Abstract
Purpose
The goal of the study was to evaluate a miniaturized dissolution-permeation apparatus (μFLUX™ apparatus) for its ability to benchmark several itraconazole (ITZ) formulations for which in vivo PK data was available in the literature.
Method
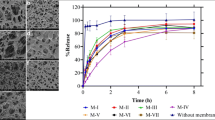
Untreated and micronized powders of ITZ and various enabling formulations of ITZ (commercial Sporanox® solid dispersion, a Soluplus®-based solid dispersion and a nanosuspension) were introduced to the donor compartment of μFLUX™ apparatus. Donor and acceptor chambers were divided from each other by a lipophilic membrane. In addition to the flux evaluations, changes in solid state as a function of time were investigated to gain further insight into the flux changes observed over time for the solid dispersion formulations.
Results
Initial flux values from Sporanox®, the nanosuspension and the micronized ITZ showed ratios of 52/4/1 with a decreasing flux from nanosuspension and both solid dispersions after 2.5–3 h. Although the initial flux from the Soluplus® formulation was 2.2 times lower than the one observed for Sporanox®, the decrease in flux observed was milder and became ~ 2 times higher than Sporanox® after approximately 2.5 h. The total amounts of ITZ in the receiver compartment after 240 min showed the same rank order as the rodent AUCs of these formulations reported in literature.
Conclusions
It was demonstrated that in vitro flux measurements using lipophilic artificial membranes could correctly reproduce the rank order of PK results for ITZ formulations. The drop in flux over time for solid dispersions could be backed by experimental indications of crystallization.










Similar content being viewed by others
Abbreviations
- A:
-
Area (cm2)
- ABL:
-
Aqueous boundary layer;
- ACN:
-
Acetonitrile;
- API:
-
Active pharmaceutical ingredient;
- ASB:
-
Acceptor sink buffer;
- ASD:
-
Amorphous solid dispersion;
- C:
-
Concentration (μg/mL), subscripts D or R refer to donor or receiver;
- Daq :
-
Aqueous diffusion coefficient (cm2 s−1);
- Deff :
-
Effective diffusion coefficient (cm2 s−1);
- DLS:
-
Dynamic light scattering;
- DMSO:
-
Dimethyl sulfoxide;
- DSC:
-
Differential scanning calorimetry;
- FaSSGF:
-
Fasted state simulated gastric fluid;
- FaSSIF:
-
Fasted state simulated intestinal fluid;
- FeSSIF:
-
Fed state simulated intestinal fluid;
- GIT:
-
Gastrointestinal;
- hABL :
-
Thickness of aqueous boundary layer;
- HCl:
-
Hydrochloric acid;
- HME:
-
Hot melt extrusion;
- HPC-L:
-
Hydroxypropylcellulose;
- HPβCD:
-
Hydroxypropyl-β-cyclodextrin;
- HPMC:
-
Hydroxypropyl methylcellulose;
- ITZ:
-
Itraconazole, a studied compound;
- J:
-
Flux (μg min−1 cm−2)
- LLD:
-
Laser light diffraction;
- OH-ITZ:
-
Hydroxy-itraconazole;
- PABL :
-
ABL permeability (cm s−1);
- Pe :
-
Effective permeability (cm s−1);
- Pm :
-
Membrane permeability (cm s−1);
- PAMPA:
-
Parallel artificial membrane permeability assay;
- PK:
-
Pharmacokinetic;
- PVDF:
-
Polyvinylidenfluoride;
- SEM:
-
Scanning electron microscopy;
- TFA:
-
Trifluoroacetic acid;
- UPLC:
-
Ultra performance liquid chromatography;
- V:
-
Volume (mL);
- v/v/v:
-
Volume/volume/volume;
- w/w:
-
Weight/weight;
- XRPD:
-
X-ray powder diffraction;
References
Avdeef A, Kansy M, Bendels S, Tsinman K. Absorption-excipient-pH classification gradient maps: sparingly soluble drugs and the pH partition hypothesis. Eur J Pharm Sci. 2008;33(1):29–41.
Dahan A, Miller J, Hoffman A, Amidon G, Amidon G. The solubility–permeability interplay in using Cyclodextrins as pharmaceutical Solubilizers: mechanistic modeling and application to progesterone. J Pharm Sci. 2010;99(6):2739–49.
Miller J, Beig A, Krieg B, Carr R, Borchardt T, Amidon G, et al. The solubility–permeability interplay: mechanistic modeling and predictive application of the impact of micellar Solubilization on intestinal permeation. Mol Pharm. 2011;8(5):1848–56.
Dahan A, Miller J. The solubility–permeability interplay and its implications in formulation design and development for poorly soluble drugs. AAPS J. 2012;14(2):244–51.
Frank K, Rosenblatt K, Westedt U, Hölig P, Rosenberg J, Mägerlein M, et al. Amorphous solid dispersion enhances permeation of poorly soluble ABT-102: true supersaturation vs. apparent solubility enhancement. Int J Pharm. 2012;437(1–2):288–93.
