Abstract
This review is a revisit of various oral drug absorption models developed in the past decades, focusing on how to incorporate the physiological dynamics in the upper gastrointestinal (GI) tract. For immediate-release oral drugs, GI absorption is a critical input of drug exposure and subsequent human body response, yet difficult to model largely due to the complex GI environment. One of the biggest hurdles lies at capturing the high within-subject variability (WSV) of bioavailability measures, which can be mechanistically explained by the GI physiological dynamics. A thorough summary of how GI dynamics is handled in the absorption models would promote the development of mechanism-based oral drug absorption models, aid in the design of clinical studies regarding dosing regimens and bioequivalence studies based on WSV, and advance the decision-making on formulation selection.
Graphical Abstract

Similar content being viewed by others
Data availability
No data were used in this manuscript.
References
Lennernas H. Human intestinal permeability. J Pharm Sci-US. 1998;87(4):403–10. https://doi.org/10.1021/js970332a.
Yu LX, Lipka E, Crison JR, Amidon GL. Transport approaches to the biopharmaceutical design of oral drug delivery systems: Prediction of intestinal absorption. Adv Drug Deliver Rev. 1996;19(3):359–76. https://doi.org/10.1016/0169-409x(96)00009-9.
Waiver of In Vivo Bioavailability and Bioequivalence Studies for Immediate-Release Solid Oral Dosage Forms Based on a Biopharmaceutics Classification System. U.S. Food and Drug Administration; 2017.
M9 Biopharmaceutics Classfication System-based Biowaivers. International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use; 2019.
Amidon GL, Lennernas H, Shah VP, Crison JR. A Theoretical Basis for a Biopharmaceutic Drug Classification - the Correlation of in-Vitro Drug Product Dissolution and in-Vivo Bioavailability. Pharmaceut Res. 1995;12(3):413–20. https://doi.org/10.1023/A:1016212804288.
Statistical Approaches to Establishing Bioequivalence. In: Research CfDEa, editor. Revision 1 ed. Rockville, MD, USA: U.S. Food and Drug Administration; 2022.
Tornoe CW, Overgaard RV, Agerso H, Nielsen HA, Madsen H, Jonsson EN. Stochastic differential equations in NONMEM: implementation, application, and comparison with ordinary differential equations. Pharm Res. 2005;22(8):1247–58. https://doi.org/10.1007/s11095-005-5269-5.
Wang K, Li Y, Chen B, Chen H, Smith DE, Sun D, et al. In Vitro Predictive Dissolution Test Should Be Developed and Recommended as a Bioequivalence Standard for the Immediate-Release Solid Oral Dosage Forms of the Highly Variable Mycophenolate Mofetil. Mol Pharm. 2022;19(7):2048–60. https://doi.org/10.1021/acs.molpharmaceut.1c00792.
Shah VP, Yacobi A, Barr WH, Benet LZ, Breimer D, Dobrinska MR, et al. Evaluation of orally administered highly variable drugs and drug formulations. Pharmaceut Res. 1996;13(11):1590–4. https://doi.org/10.1023/A:1016468018478.
Davit BM, Chen ML, Conner DP, Haidar SH, Kim S, Lee CH, et al. Implementation of a reference-scaled average bioequivalence approach for highly variable generic drug products by the US Food and Drug Administration. AAPS J. 2012;14(4):915–24. https://doi.org/10.1208/s12248-012-9406-x.
Cvijic S, Parojcic J, Langguth P. Viscosity-mediated negative food effect on oral absorption of poorly-permeable drugs with an absorption window in the proximal intestine: In vitro experimental simulation and computational verification. Eur J Pharm Sci. 2014;61:40–53. https://doi.org/10.1016/j.ejps.2014.04.008.
Barrett KE. Gastrointestinal physiology. 2nd ed. McGraw-Hill's AccessMedicine. New York, N.Y.: McGraw-Hill Education LLC, 2014.
Schuster MM, Crowell MD, Koch KL. Schuster atlas of gastrointestinal motility in health and disease. 2nd ed. Hamilton: B.C. Decker; 2002.
Johnson LR. Physiology of the gastrointestinal tract. 5th ed. London: Academic Press; 2012.
Food-Effect Bioavailability and Fed Bioequivalence Studies. U.S. Food and Drug Administration; 2018.
