Abstract
Malassezia pachydermatis is part of the normal skin microbiota of various animal species but under certain circumstances becomes an opportunistic pathogen producing otitis and dermatitis. Commonly these Malassezia diseases are effectively treated using azoles. However, some cases of treatment failure have been reported. Alterations in the ERG11 gene have been associated with in vitro azole resistance in M. pachydermatis. In the present study, in vitro antifungal susceptibility of 89 different strains of M. pachydermatis isolated from different animal species and health status was studied. The susceptibility to fluconazole (FLZ), itraconazole (ITZ), ketoconazole and amphotericin B was tested by a disk diffusion method and 17 strains were also subjected to an ITZ E-test. Mueller–Hinton supplemented with 2% glucose and methylene blue was used as culture medium in both susceptibility assays. Multilocus sequence typing was performed in 30 selected strains using D1D2, ITS, CHS2 and β-tubulin genes. Also, ERG11 gene was sequenced. The four antifungals tested were highly effective against most of the strains. Only two strains showed no inhibition zone to antifungals and a strain showed an increased MIC to ITZ. The study of the ERG11 sequences revealed a high diversity of DNA sequences and a total of 23 amino acid substitutions, from which only two have been previously described. Also, three deleterious substitutions (A302T, G459D and G461D) previously associated with azole resistance in this yeast were recovered. A correlation between certain genotypes and ERG11 mutations was observed. Some of the ERG11 mutations recovered were correlated with a reduced susceptibility to azoles.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malassezia pachydermatis is a lipophilic yeast that belongs to the normal skin microbiota of various animal species and colonizes the skin and mucosal sites of healthy dogs. Although M. pachydermatis has been considered classically the only non-lipid-dependent species of the genus Malassezia, they also lack the genes coding for a fatty acid synthase and thus, are unable to synthetize long-chained fatty acids (C14 or C16) de novo [1, 2]. Malassezia pachydermatis can utilize lipid fractions within the peptone component of SGA, thus they also need a few lipids to be able to grow [2,3,4].
Despite being part of the microbiota, Malassezia may act as an opportunistic pathogen under certain circumstances that allow the overgrowth of the yeast population. Malassezia pachydermatis is a common responsible agent of otitis and dermatitis in dogs [5, 6]. In humans, it has also been reported to produce systemic infections particularly in neonates and immunocompromised patients receiving parenteral nutrition [7]. The treatment of Malassezia diseases is currently based on the use of topical and systemic antifungal therapy. Topical agents include chlorhexidine, clotrimazole, enilconazole, ketoconazole, miconazole and nystatin that can be used in various forms such as shampoos, sprays, or ointments [8]. Azoles like ketoconazole (KTZ) or itraconazole (ITZ) are commonly used as systemic agents for the treatment of Malassezia dermatitis and otitis. Fluconazole (FLZ) can be used for the treatment of Malassezia skin diseases like seborrheic dermatitis [9, 10]. Amphotericin B (AMB) and liposomal amphotericin B are indicated in the treatment of systemic cases of Malassezia in humans [8, 11].
The Clinical and Laboratory Standards Institute (CLSI) developed in 2002 a reference broth microdilution method for evaluating the susceptibility of Candida spp. and Cryptococcus neoformans [12]. This method is inapplicable to the genus Malassezia because of their lipid-dependency, their slower growth rate and tendency to form clusters [13, 14]. Thus, it has been subsequently adapted to Malassezia by various researchers modifying the media, time of incubation and inoculum but it has not been yet standardized [13, 15,16,17]. Also, disk diffusion method and the E-test gradient have been adapted to evaluate the susceptibility of Malassezia against antifungal compounds [14, 18].
Although antimicrobial resistance is a global serious threat to human and animal health, recent studies have showed that most wild-type Malassezia yeast remain susceptible to the most used azoles such as KTZ, ITZ and miconazole but the efficacy of FLZ is variable [8, 11, 19]. Some sporadic reports of therapeutic failure with azoles in canine M. pachydermatis dermatitis associated with increased tolerance to azoles in vitro might reflect the chronic and relapsing course of Malassezia diseases that often need frequent and lengthy treatments [16, 20,21,22,23].