Beig A, Miller J, Dahan A. Accounting for the solubility–permeability interplay in oral formulation development for poor water solubility drugs: the effect of PEG-400 on carbamazepine absorption. Eur J Pharm Biopharm. 2012;81(2):386–91.
Miller J, Beig A, Carr R, Spence J, Dahan A. A win–win solution in oral delivery of lipophilic drugs: supersaturation via amorphous solid dispersions increases apparent solubility without sacrifice of intestinal membrane permeability. Mol Pharm. 2012;9(7):2009–16.
Miller J, Beig A, Carr R, Webster G, Dahan A. The solubility–permeability interplay when using Cosolvents for Solubilization: revising the way we use solubility-enabling formulations. Mol Pharm. 2012;9(3):581–90.
Dahan A, Beig A, Ioffe-Dahan V, Agbaria R, Miller J. The twofold advantage of the amorphous form as an oral drug delivery practice for lipophilic compounds: increased apparent solubility and drug flux through the intestinal membrane. AAPS J. 2012;15(2):347–53.
Beig A, Miller J, Dahan A. The interaction of nifedipine with selected cyclodextrins and the subsequent solubility–permeability trade-off. Eur J Pharm Biopharm. 2013;85(3):1293–9.
Kataoka M, Yano K, Hamatsu Y, Masaoka Y, Sakuma S, Yamashita S. Assessment of absorption potential of poorly water-soluble drugs by using the dissolution/permeation system. Eur J Pharm Biopharm. 2013;85(3):1317–24.
Frank K, Westedt U, Rosenblatt K, Hölig P, Rosenberg J, Mägerlein M, et al. What is the mechanism behind increased permeation rate of a poorly soluble drug from aqueous dispersions of an amorphous solid dispersion? J Pharm Sci. 2014;103(6):1779–86.
Raina S, Zhang G, Alonzo D, Wu J, Zhu D, Catron N, et al. Enhancements and limits in drug membrane transport using supersaturated solutions of poorly water soluble drugs. J Pharm Sci. 2014;103(9):2736–48.
Beig A, Miller J, Lindley D, Carr R, Zocharski P, Agbaria R, et al. Head-to-head comparison of different solubility-enabling formulations of etoposide and their consequent solubility–permeability interplay. J Pharm Sci. 2015;104(9):2941–7.
Trasi N, Taylor L. Thermodynamics of highly supersaturated aqueous solutions of poorly water-soluble drugs—impact of a second drug on the solution phase behavior and implications for combination products. J Pharm Sci. 2015;104(8):2583–93.
Raina S, Zhang G, Alonzo D, Wu J, Zhu D, Catron N, et al. Impact of solubilizing additives on supersaturation and membrane transport of drugs. Pharm Res. 2015;32(10):3350–64.
Beig A, Agbaria R, Dahan A. The use of captisol (SBE7-β-CD) in oral solubility-enabling formulations: comparison to HPβCD and the solubility–permeability interplay. Eur J Pharm Sci. 2015;77:73–8.
Fong S, Martins S, Brandl M, Bauer-Brandl A. Solid phospholipid dispersions for oral delivery of poorly soluble drugs: investigation into celecoxib incorporation and solubility-in vitro permeability enhancement. J Pharm Sci. 2016;105(3):1113–23.
Beig A, Lindley D, Miller J, Agbaria R, Dahan A. Hydrotropic solubilization of lipophilic drugs for oral delivery: the effects of urea and nicotinamide on carbamazepine solubility–permeability interplay. Front Pharmacol. 2016;7:379.
Indulkar A, Gao Y, Raina S, Zhang G, Taylor L. Exploiting the phenomenon of liquid–liquid phase separation for enhanced and sustained membrane transport of a poorly water-soluble drug. Mol Pharm. 2016;13(6):2059–69.
Jackson M, Kestur U, Hussain M, Taylor L. Dissolution of Danazol amorphous solid dispersions: supersaturation and phase behavior as a function of drug loading and polymer type. Mol Pharm. 2016;13(1):223–31.
Dahan A, Beig A, Lindley D, Miller J. The solubility–permeability interplay and oral drug formulation design: two heads are better than one. Adv Drug Deliv Rev. 2016;101:99–107.
Beig A, Miller J, Lindley D, Dahan A. Striking the optimal solubility–permeability balance in oral formulation development for lipophilic drugs: maximizing carbamazepine blood levels. Mol Pharm. 2017;14(1):319–27.
Forner K, Holm R, Morakul B, Junyaprasert VB, Ackermann M, Mazur J, et al. Dissolution and dissolution/permeation experiments for predicting systemic exposure following oral administration of the BCS class II drug clarithromycin. Eur J Pharm Sci. 2017;101:211–9.