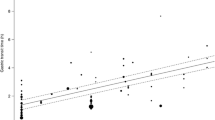
Wang K, Marciani L, Amidon GL, Smith DE, Sun D. Stochastic Differential Equation-based Mixed Effects Model of the Fluid Volume in the Fasted Stomach in Healthy Adult Human. AAPS J. 2023;25(5):76. https://doi.org/10.1208/s12248-023-00840-3.
Koziolek M, Alcaro S, Augustijns P, Basit AW, Grimm M, Hens B, et al. The mechanisms of pharmacokinetic food-drug interactions - A perspective from the UNGAP group. Eur J Pharm Sci. 2019;134:31–59. https://doi.org/10.1016/j.ejps.2019.04.003.
Ouyang A, Sunshine AG, Reynolds JC. Caloric Content of a Meal Affects Duration but Not Contractile Pattern of Duodenal Motility in Man. Digest Dis Sci. 1989;34(4):528–36. https://doi.org/10.1007/Bf01536328.
Siegel JA, Urbain JL, Adler LP, Charkes ND, Maurer AH, Krevsky B, et al. Biphasic Nature of Gastric-Emptying. Gut. 1988;29(1):85–9. https://doi.org/10.1136/gut.29.1.85.
Shore PA, Brodie BB, Hogben CA. The gastric secretion of drugs: a pH partition hypothesis. J Pharmacol Exp Ther. 1957;119(3):361–9.
Hens B, Tsume Y, Bermejo M, Paixao P, Koenigsknecht MJ, Baker JR, et al. Low Buffer Capacity and Alternating Motility along the Human Gastrointestinal Tract: Implications for in Vivo Dissolution and Absorption of Ionizable Drugs. Mol Pharm. 2017. https://doi.org/10.1021/acs.molpharmaceut.7b00426.
Mudie DM, Murray K, Hoad CL, Pritchard SE, Garnett MC, Amidon GL, et al. Quantification of gastrointestinal liquid volumes and distribution following a 240 mL dose of water in the fasted state. Mol Pharm. 2014;11(9):3039–47. https://doi.org/10.1021/mp500210c.
DiMagno EP. Regulation of interdigestive gastrointestinal motility and secretion. Digestion. 1997;58(Suppl 1):53–5.
Kalantzi L, Goumas K, Kalioras V, Abrahamsson B, Dressman JB, Reppas C. Characterization of the human upper gastrointestinal contents under conditions simulating bioavailability/bioequivalence studies. Pharmaceut Res. 2006;23(1):165–76. https://doi.org/10.1007/s11095-005-8476-1.
Clarysse S, Tack J, Lammert F, Duchateau G, Reppas C, Augustijns P. Postprandial evolution in composition and characteristics of human duodenal fluids in different nutritional states. J Pharm Sci. 2009;98(3):1177–92. https://doi.org/10.1002/jps.21502.
Kaunitz JD, Akiba Y. Review article: duodenal bicarbonate - mucosal protection, luminal chemosensing and acid-base balance. Aliment Pharmacol Ther. 2006;24(Suppl 4):169–76. https://doi.org/10.1111/j.1365-2036.2006.00041.x.
Hogan DL, Ainsworth MA, Isenberg JI. Review article: gastroduodenal bicarbonate secretion. Aliment Pharmacol Ther. 1994;8(5):475–88.
Fuchs A, Dressman JB. Composition and physicochemical properties of fasted-state human duodenal and jejunal fluid: a critical evaluation of the available data. J Pharm Sci. 2014;103(11):3398–411. https://doi.org/10.1002/jps.24183.
McNamara DP, Whitney KM, Goss SL. Use of a physiologic bicarbonate buffer system for dissolution characterization of ionizable drugs. Pharmaceut Res. 2003;20(10):1641–6. https://doi.org/10.1023/A:1026147620304.
Koziolek M, Schneider F, Grimm M, Modebeta C, Seekamp A, Roustom T, et al. Intragastric pH and pressure profiles after intake of the high-caloric, high-fat meal as used for food effect studies. J Control Release. 2015;220(Pt A):71–8. https://doi.org/10.1016/j.jconrel.2015.10.022.
Dressman JB, Berardi RR, Dermentzoglou LC, Russell TL, Schmaltz SP, Barnett JL, et al. Upper gastrointestinal (GI) pH in young, healthy men and women. Pharm Res. 1990;7(7):756–61. https://doi.org/10.1023/a:1015827908309.