There are various mechanisms of azole antifungal resistance in Malassezia species. The drug efflux pump is associated to azole resistance in M. pachydermatis [14, 25]. Mutations in the coding region of the ERG11 gene, encoding a lanosterol 14α-demethylase, which is the target enzyme of azole antifungals, are considered a mechanism of resistance [26,27,28]. Kim et al. [29] demonstrated that tandem quadruplication of the genomic region of the ERG11 gene contributes to azole resistance in M. pachydermatis. At the present, only two M. pachydermatis strains have demonstrated to be resistant to azoles. The strains were isolated in Japan [23] and Italy [22]. Both isolates showed high minimum inhibitory concentrations (MICs) against azoles but only in one case this resistance was linked to ERG11 mutations [23]. Although some mutations have been detected in this gene, its intrinsic diversity in M. pachydermatis yeasts, that are mainly susceptible to antifungals, is yet unknown.
Even though there is not a reference method for susceptibility testing of M. pachydermatis available yet, on this study we evaluate the susceptibility of different strains of this yeast against three different azoles (FLZ, ITZ, and KTZ) and AMB. We included a wide variety of strains recovered from different animal species with different health status and collected over different years. Also, we study the genetic variability of ERG11 gene in these strains. Gene mutations and antifungal susceptibility testing results was investigated.
Materials and Methods
Strains
A total of 89 strains of M. pachydermatis (Table S1) were selected from our culture collection for susceptibility testing. Strains were isolated between 1994 and 2021 and included different animal species: dog (n = 73), cat (n = 12), pig (n = 1), cow (n = 1), goat (n = 1), and horse (n = 1). The M. pachydermatis neotype strain CBS1879 was also included. The strains were stored at − 80 ºC [24].
The 73 strains of dogs included four strains isolated from healthy dogs, eight strains from dogs with dermatitis, 59 from dogs with otitis externa and two from otitis media. According to the data provided by the clinicians when sending the samples, the strains from otitis externa were classified into chronic otitis externa (lasting more than three months, n = 25), acute otitis externa (lasting less than six weeks, n = 17), purulent otitis externa (n = 6) and recurrent otitis externa (n = 4). The strains isolated from cats included five strains recovered from cats with dermatitis and six strains from animals with otitis, from which two were otitis media and four otitis externa. The strains from otitis externa were classified into acute otitis externa (n = 2), chronic otitis externa (n = 1) and purulent otitis externa (n = 1). One strain from a healthy cat was also included. The strains from cow, horse, pig, and goat were all obtained from healthy animals.
Susceptibility Testing
Four different antifungals were selected for susceptibility testing: amphotericin B (AMB), fluconazole (FLZ), itraconazole (ITZ) and ketoconazole (KTZ). Susceptibility of the strains was tested by a disk diffusion method. For the disk diffusion method, two stock inoculum suspensions were prepared from 3-day old cultures on SGA (Oxoid) at 35ºC from each strain. The stock inoculum suspensions were performed in 3 mL of distilled water supplemented with 0.004% Tween 80 to reduce clump formation and were adjusted to a density of 1 McFarland standards (3 × 108 CFU/ml). Mueller–Hinton supplemented with 2% glucose and 0.5 mg/l methylene blue (MH-GM) was the media selected for the disk diffusion method [13, 30]. For each suspension tube, 5 plates of the media were streaked using a sterile cotton swab dipped into the inoculum suspension. One of the plates was a growth control and on the remaining four, one disk of antifungal per plate was placed. Two commercial antifungal disks were used comprising AMB, FLZ, ITZ and KTZ (Neo-Sensitabs, Rosco) at concentrations of 10, 25, 10 and 15 µg/disk respectively and FLZ, KTZ and AMB (Bio-Rad) at concentrations of 25, 50 and 100 µg/disk, respectively. Plates were then incubated at 35ºC, and inhibition zone sizes were measured at 48, 72 and 96 h. The inhibition zone diameter was determined after incubating at 35ºC for 72 h. Candida parapsilopsis ATCC 90,028 and Pichia kundriavzevii ATCC 6258 were included as quality control strains in both disk diffusion tests.
The interpretative criterion was according to the manufacturer’s guidelines for yeasts, as shown in Table 1.
Susceptibility against ITZ was also studied using the E-test method on 17 out of the 89 strains. The 17 strains were selected based on their diverse response to antifungals by disk diffusion method, but also different animal species were included. The strain selection included strains obtained from healthy animals (n = 7), from animals with otitis externa (n = 8) and animals with dermatitis (n = 2). Also, the M. pachydermatis neotype strain CBS1879 was included. E-test was performed under the same conditions that the disk diffusion method. One E-test gradient stripe for ITZ (Biomérieux) was placed on each plate. The plates were then incubated at 35ºC and examined at 48, 72 and 96 h. The MICs were determined after 72 h of incubation. Also, some strains were evaluated using SGA supplemented with 1% Tween 80 [23] to compare the results obtained.
