescribing benzodiazepine receptor agonists: evidence-based clinical practice guideline. Can Fam Phys. 2018;64(5):339–51.
Schreiber MP, Colantuoni E, Bienvenu OJ, et al. Corticosteroids and transition to delirium in patients with acute lung injury. Crit Care Med. 2014;42(6):1480–6.
Dubovsky AN, Arvikar S, Stern TA, et al. The neuropsychiatric complications of glucocorticoid use: steroid psychosis revisited. Psychosomatics. 2012;53(2):103–15.
San-José A, Agustí A, Vidal X, et al. Inappropriate prescribing to the oldest old patients admitted to hospital: prevalence, most frequently used medicines, and associated factors. BMC Geriatr. 2015;15:42.
Weeda ER, AlDoughaim M, Criddle S. Association between potentially inappropriate medications and hospital encounters among older adults: a meta-analysis. Drugs Aging. 2020;37(7):529–37.
Adeola M, Azad R, Kassie GM, et al. Multicomponent interventions reduce high-risk medications for delirium in hospitalized older adults. J Am Geriatr Soc. 2018;66(8):1638–45.
Funding
This study was partially funded by São Paulo Research Foundation (FAPESP) scholarship Grant No 2019/19430–1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Raso, J., Santos, L.M.C., Reis, D.A. et al. Hospitalizations of older people in an emergency department related to potential medication-induced hyperactive delirium: a cross-sectional study. Int J Clin Pharm 44, 548–556 (2022). https://doi.org/10.1007/s11096-022-01378-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-022-01378-8