Russell TL, Berardi RR, Barnett JL, Dermentzoglou LC, Jarvenpaa KM, Schmaltz SP, et al. Upper gastrointestinal pH in seventy-nine healthy, elderly, North American men and women. Pharm Res. 1993;10(2):187–96. https://doi.org/10.1023/a:1018970323716.
Cheng LS, Wong H. Food effects on oral drug absorption: application of physiologically-based pharmacokinetic modeling as a predictive tool. Pharmaceutics. 2020;12(7). ARTN 672. https://doi.org/10.3390/pharmaceutics12070672.
Koziolek M, Grimm M, Schneider F, Jedamzik P, Sager M, Kuhn JP, et al. Navigating the human gastrointestinal tract for oral drug delivery: Uncharted waters and new frontiers. Adv Drug Deliv Rev. 2016;101:75–88. https://doi.org/10.1016/j.addr.2016.03.009.
Grimm M, Koziolek M, Kuhn JP, Weitschies W. Interindividual and intraindividual variability of fasted state gastric fluid volume and gastric emptying of water. Eur J Pharm Biopharm. 2018;127:309–17. https://doi.org/10.1016/j.ejpb.2018.03.002.
Koziolek M, Grimm M, Garbacz G, Kuhn JP, Weitschies W. Intragastric volume changes after intake of a high-caloric, high-fat standard breakfast in healthy human subjects investigated by MRI. Mol Pharm. 2014;11(5):1632–9. https://doi.org/10.1021/mp500022u.
Pentafragka C, Vertzoni M, Symillides M, Goumas K, Reppas C. Disposition of two highly permeable drugs in the upper gastrointestinal lumen of healthy adults after a standard high-calorie, high-fat meal. Eur J Pharm Sci. 2020;149:105351. https://doi.org/10.1016/j.ejps.2020.105351.
Schiller C, Frohlich CP, Giessmann T, Siegmund W, Monnikes H, Hosten N, et al. Intestinal fluid volumes and transit of dosage forms as assessed by magnetic resonance imaging. Aliment Pharm Therap. 2005;22(10):971–9. https://doi.org/10.1111/j.1365-2036.2005.02683.x.
Mudie DM, Amidon GL, Amidon GE. Physiological parameters for oral delivery and in vitro testing. Mol Pharm. 2010;7(5):1388–405. https://doi.org/10.1021/mp100149j.
de la Cruz Perez, Moreno M, Oth M, Deferme S, Lammert F, Tack J, Dressman J, et al. Characterization of fasted-state human intestinal fluids collected from duodenum and jejunum. J Pharm Pharmacol. 2006;58(8):1079–89. https://doi.org/10.1211/jpp.58.8.0009.
Riethorst D, Mols R, Duchateau G, Tack J, Brouwers J, Augustijns P. Characterization of Human Duodenal Fluids in Fasted and Fed State Conditions. J Pharm Sci. 2016;105(2):673–81. https://doi.org/10.1002/jps.24603.
Keszthelyi D, Knol D, Troost FJ, van Avesaat M, Foltz M, Masclee AA. Time of ingestion relative to meal intake determines gastrointestinal responses to a plant sterol-containing yoghurt drink. Eur J Nutr. 2013;52(4):1417–20. https://doi.org/10.1007/s00394-012-0440-3.
Marciani L, Gowland PA, Spiller RC, Manoj P, Moore RJ, Young P, et al. Gastric response to increased meal viscosity assessed by echo-planar magnetic resonance imaging in humans. J Nutr. 2000;130(1):122–7. https://doi.org/10.1093/jn/130.1.122.
Thomas G, Girre C, Scherrmann JM, Francheteau P, Steimer JL. Zero-order absorption and linear disposition of oral colchicine in healthy volunteers. Eur J Clin Pharmacol. 1989;37(1):79–84. https://doi.org/10.1007/BF00609430.
Wagner JG, Nelson E. Per cent absorbed time plots derived from blood level and/or urinary excretion data. J Pharm Sci. 1963;52:610–1. https://doi.org/10.1002/jps.2600520629.
Loo JC, Riegelman S. New method for calculating the intrinsic absorption rate of drugs. J Pharm Sci. 1968;57(6):918–28. https://doi.org/10.1002/jps.2600570602.