ERG11 Gene Amplification and Sequencing
A total of 31 strains were selected to sequence their ERG11 gene, including the neotype strain of M. pachydermatis CBS1879 and the 17 strains evaluated by E-test. The strains selected included different animal species, dog (n = 23), cat (n = 4), pig (n = 1), horse (n = 1), goat (n = 1) and cow (n = 1). These strains were recovered from nine healthy animals, 17 animals with otitis externa, one animal with otitis media and four animals with dermatitis. The strains were selected based on their susceptibility results against the four antifungals tested. Strains without an inhibition zone, a reduced inhibition zone in the disk diffusion method and a high MIC to ITZ were included. Also, strains with wider inhibition zone diameters were included.
The DNA was extracted directly from 5-day-old cultures grown in SGA according to the FastDNA Spin kit protocol (MP Bio-medicals, Biolink, Barcelona, Spain). The ERG11 gene was amplified using the primers pairs MALAERG1S/R, MALAERG2S/R, MALAERG3S/R, MALAERG4S/R described by Kano et al. [23]. Reaction mixtures contained 5.0 μl of template DNA, 5.0 μl of 10 × PCR buffer, 0.2 mM of each dNTP, 1.5 mM MgCl2, 0.2 μM each primer and 1.25 U of Taq polymerase in a final volume of 50 μl. The amplification process consisted of a pre-denaturation step at 95 ºC for 10 min, followed by 35 cycles of denaturation at 95 ºC /15 s, annealing at 55 ºC /30 s and extension at 72 ºC /1 min, and a final extension of 5 min at 72 ºC. Both strands of purified gene fragments were sequenced with BigDye Terminator v3.1. cycle sequencing kit (Applied Biosystems) on an Applied Biosystems 3730 DNA Analyzer (Applied Biosystems). Sequence alignments were carried out using Clustal X v2.0.12. software [31]. The PROVEAN software [32] was used to study the effect on the protein of the amino acid substitutions.
Maximum likelihood analysis of the ERG11 sequences was conducted using MEGA 11 software [33] with 1,000 bootstrap replicates. Clades that were supported by bootstrap values of ≥ 70% were regarded as strongly supported.
Multilocus Sequences Typing
The strains selected for ERG11 gene sequencing were also chosen for a multilocus sequence typing system based on four target regions (D1/D2 region of the 26S rRNA gene, the ITS-5.8S rRNA gene, the β-tubulin gene and the CHS2 gene).
Sequences of the four genes of 16 strains had been characterized previously [34]. The four genes of 15 remaining strains were amplified and sequenced as described previously [35]. To illustrate the phylogenetic relatedness between our strains a minimum spanning tree was constructed using the PHYLOViZ 2.0 software [36]. Each genotype cluster was identified by using the goeBURST algorithm version.
Statistical Analysis
Statistical analyses were conducted by Minitab 17 Statistical software (Minitab). The results of both dilutions of each strain were compared using the Student’s t-test. To compare the means of inhibition zone diameter between strains obtained from healthy animals and strains obtained from animals with dermatitis/otitis the ANOVA test was used.
Results
Susceptibility Testing
All the strains tested showed growth on the media selected (MH-GM). Susceptibility results were determined after 72 h of incubation at 35ºC, since it was the optimal time of growth for all the strains included. At 48 h not all the strains had growth and no differences were observed between inhibition zone diameters at 72 and 96 h. The results of both disk diffusion methods at 72 h are summarized in Table 2. No significant differences were observed between both dilutions of each strain (P > 0.05).
In general, according to the manufacturer’s breakpoints for yeasts, the four antifungals tested were active against most of the strains regardless of their origin. However, a few exceptions were observed. With Rosco antifungal disks, five strains were classified as susceptible dose dependent (SDD) and five as resistant (R) to FLZ. One strain was classified as R to KTZ, one as SDD to ITZ, and four as SDD and one as R to AMB. One strain (MA165) was classified as R to ITZ, KTZ and AMB, and one strain (MA1386) was classified as R to FLZ and SDD to AMB. With Bio-Rad antifungal disks, four strains were classified as SDD and seven as R to FLZ. These strains were recovered from animals with chronic otitis externa or dermatitis. All strains recovered from healthy animals were classified as susceptible according to the manufacturer’s breakpoints for yeasts. Strain MA1429, isolated from a dog with dermatitis, showed the complete absence of inhibition zone to FLZ and strain MA165, isolated from a dog with chronic otitis externa, showed no inhibition zone to AMB.
