Abstract
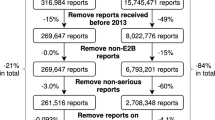
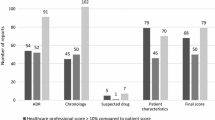
Background The quality of adverse drug reaction reports can have a strong influence on the causality assessment or the detection of safety signals. Various methods have been used to evaluate the quality of adverse drug reaction reports. Objective We used the vigiGrade completeness score to evaluate the quality of the Japanese adverse drug event report database (JADER). Methods Among all reports in the JADER (cases received by regulatory authorities from April 2004 to November 2018), 427,797 cases that did not meet the exclusion criteria were analyzed using vigiGrade. An report was considered a ‘well-documented’ report if the completeness score > 0.8. For each dimension, the proportion of incomplete information was calculated. Main outcome measure Proportion of ‘well-documented’ reports. Results A total of 211,774 (49.5%) cases were classified as ‘well-documented’ reports. When classified by sender, 6240 out of 8257 cases (75.6%) from medical institutions were ‘well-documented’, while 205,534 out of 419,540 cases (49.0%) from pharmaceutical companies were categorized as such. ‘Time-to-onset’ could not be calculated in 173,027 (41.2%) cases from the pharmaceutical companies and in 1228 (14.9%) cases from medical institutions. Conclusion In the JADER, the proportion of ‘well-documented’ adverse drug reaction reports from medical institutions was higher than that from pharmaceutical companies, and reports from medical institutions could help to clarify generated safety signals. We also found that more than 40% of the reports from pharmaceutical companies did not include information that is considered essential for the evaluation of any causal relationship between suspected drugs and adverse drug reactions, which could pose challenges to the detection of safety signals.





Similar content being viewed by others
References
Guidance for Industry: Good Pharmacovigilance Practices and Pharmacoepidemiologic Assessment. U.S. Department of Health and Human Services Food and Drug Administration (FDA), Center for Drug Evaluation and Research (CDER), and Center for Biologics Evaluation and Research (CBER), March 2005. https://www.fda.gov/downloads/drugs/guidancecomplianceregulatoryinformation/guidances/ucm071696.pdf. Accessed 6 Aug 2019.
Bergvall T, Norén GN, Lindquist M. vigiGrade: a tool to identify well-documented individual case reports and highlight systematic data quality issues. Drug Saf. 2014;37(1):65–77.
Plessis L, Gómez A, García N, Cereza G, Figueras A. Lack of essential information in spontaneous reports of adverse drug reactions in Catalonia-a restraint to the potentiality for signal detection. Eur J Clin Pharmacol. 2017;73(6):751–8.
Anonymous. The WHO Adverse Reactions Database On-line Searches User’s Manual. Uppsala Monitoring Centre, 1997. http://www.who.int/medicines/areas/quality_safety/safety_efficacy/advdrugreactions/en/. Accessed 31 Aug 2019.
Gedde-Dahl A, Harg P, Stenberg-Nilsen H, Buajordet M, Granas AG, Horn AM. Characteristics and quality of adverse drug reaction reports by pharmacists in Norway. Pharmacoepidemiol Drug Saf. 2007;16(9):999–1005.
van Grootheest AC, van Puijenbroek EP, de Jong-van den Berg LT. Contribution of pharmacists to the reporting of adverse drug reactions. Pharmacoepidemiol Drug Saf. 2002;11(3):205–10.
Rolfes L, van Hunsel F, van der Linden L, Taxis K, van Puijenbroek E. The quality of clinical information in adverse drug reaction reports by patients and healthcare professionals: a retrospective comparative analysis. Drug Saf. 2017;40(7):607–14.
Durrieu G, Jacquot J, Mège M, Bondon-Guitton E, Rousseau V, Montastruc F, et al. Completeness of spontaneous adverse drug reaction reports sent by general practitioners to a regional pharmacovigilance centre: a descriptive study. Drug Saf. 2016;39(12):1189–95.
Tuccori M, Giustarini G, Blandizzi C, Capogrosso-Sansone A, Rossi M, Gori G, et al. Quality of adverse drug reaction (QADRA) reports: an algorithm to appraise the efficiency of spontaneous reporting systems in pharmacovigilance. J Public Health. 2013;21:365–72.
Tsuchiya, M, Obara, T, Sakai, T, Nomura, K, Takamura, C, Mano, N. Quality evaluation of the Japanese adverse drug event report database (JADER). Pharmacoepidemiol Drug Saf. 2019. https://doi.org/10.1002/pds.4944. [Epub ahead of print].
Caster O, Sandberg L, Bergvall T, Watson S, Norén GN. vigiRank for statistical signal detection in pharmacovigilance: first results from prospective real-world use. Pharmacoepidemiol Drug Saf. 2017;26(8):1006–10.
Van Holle L, Tavares Da Silva F, Bauchau V. Signal detection based on time-to-onset: extending a new method from spontaneous reports to observational studies. Pharmacoepidemiol Drug Saf. 2014;23(8):849–58.
PMDA, Japanese Adverse Drug Event Report database (JADER), https://www.pmda.go.jp/safety/info-services/drugs/adr-info/suspected-adr/0003.html. Accessed 18 Dec 2019.
Lindquist M. VigiBase, the WHO global ICSR database system: basic facts. Drug Inf J. 2008;42(5):409–19.
Wakao R, Taavola H, Sandberg L, Iwasa E, Soejima S, Chandler R, et al. Data-driven identification of adverse event reporting patterns for Japan in VigiBase, the WHO global database of individual case safety reports. Drug Saf. 2019;42(12):1487–98.
McCarthy M. Drug maker’s adverse event reports are often incomplete, US report finds. Br Med J. 2015;350:h651.
Ministry of Health, Labour and Welfare, Pharmaceuticals and Medical Devices Safety Information No. 345, dated August 2017. https://www.pmda.go.jp/files/000219247.pdf. Accessed 31 Aug 2019.
MIC, recommendations based on administrative evaluations/monitoring results regarding pharmaceuticals—mainly focused on safety measures—dated June 2001 (Only available in Japanese language) http://www.soumu.go.jp/main_sosiki/hyouka/010608_2.htm. Accessed 31 Aug 2019.
MIC, recommendations based on administrative evaluations/monitoring results-regarding widespread use/safety of pharmaceuticals dated March 2013 (Only available in Japanese language) http://www.soumu.go.jp/main_content/000213386.pdf. Accessed 31 Aug 2019.
Rosli R, Ming LC, Abd Aziz N, Manan MM. A retrospective analysis of spontaneous adverse drug reactions reports relating to paediatric patients. PLoS ONE. 2016;11(6):e0155385.
Acknowledgements
This research was partially supported by the Research on Regulatory Harmonization and Evaluation of Pharmaceuticals, Medical Devices, Regenerative and Cellular Therapy Products, Gene Therapy Products, and Cosmetics from the Japan Agency for Medical Research and Development (AMED).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
Masami Tsuchiya, Taku Obara, Makoto Miyazaki, Aoi Noda, Chizuko Takamura, and Nariyasu Mano have no conflicts of interest directly relevant to the content of this study. Makoto Miyazaki is also an employee of a pharmaceutical company, MSDKK. However, he has no conflicts of interest directly relevant to the content of this study, as this study focuses on all marketed drugs in Japan but not on any specific drug.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Tsuchiya, M., Obara, T., Miyazaki, M. et al. The quality assessment of the Japanese Adverse Drug Event Report database using vigiGrade. Int J Clin Pharm 42, 728–736 (2020). https://doi.org/10.1007/s11096-020-00969-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11096-020-00969-7