Rousseau A, Leger F, Le Meur Y, Saint-Marcoux F, Paintaud G, Buchler M, et al. Population pharmacokinetic modeling of oral cyclosporin using NONMEM: comparison of absorption pharmacokinetic models and design of a Bayesian estimator. Ther Drug Monit. 2004;26(1):23–30. https://doi.org/10.1097/00007691-200402000-00006.
Savic RM, Jonker DM, Kerbusch T, Karlsson MO. Implementation of a transit compartment model for describing drug absorption in pharmacokinetic studies. J Pharmacokinet Pharmacodyn. 2007;34(5):711–26. https://doi.org/10.1007/s10928-007-9066-0.
Karatza E, Karalis V. Delay differential equations for the description of Irbesartan pharmacokinetics: A population approach to model absorption complexities leading to dual peaks. Eur J Pharm Sci. 2020;153:105498. https://doi.org/10.1016/j.ejps.2020.105498.
Higaki K, Yamashita S, Amidon GL. Time-dependent oral absorption models. J Pharmacokinet Pharmacodyn. 2001;28(2):109–28.
Garrigues TM, Martin U, Peris-Ribera JE, Prescott LF. Dose-dependent absorption and elimination of cefadroxil in man. Eur J Clin Pharmacol. 1991;41(2):179–83. https://doi.org/10.1007/BF00265914.
Cosson VF, Fuseau E. Mixed effect modeling of sumatriptan pharmacokinetics during drug development: II. From healthy subjects to phase 2 dose ranging in patients. J Pharmacokinet Biopharm. 1999;27(2):149–71. https://doi.org/10.1023/a:1020601906027.
Riad LE, Chan KK, Wagner WE Jr, Sawchuk RJ. Simultaneous first- and zero-order absorption of carbamazepine tablets in humans. J Pharm Sci. 1986;75(9):897–900. https://doi.org/10.1002/jps.2600750916.
Locatelli I, Mrhar A, Bogataj M. Gastric Emptying of Pellets under Fasting Conditions: A Mathematical Model. Pharmaceut Res. 2009;26(7):1607–17. https://doi.org/10.1007/s11095-009-9869-3.
Wu K, Cohen EE, House LK, Ramirez J, Zhang W, Ratain MJ, et al. Nonlinear population pharmacokinetics of sirolimus in patients with advanced cancer. CPT Pharmacometrics Syst Pharmacol. 2012;1:e17. https://doi.org/10.1038/psp.2012.18.
Ogungbenro K, Pertinez H, Aarons L. Empirical and semi-mechanistic modelling of double-peaked pharmacokinetic profile phenomenon due to gastric emptying. AAPS J. 2015;17(1):227–36. https://doi.org/10.1208/s12248-014-9693-5.
Paixao P, Bermejo M, Hens B, Tsume Y, Dickens J, Shedden K, et al. Gastric emptying and intestinal appearance of nonabsorbable drugs phenol red and paromomycin in human subjects: A multi-compartment stomach approach. Eur J Pharm Biopharm. 2018;129:162–74. https://doi.org/10.1016/j.ejpb.2018.05.033.
Csajka C, Drover D, Verotta D. The use of a sum of inverse Gaussian functions to describe the absorption profile of drugs exhibiting complex absorption. Pharmaceut Res. 2005;22(8):1227–35. https://doi.org/10.1007/s11095-005-5266-8.
Karatza E, Karalis V. Modelling gastric emptying: A pharmacokinetic model simultaneously describing distribution of losartan and its active metabolite EXP-3174. Basic Clin Pharmacol Toxicol. 2020;126(3):193–202. https://doi.org/10.1111/bcpt.13321.
Talattof A, Price JC, Amidon GL. Gastrointestinal Motility Variation and Implications for Plasma Level Variation: Oral Drug Products. Mol Pharmaceut. 2016;13(2):557–67. https://doi.org/10.1021/acs.molpharmaceut.5b00774.
Karatza E, Karalis V. Investigating the Impact of Gastric Emptying on Pharmacokinetic Parameters Using Delay Differential Equations and Principal Component Analysis. Eur J Drug Metab Ph. 2021. https://doi.org/10.1007/s13318-021-00683-3.
Abuhelwa AY, Foster DJR, Upton RN. A Quantitative Review and Meta-models of the Variability and Factors Affecting Oral Drug Absorption-Part II: Gastrointestinal Transit Time. AAPS J. 2016;18(5):1322–33. https://doi.org/10.1208/s12248-016-9953-7.