Sironi D, Rosenberg J, Bauer-Brandl A, Brandl M. Dynamic dissolution−/permeation-testing of nano- and microparticle formulations of fenofibrate. Eur J Pharm Sci. 2017;96:20–7.
Fong S, Poulsen J, Brandl M, Bauer-Brandl A. A novel microdialysis-dissolution/permeation system for testing oral dosage forms: a proof-of-concept study. Eur J Pharm Sci. 2017;96:154–63.
Lu J, Ormes J, Lowinger M, Xu W, Mitra A, Mann A, et al. Impact of endogenous bile salts on the thermodynamics of supersaturated active pharmaceutical ingredient solutions. Cryst Growth Des. 2017;17(3):1264–75.
Bailey EM, Krakovsky DJ, Rybak MJ. The triazole antifungal agents – a review of itraconazole and fluconazole. Pharmacotherapy. 1990;10(2):146–53.
Matsui K, Tsume Y, Amidon G, Amidon G. The evaluation of in vitro drug dissolution of commercially available oral dosage forms for Itraconazole in gastrointestinal simulator with biorelevant media. J Pharm Sci. 2016;105(9):2804–14.
Zhang S, Lee T, Chow A. Crystallization of Itraconazole polymorphs from melt. Cryst Growth Des. 2016;16(7):3791–801.
Zhang K, Yu H, Luo Q, Yang S, Lin X, Zhang Y, et al. Increased dissolution and oral absorption of itraconazole/Soluplus extrudate compared with itraconazole nanosuspension. Eur J Pharm Biopharm. 2013;85(3):1285–92.
Avdeef A, Tsinman O. PAMPA - a drug absorption in vitro model: 13. Chemical selectivity due to membrane hydrogen bonding: in combo comparisons of HDM-, DOPC-, and DS-PAMPA models. Eur J Pharm Sci. 2006;28(1–2):43–50.
Avdeef A. Absorption and drug development: solubility, permeability, and charge state. Second Edition. Hoboken: Wiley & Sons, Inc.; 2012.
Scardi P, Leoni M, Delhez R. Line broadening analysis using integral breadth methods: a critical review. J Appl Crystallogr. 2004 Jun 1;37(3):381–90.
Amidon GL, Lee PI, Topp EM. Transport processes in pharmaceutical systems. Drugs and the pharmaceutical sciences Vol.102. New York: Marcel Dekker, Inc.; 1999.
Ruell J, Tsinman O, Avdeef A. Acid-Base Cosolvent method for determining aqueous permeability of amiodarone, Itraconazole, tamoxifen, Terfenadine and other very insoluble molecules. Chem Pharm Bull. 2004;52(5):561–5.
Avdeef A. Leakiness and size exclusion of Paracellular channels in cultured epithelial cell monolayers–Interlaboratory comparison. Pharm Res. 2010;27(3):480–9.
Stewart A, Grass M, Brodeur T, Goodwin A, Morgen M, Friesen D, et al. Impact of drug-rich colloids of Itraconazole and HPMCAS on membrane flux in vitro and oral bioavailability in rats. Mol Pharm. 2017;14(7):2437–49.
Glomme A, März J, Dressman JB. Predicting the intestinal solubility of poorly soluble drugs. In: Testa B, Krämer SD, Wunderli-Allenspach H, Folkers G, editors. Pharmacokinetic profiling in drug research: biological, physicochemical, and computational strategies. Zürich: Verlag Helvetica Chimica Acta; 2006. p. 259–80.
Van Eerdenbrugh B, Vermant J, Martens J, Froyen L, Humbeeck J, Van den Mooter G, et al. Solubility increases associated with crystalline drug nanoparticles: methodologies and significance. Mol Pharm. 2010;7(5):1858–70.
Sugano K. Possible reduction of effective thickness of intestinal unstirred water layer by particle drifting effect. Int J Pharm. 2010;387(1–2):103–9.
Sarnes A, Kovalainen M, Häkkinen M, Laaksonen T, Laru J, Kiesvaara J, et al. Nanocrystal-based per-oral itraconazole delivery: superior in vitro dissolution enhancement versus Sporanox® is not realized in in vivo drug absorption. J Control Release. 2014;180:109–16.
Brouwers J, Geboers S, Mols R, Tack J, Augustijns P. Gastrointestinal behavior of itraconazole in humans – part 1: supersaturation from a solid dispersion and a cyclodextrin-based solution. Int J Pharm. 2017;525(1):211–7.
ACKNOWLEDGMENTS AND DISCLOSURES
Authors would like to thank Dr. Karl Box (Sirius Analytical - a Pion Company) for providing supporting experimental data for pKa measurements of Itraconazole.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tsinman, K., Tsinman, O., Lingamaneni, R. et al. Ranking Itraconazole Formulations Based on the Flux through Artificial Lipophilic Membrane. Pharm Res 35, 161 (2018). https://doi.org/10.1007/s11095-018-2440-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11095-018-2440-3