Abstract
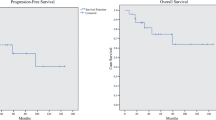
Background Infratentorial ependymoma is a common central nervous system tumor of childhood and in patients >1 year of age is treated with maximally feasible surgical resection and radiotherapy. Because of this tumor typically arises within the 4th ventricle and can invade the brainstem, patients are at risk for significant neurological impairment. Purpose To characterize the incidence, evolution, and persistence of neurologic impairment in children with infratentorial ependymoma following maximal safe surgery and conformal or intensity-modulated radiation therapy (CRT/IMRT). Patients and Methods After surgical resection, 96 children with non-metastatic infratentorial ependymoma were enrolled on a phase II study of image-guided radiation therapy and were prospectively followed with interval comprehensive neurological examinations. Late adverse neurological severity was graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events (CTCAE), version 3.0. Results The most common deficits detected at baseline examination were limb dysmetria, cranial nerve VI/VII palsy, limb paresis, dysphagia, and truncal ataxia/hypotonia. When present, gait dysfunction and dysphagia were often severe. Oculomotor dysfunction, facial paresis, dysphagia, and gait impairment improved over time. With the exception of hearing loss, in the survivor cohort, very few severe late effects (CTCAE Grade 3/4/5) were present at 60 months survival. Conclusion In general, neurological deficits were maximal in the post-operative period and either remained stable or improved during radiation and the post-treatment evaluation period. With the exception of hearing, the majority of chronic residual neurological deficits in this at-risk population are mild and only minimally intrude upon daily life.
Similar content being viewed by others
Explore related subjects
Discover the latest articles and news from researchers in related subjects, suggested using machine learning.References
CBTRUS 1/22/08. Selected primary (malignant and non-malignant) brain and central nervous system tumor age-specific incidence rates by age at diagnosis, CBTRUS 1998–2002. http://wwwcbtrusorg/2005-2006/tables/2006table12pdf Accessed 22 Jan 2008
Gurney JGSM, Bunin GR (1999) CNS and miscellaneous intracranial and intraspinal neoplasms. National Cancer Institute, SEER Program, Bethesda, MD. NIH Pub. No. 99-4649 Report
Bouffet E, Perilongo G, Canete A et al (1998) Intracranial ependymomas in children: a critical review of prognostic factors and a plea for cooperation. Med Pediatr Oncol 30(6):319–329. doi:10.1002/(SICI)1096-911X(199806)30:6<319::AID-MPO1>3.0.CO;2-H (discussion 329–331)
Phase A II trial of conformal rt for pediatric patients with localized ependymoma, chemotherapy prior to 2nd surgery for incompletely resected ependymoma and observations for completely resected, differentiated, supratentorial ependymoma. https://members.childrensoncologygroup.org/prot/ProtInfo.asp?ProtocolNum=ACNS0121&Disease=CNS. Children’s Oncology Group Accessed
Merchant TE, Mulhern RK, Krasin MJ et al (2004) Preliminary results from a phase II trial of conformal radiation therapy and evaluation of radiation-related CNS effects for pediatric patients with localized ependymoma. J Clin Oncol 22(15):3156–3162. doi:10.1200/JCO.2004.11.142
Littell RCMG, Stroup WW, Wolfinger RD (1996) SAS system for mixed models. SAS Institute Inc, Cary, NC
Liang H (2006) A new method of evaluating antitumor activity from measured tumor volumes. Contemp Clin Trials 27(3):269–273. doi:10.1016/j.cct.2005.11.004
Spunt SL, Sweeney TA, Hudson MM et al (2005) Late effects of pelvic rhabdomyosarcoma and its treatment in female survivors. J Clin Oncol 23(28):7143–7151. doi:10.1200/JCO.2005.12.096
Oeffinger KC, Mertens AC, Sklar CA et al (2006) Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 355(15):1572–1582. doi:10.1056/NEJMsa060185
Hua C, Bass JK, Khan R et al (2008) Hearing loss after radiotherapy for pediatric brain tumors: effect of cochlear dose. Int J Radiat Oncol Biol Phys 72(3):892–899
Hawkins MM, Kingston JE, Kinnier Wilson LM (1990) Late deaths after treatment for childhood cancer. Arch Dis Child 65(12):1356–1363. doi:10.1136/adc.65.12.1356
Mertens AC, Yasui Y, Neglia JP et al (2001) Late mortality experience in five-year survivors of childhood and adolescent cancer: the childhood cancer survivor study. J Clin Oncol 19(13):3163–3172
Packer RJ, Gurney JG, Punyko JA et al (2003) Long-term neurologic and neurosensory sequelae in adult survivors of a childhood brain tumor: childhood cancer survivor study. J Clin Oncol 21(17):3255–3261. doi:10.1200/JCO.2003.01.202
Bamford FN, Jones PM, Pearson D et al (1976) Residual disabilities in children treated for intracranial space-occupying lesions. Cancer 37(2 (Suppl)):1149–1151. doi:10.1002/1097-0142(197602)37:2+<1149::AID-CNCR2820370825>3.0.CO;2-C
Butler DF, Jose BO, Paris KJ et al (1999) An analysis of the late effects of radiotherapy in pediatric central nervous system tumors. J Ky Med Assoc 97(10):465–471
Chapman CA, Waber DP, Bernstein JH et al (1995) Neurobehavioral and neurologic outcome in long-term survivors of posterior fossa brain tumors: role of age and perioperative factors. J Child Neurol 10(3):209–212. doi:10.1177/088307389501000308
Foreman NK, Faestel PM, Pearson J et al (1999) Health status in 52 long-term survivors of pediatric brain tumors. J Neurooncol 41(1):47–53. doi:10.1023/A:1006145724500
Lannering B, Marky I, Lundberg A et al (1990) Long-term sequelae after pediatric brain tumors: their effect on disability and quality of life. Med Pediatr Oncol 18(4):304–310. doi:10.1002/mpo.2950180410
Macedoni-Luksic M, Jereb B, Todorovski L (2003) Long-term sequelae in children treated for brain tumors: impairments, disability, and handicap. Pediatr Hematol Oncol 20(2):89–101. doi:10.1080/0880010390158595
Sonderkaer S, Schmiegelow M, Carstensen H et al (2003) Long-term neurological outcome of childhood brain tumors treated by surgery only. J Clin Oncol 21(7):1347–1351. doi:10.1200/JCO.2003.08.009
Spunberg JJ, Chang CH, Goldman M et al (1981) Quality of long-term survival following irradiation for intracranial tumors in children under the age of two. Int J Radiat Oncol Biol Phys 7(6):727–736
Syndikus I, Tait D, Ashley S et al (1994) Long-term follow-up of young children with brain tumors after irradiation. Int J Radiat Oncol Biol Phys 30(4):781–787
Acknowledgements
Financial Support: This work was supported by the Cancer Center Support (CORE) Grant P30 CA 21765 from the National Institutes of Health and by the American Lebanese Syrian Associated Charities (ALSAC).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Brannon Morris, E., Li, C., Khan, R.B. et al. Evolution of neurological impairment in pediatric infratentorial ependymoma patients. J Neurooncol 94, 391–398 (2009). https://doi.org/10.1007/s11060-009-9866-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11060-009-9866-8