Abuhelwa AY, Foster DJR, Upton RN. A Quantitative Review and Meta-Models of the Variability and Factors Affecting Oral Drug Absorption-Part I: Gastrointestinal pH. AAPS J. 2016;18(5):1309–21. https://doi.org/10.1208/s12248-016-9952-8.
Plusquellec Y, Campistron G, Staveris S, Barre J, Jung L, Tillement JP, et al. A double-peak phenomenon in the pharmacokinetics of veralipride after oral administration: a double-site model for drug absorption. J Pharmacokinet Biopharm. 1987;15(3):225–39. https://doi.org/10.1007/BF01066319.
Henin E, Bergstrand M, Weitschies W, Karlsson MO. Meta-analysis of Magnetic Marker Monitoring Data to Characterize the Movement of Single Unit Dosage Forms Though the Gastrointestinal Tract Under Fed and Fasting Conditions. Pharmaceut Res. 2016;33(3):751–62. https://doi.org/10.1007/s11095-015-1824-x.
Yun HY, Joo Lee E, Youn Chung S, Choi SO, Kee Kim H, Kwon JT, et al. The effects of food on the bioavailability of fenofibrate administered orally in healthy volunteers via sustained-release capsule. Clin Pharmacokinet. 2006;45(4):425–32. https://doi.org/10.2165/00003088-200645040-00007.
Dressman JB, Fleisher D. Mixing-tank model for predicting dissolution rate control or oral absorption. J Pharm Sci. 1986;75(2):109–16. https://doi.org/10.1002/jps.2600750202.
Dressman JB, Fleisher D, Amidon GL. Physicochemical model for dose-dependent drug absorption. J Pharm Sci. 1984;73(9):1274–9. https://doi.org/10.1002/jps.2600730922.
Yu LX, Amidon GL. A compartmental absorption and transit model for estimating oral drug absorption. Int J Pharmaceut. 1999;186(2):119–25. https://doi.org/10.1016/S0378-5173(99)00147-7.
Agoram B, Woltosz WS, Bolger MB. Predicting the impact of physiological and biochemical processes on oral drug bioavailability. Adv Drug Deliv Rev. 2001;50(Suppl 1):S41-67.
Jamei M, Marciniak S, Feng K, Barnett A, Tucker G, Rostami-Hodjegan A. The Simcyp population-based ADME simulator. Expert Opin Drug Metab Toxicol. 2009;5(2):211–23. https://doi.org/10.1517/17425250802691074.
Arora S, Pansari A, Kilford P, Jamei M, Gardner I, Turner DB. Biopharmaceutic In Vitro In Vivo Extrapolation (IVIV_E) Informed Physiologically-Based Pharmacokinetic Model of Ritonavir Norvir Tablet Absorption in Humans Under Fasted and Fed State Conditions. Mol Pharm. 2020;17(7):2329–44. https://doi.org/10.1021/acs.molpharmaceut.0c00043.
Wang J, Flanagan DR. General solution for diffusion-controlled dissolution of spherical particles. 1. Theory. J Pharm Sci. 1999;88(7):731–8. https://doi.org/10.1021/js980236p.
Sjogren E, Westergren J, Grant I, Hanisch G, Lindfors L, Lennernas H, et al. In silico predictions of gastrointestinal drug absorption in pharmaceutical product development: application of the mechanistic absorption model GI-Sim. Eur J Pharm Sci. 2013;49(4):679–98. https://doi.org/10.1016/j.ejps.2013.05.019.
Sjogren E, Thorn H, Tannergren C. In Silico Modeling of Gastrointestinal Drug Absorption: Predictive Performance of Three Physiologically Based Absorption Models. Mol Pharm. 2016;13(6):1763–78. https://doi.org/10.1021/acs.molpharmaceut.5b00861.
Demeester C, Robins D, Edwina AE, Tournoy J, Augustijns P, Ince I, et al. Physiologically based pharmacokinetic (PBPK) modelling of oral drug absorption in older adults - an AGePOP review. Eur J Pharm Sci. 2023;188:106496. https://doi.org/10.1016/j.ejps.2023.106496.
Jamei M, Turner D, Yang J, Neuhoff S, Polak S, Rostami-Hodjegan A, et al. Population-based mechanistic prediction of oral drug absorption. AAPS J. 2009;11(2):225–37. https://doi.org/10.1208/s12248-009-9099-y.
