Abstract
Background
Metastases to the pituitary (MP) are uncommon, accounting for 0.4% of intracranial metastases. Through advances in neuroimaging and oncological therapies, patients with metastatic cancers are living longer and MP may be more frequent. This review aimed to investigate clinical and oncological features, treatment modalities and their effect on survival.
Methods
A systematic review was performed according to PRISMA recommendations. All cases of MP were included, excepted primary pituitary neoplasms and autopsy reports. Descriptive and survival analyses were then conducted.
Results
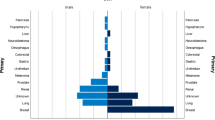
The search identified 2143 records, of which 157 were included. A total of 657 cases of MP were reported, including 334 females (50.8%). The mean ± standard deviation age was 59.1 ± 11.9 years. Lung cancer was the most frequent primary site (31.0%), followed by breast (26.2%) and kidney cancers (8.1%). Median survival from MP diagnosis was 14 months. Overall survival was significantly different between lung, breast and kidney cancers (P < .0001). Survival was impacted by radiotherapy (hazard ratio (HR) 0.49; 95% confidence interval (CI) 0.35–0.67; P < .0001) and chemotherapy (HR 0.58; 95% CI 0.36–0.92; P = .013) but not by surgery. Stereotactic radiotherapy tended to improve survival over conventional radiotherapy (HR 0.66; 95% CI 0.39–1.12; P = .065). Patients from recent studies (≥ 2010) had longer survival than others (HR 1.36; 95% CI 1.05–1.76; P = .0019).
Conclusion
This systematic review based on 657 cases helped to better identify clinical features, oncological characteristics and the effect of current therapies in patients with MP. Survival patterns were conditioned upon primary cancer histologies, the use of local radiotherapy and systemic chemotherapy, but not by surgery.



Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
Habu M, Tokimura H, Hirano H et al (2015) Pituitary metastases: current practice in Japan. J Neurosurg 123:998–1007. https://doi.org/10.3171/2014.12.JNS14870
Fassett DR, Couldwell WT (2004) Metastases to the pituitary gland. Neurosurg Focus 16:E8
He W, Chen F, Dalm B et al (2015) Metastatic involvement of the pituitary gland: a systematic review with pooled individual patient data analysis. Pituitary 18:159–168. https://doi.org/10.1007/s11102-014-0552-2
Freda PU, Post KD (1999) Differential diagnosis of sellar masses. Endocrinol Metab Clin N Am 28:81–117. https://doi.org/10.1016/S0889-8529(05)70058-X
Nelson PB, Robinson AG, Martinez JA (1987) Metastatic tumor of the pituitary gland. Neurosurgery 21:941–944. https://doi.org/10.1227/00006123-198712000-00030
Heshmati HM, Scheithauer BW, Young WF (2002) Metastases to the pituitary gland. Endocrinologist 12:45–49. https://doi.org/10.1097/00019616-200201000-00010
Zhao Y, Lian W, Xing B et al (2018) Diagnosis, therapy, and therapeutic effects in cases of pituitary metastasis. World Neurosurg 117:122–128. https://doi.org/10.1016/j.wneu.2018.05.205
Komninos J, Vlassopoulou V, Protopapa D et al (2004) Tumors metastatic to the pituitary gland: case report and literature review. J Clin Endocrinol Metab 89:574–580. https://doi.org/10.1210/jc.2003-030395
Morita A, Meyer FB, Laws ER (1998) Symptomatic pituitary metastases. J Neurosurg 89:69–73. https://doi.org/10.3171/jns.1998.89.1.0069
Iwai Y, Yamanaka K, Honda Y, Matsusaka Y (2004) Radiosurgery for pituitary metastases. Neurol Med Chir 44:112–117. https://doi.org/10.2176/nmc.44.112
Kano H, Niranjan A, Kondziolka D et al (2009) Stereotactic radiosurgery for pituitary metastases. Surg Neurol 72:248–255. https://doi.org/10.1016/j.surneu.2008.06.003
Chon H, Yoon K, Kwon DH et al (2017) Hypofractionated stereotactic radiosurgery for pituitary metastases. J Neurooncol 132:127–133. https://doi.org/10.1007/s11060-016-2346-z
Di Nunno V, Mollica V, Corcioni B et al (2018) Clinical management of a pituitary gland metastasis from clear cell renal cell carcinoma. Anticancer Drugs 29:710–715. https://doi.org/10.1097/CAD.0000000000000644
Priddy B, Hardesty DA, Beer-Furlan A et al (2017) Cerebrospinal fluid leak rhinorrhea after systemic erlotinib chemotherapy for metastatic lung cancer: a familiar problem from an unfamiliar culprit. World Neurosurg 108:992.e11–992.e14. https://doi.org/10.1016/j.wneu.2017.08.183
Liberati A, Altman DG, Tetzlaff J et al (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6:e1000100. https://doi.org/10.1371/journal.pmed.1000100
Duchen LW (1966) Metastatic carcinoma in the pituitary gland and hypothalamus. J Pathol Bacteriol 91:347–355. https://doi.org/10.1002/path.1700910208