Chirumamilla SK, Banala VT, Jamei M, Turner DB. Mechanistic PBPK modelling to predict the advantage of the salt form of a drug when dosed with acid reducing agents. Pharmaceutics. 2021;13(8). https://doi.org/10.3390/pharmaceutics13081169.
Oberle RL, Amidon GL. The influence of variable gastric emptying and intestinal transit rates on the plasma level curve of cimetidine; an explanation for the double peak phenomenon. J Pharmacokinet Biopharm. 1987;15(5):529–44. https://doi.org/10.1007/BF01061761.
Langguth P, Lee KM, Spahn-Langguth H, Amidon GL. Variable gastric emptying and discontinuities in drug absorption profiles: dependence of rates and extent of cimetidine absorption on motility phase and pH. Biopharm Drug Dispos. 1994;15(9):719–46.
Stamatis SD, Rose JP. Lilly Absorption Modeling Platform: A Tool for Early Absorption Assessment. Mol Pharm. 2022;19(1):213–26. https://doi.org/10.1021/acs.molpharmaceut.1c00726.
Talattof A, Amidon GL. Pulse Packet Stochastic Model for Gastric Emptying in the Fasted State: A Physiological Approach. Mol Pharmaceut. 2018;15(6):2107–15. https://doi.org/10.1021/acs.molpharmaceut.7b01077.
Stamatopoulos K, Pathak SM, Marciani L, Turner DB. Population-Based PBPK Model for the Prediction of Time-Variant Bile Salt Disposition within GI Luminal Fluids. Mol Pharm. 2020;17(4):1310–23. https://doi.org/10.1021/acs.molpharmaceut.0c00019.
Langenbucher F. Linearization of dissolution rate curves by the Weibull distribution. J Pharm Pharmacol. 1972;24(12):979–81. https://doi.org/10.1111/j.2042-7158.1972.tb08930.x.
Stubbs DF. Models of gastric emptying. Gut. 1977;18(3):202–7. https://doi.org/10.1136/gut.18.3.202.
Yokrattanasak J, De Gaetano A, Panunzi S, Satiracoo P, Lawton WM, Lenbury Y. A Simple, Realistic Stochastic Model of Gastric Emptying. PLoS One. 2016;11(4):e0153297. https://doi.org/10.1371/journal.pone.0153297.
Liu B, Jamei M, Rostami-Hodjegan A, Turner DB. PBPK modeling of Negative Food Effects upon Oral Drug Absorption of the BCS Class III Drug Trospium Chloride (TC): Combination of a Dynamic Viscosity-Disintegration Model and the ADAM (Advanced Dissolution, Absorption and Metabolism. 2013 AAPS Annual Meeting and Exposition. San Antonio, USA 2013.
Liu B, Jamei M, Rostami-Hodjegan A, Turner DB. Toward Mechanistic Modeling of Negative Food Effects upon Oral Drug Absorption: Linking In Vivo Dynamic Dilution of Digesta to Viscosity, Disintegration and Dissolution Rate. 2013 AAPS Annual Meeting and Exposition. San Antonio, USA 2013.
Koenigsknecht MJ, Baker JR, Wen B, Frances A, Zhang H, Yu A, et al. In Vivo Dissolution and Systemic Absorption of Immediate Release Ibuprofen in Human Gastrointestinal Tract under Fed and Fasted Conditions. Mol Pharm. 2017;14(12):4295–304. https://doi.org/10.1021/acs.molpharmaceut.7b00425.
Mikolajczyk AE, Watson S, Surma BL, Rubin DT. Assessment of Tandem Measurements of pH and Total Gut Transit Time in Healthy Volunteers. Clin Transl Gastroenterol. 2015;6:e100. https://doi.org/10.1038/ctg.2015.22.
Gao H, Shanmugasundaram V, Lee P. Estimation of aqueous solubility of organic compounds with QSPR approach. Pharm Res. 2002;19(4):497–503. https://doi.org/10.1023/a:1015103914543.
Chevillard F, Lagorce D, Reynes C, Villoutreix BO, Vayer P, Miteva MA. In silico prediction of aqueous solubility: a multimodel protocol based on chemical similarity. Mol Pharm. 2012;9(11):3127–35. https://doi.org/10.1021/mp300234q.
Raevsky OA, Polianczyk DE, Grigorev VY, Raevskaja OE, Dearden JC. In silico Prediction of Aqueous Solubility: a Comparative Study of Local and Global Predictive Models. Mol Inform. 2015;34(6–7):417–30. https://doi.org/10.1002/minf.201400144.
Wang NN, Dong J, Deng YH, Zhu MF, Wen M, Yao ZJ, et al. ADME Properties Evaluation in Drug Discovery: Prediction of Caco-2 Cell Permeability Using a Combination of NSGA-II and Boosting. J Chem Inf Model. 2016;56(4):763–73. https://doi.org/10.1021/acs.jcim.5b00642.
Miljkovic F, Martinsson A, Obrezanova O, Williamson B, Johnson M, Sykes A, et al. Machine Learning Models for Human In Vivo Pharmacokinetic Parameters with In-House Validation. Mol Pharm. 2021;18(12):4520–30. https://doi.org/10.1021/acs.molpharmaceut.1c00718.
Ahmed SS, Ramakrishnan V. Systems biological approach of molecular descriptors connectivity: optimal descriptors for oral bioavailability prediction. PLoS One. 2012;7(7):e40654. https://doi.org/10.1371/journal.pone.0040654.
Xu X, Zhang W, Huang C, Li Y, Yu H, Wang Y, et al. A novel chemometric method for the prediction of human oral bioavailability. Int J Mol Sci. 2012;13(6):6964–82. https://doi.org/10.3390/ijms13066964.
Tian S, Li Y, Wang J, Zhang J, Hou T. ADME evaluation in drug discovery. 9. Prediction of oral bioavailability in humans based on molecular properties and structural fingerprints. Mol Pharm. 2011;8(3):841–51. https://doi.org/10.1021/mp100444g.
Xu Y, Ma J, Liaw A, Sheridan RP, Svetnik V. Demystifying Multitask Deep Neural Networks for Quantitative Structure-Activity Relationships. J Chem Inf Model. 2017;57(10):2490–504. https://doi.org/10.1021/acs.jcim.7b00087.
Wright MR. Opportunities and Considerations in the Application of Artificial Intelligence to Pharmacokinetic Prediction. Methods Mol Biol. 2022;2390:461–82. https://doi.org/10.1007/978-1-0716-1787-8_21.
Poynton MR, Choi BM, Kim YM, Park IS, Noh GJ, Hong SO, et al. Machine learning methods applied to pharmacokinetic modelling of remifentanil in healthy volunteers: a multi-method comparison. J Int Med Res. 2009;37(6):1680–91. https://doi.org/10.1177/147323000903700603.
Gao F, Xu J, Liu H, Shi P. Reinforcement Learning Based Model Selection and Parameter Estimation for Pharmacokinetic Analysis in Drug Selection. In: Liao H, Linte CA, Masamune K, Peters TM, Zheng G, editors. MIAR AE-CAI 2013: Springer. Berlin: Heidelberg; 2013. p. 221–30.
Liu X, Liu C, Huang R, Zhu H, Liu Q, Mitra S, et al. Long short-term memory recurrent neural network for pharmacokinetic-pharmacodynamic modeling. Int J Clin Pharmacol Ther. 2021;59(2):138–46. https://doi.org/10.5414/CP203800.
Lu J, Deng K, Zhang X, Liu G, Guan Y. Neural-ODE for pharmacokinetics modeling and its advantage to alternative machine learning models in predicting new dosing regimens. iScience. 2021;24(7):102804. https://doi.org/10.1016/j.isci.2021.102804.
Acknowledgements
This review was adapted from the Chapter 1 of the PhD thesis of Kai Wang entitled with “Mechanistic Model-based Drug Oral Absorption Analysis” with additional summary and discussion. Special appreciation goes to the anonymous reviewers who made insightful and constructive comments to improve the quality of this manuscript.
Author information
Authors and Affiliations
Contributions
Dr. Wang drafted the manuscript. Dr. Amidon and Dr. Smith revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
Nothing to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wang, K., Amidon, G.L. & Smith, D.E. Physiological Dynamics in the Upper Gastrointestinal Tract and the Development of Gastrointestinal Absorption Models for the Immediate-Release Oral Dosage Forms in Healthy Adult Human. Pharm Res 40, 2607–2626 (2023). https://doi.org/10.1007/s11095-023-03597-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-023-03597-8