Gsponer J, Tribolet ND, Déruaz J-P et al (1999) Diagnosis, treatment, and outcome of pituitary tumors and other abnormal intrasellar masses: retrospective analysis of 353 patients. Medicine 78:236–269. https://doi.org/10.1097/00005792-199907000-00004
Max MB, Deck MDF, Rottenberg DA (1981) Pituitary metastasis: incidence in cancer patients and clinical differentiation from pituitary adenorna. Neurology 31:998–998. https://doi.org/10.1212/WNL.31.8.998
Houck WA, Olson KB, Horton J (1970) Clinical features of tumor metastasis to the pituitary. Cancer 26:656–659. https://doi.org/10.1002/1097-0142(197009)26:3%3c656:aid-cncr2820260325%3e3.0.co;2-m
Sioutos P, Yen V, Arbit E (1996) Pituitary gland metastases. Ann Surg Oncol 3:94–99. https://doi.org/10.1007/BF02409058
Kimmel DW, O’Neill BP (1983) Systemic cancer presenting as diabetes insipidus. Clinical and radiographic features of 11 patients with a review of metastatic-induced diabetes insipidus. Cancer 52:2355–2358. https://doi.org/10.1002/1097-0142(19831215)52:12%3c2355:aid-cncr2820521232%3e3.0.co;2-j
Al-Aridi R, El Sibai K, Fu P et al (2014) Clinical and biochemical characteristic features of metastatic cancer to the sella turcica: an analytical review. Pituitary 17:575–587. https://doi.org/10.1007/s11102-013-0542-9
Schill F, Nilsson M, Olsson DS et al (2019) Pituitary metastases: a nationwide study on current characteristics with special reference to breast cancer. J Clin Endocrinol Metab 104:3379–3388. https://doi.org/10.1210/jc.2019-00012
Arafah BM, Nasrallah MP (2001) Pituitary tumors: pathophysiology, clinical manifestations and management. Endocr Relat Cancer 8:287–305
Sathananthan M, Sathananthan A, Scheithauer BW et al (2013) Sellar meningiomas: an endocrinologic perspective. Pituitary 16:182–188. https://doi.org/10.1007/s11102-012-0399-3
Byun DJ, Wolchok JD, Rosenberg LM, Girotra M (2017) Cancer immunotherapy—immune checkpoint blockade and associated endocrinopathies. Nat Rev Endocrinol 13:195–207. https://doi.org/10.1038/nrendo.2016.205
Joshi MN, Whitelaw BC, Palomar MTP et al (2016) Immune checkpoint inhibitor-related hypophysitis and endocrine dysfunction: clinical review. Clin Endocrinol 85:331–339. https://doi.org/10.1111/cen.13063
Zoli M, Mazzatenta D, Faustini-Fustini M et al (2013) Pituitary metastases: role of surgery. World Neurosurg 79:327–330. https://doi.org/10.1016/j.wneu.2012.03.018
Feiz-Erfan I, Rao G, White W, McCutcheon I (2008) Efficacy of trans-septal trans-sphenoidal surgery in correcting visual symptoms caused by hematogenous metastases to the sella and pituitary gland. Skull Base 18:077–084. https://doi.org/10.1055/s-2007-991105
Shen Z, Yang C, Bao X, Wang R (2018) Giant sellar metastasis from renal cell carcinoma: a case report and literature review. Medicine 97:e13376. https://doi.org/10.1097/MD.0000000000013376
Payandeh M, Sadeghi M, Sadeghi E (2016) The complete response to targeted drugs without surgery or radiotherapy: a case of pituitary metastasis from renal cell carcinoma. Acta Med Iran 54:617–619
Wendel C, Campitiello M, Plastino F, et al. (2017) Pituitary metastasis from renal cell carcinoma: description of a case report. Am J Case Rep 18:7–11. https://doi.org/10.12659/ajcr.901032
Castle-Kirszbaum M, Goldschlager T, Ho B et al (2018) Twelve cases of pituitary metastasis: a case series and review of the literature. Pituitary 21:463–473. https://doi.org/10.1007/s11102-018-0899-x
Gilard V, Alexandru C, Proust F et al (2016) Pituitary metastasis: is there still a place for neurosurgical treatment? J Neurooncol 126:219–224. https://doi.org/10.1007/s11060-015-1967-y
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no relevant financial relationships or conflict of interest to disclose.
Informed consent
This research did not involve humans, and no informed consent was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
11060_2020_3396_MOESM3_ESM.tiff
Supplementary Material 3: Survival analysis based on surgical technique: Biopsy versus Debulking versus Gross Total resection. N=99. (TIFF 253 kb)
11060_2020_3396_MOESM4_ESM.tiff
Supplementary Material 4: Survival analysis based on radiotherapy technique: conventional multifractional radiotherapy versus stereotactic radiotherapy. N=103. (TIFF 718 kb)
11060_2020_3396_MOESM5_ESM.tiff
Supplementary Material 5: Survival analysis based on radiotherapy technique: conventional multifractional radiotherapy versus stereotactic radiotherapy after 2010. N=36. (TIFF 674 kb)
Rights and permissions
About this article
Cite this article
Ng, S., Fomekong, F., Delabar, V. et al. Current status and treatment modalities in metastases to the pituitary: a systematic review. J Neurooncol 146, 219–227 (2020). https://doi.org/10.1007/s11060-020-03396-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-020-03396-w