No differences were observed in the inhibition zone diameters between strains recovered from healthy animals and strains from animals with otitis or dermatitis except for the KTZ Bio-Rad antifungal disks (Table 2). Strains recovered from chronic otitis externa and otitis media showed smaller inhibition diameters to KTZ than strains from purulent and acute otitis externa (P = 0.010).
Most of the strains selected for the E-test method using MH-GM as culture medium, showed MICs between 0.002 and 0.003 µg/ml to ITZ (Table 3). The only exception was strain MA1716 that showed a MIC of 0.125 µg/ml (Fig. 1). This strain was also tested using SGA supplemented with 1% Tween 80 and a MIC of 8-12 µg/ml was obtained. The neotype strain CBS 1879 showed a MIC of 0.002 µg/ml and 0.38 µg/ml in MH-GM and SGA + 1% Tween 80, respectively.
ERG11 Sequence
Amplification of the complete ERG11 gene and screening for amino acid substitutions was performed for each of the 31 strains (Table 3). The ERG11 sequence included 1623 bp. The sequences of the strains shared 96.0–100% sequence similarity to M. pachydermatis neotype strain CBS1879 and were clustered into 21 different genetic types. Representative nucleotide sequences of the different genetic types determined in this study have been deposited at the GenBank database under accession numbers ON814677- ON814697.
Of the 31 strains of M. pachydermatis, seven of them belonged to the genetic type I, including the neotype strain CBS1879. All strains of genetic type I were isolated from healthy animals except two (MA195 and CBS1879). Genetic type II included three strains recovered from different animal species and genetic type XIV included three strains recovered from dogs with otitis. The rest of genetic types were unique for each strain.
The predicted ERG11 amino acid sequences consisted of 540 amino acids. Some silent polymorphisms were identified, and comparison of the deduced amino acid sequences revealed 14 unique amino acid sequence types. Strains belonging to genetic type I had no amino acid substitution. Strains from genetic type II and XI showed the same amino acid sequence with one amino acid substitution (E181Q). Strains from genetic type IV and VIII showed the same amino acid sequence with three substitutions (I25V, E181Q, and T354I). Strains from genetic type X, XIII and XIX showed the same amino acid sequence with nine substitutions (I25S, W52L, R84K, L86F, E181Q, N212S, S226L, E290D, Y352F, H399R). Strains from genetic type VI, VII, XIV and XV showed the same amino acid sequence with five substitutions (A17T, R84K, R175H, Q178R, and E181Q). The number of amino acid substitutions of the rest of genetic types varied between the strains and ranged from 2 to 11 substitutions per strain. A total of 23 amino acid substitutions were identified. Fourteen amino acid substitutions were considered as neutral: A17T, I25V, I25S, V33I, R84K, L86F, D166E, R175H, Q178R, E181Q, N212S, E290D, T354I, H399R, D405N. All these mutations were recovered from strains isolated from different animal species and health status. Nine amino acid substitutions were considered as deleterious substitutions (W52L, F143S, R202H, S226L, A302T, A306S, Y352F, G459D, G461D) and were recovered from strains isolated mainly from dogs with otitis or dermatitis. Mutations A302T, G459D were detected in strain MA1716 with a MIC of 0.125 µg/ml and mutations W52L, A306S, Y352F, and G461D were detected in strain MA1429 with no inhibition zone to FLZ.
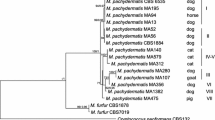
Maximum likelihood analysis of the ERG11 gene is shown in Fig. 2. All M. pachydermatis sequences grouped in a supported clade. The strains were grouped in three different subclades. Subclade I (94% bootstrap) grouped strains from healthy animals and animals with otitis or dermatitis. Subclade II (96% bootstrap) grouped mainly strains isolated from dogs with otitis and dermatitis and one strain from a healthy goat. A third subclade, subclade III (81% bootstrap) grouped strains isolated from dogs with otitis and one strain from a healthy pig.
Molecular phylogenetic tree inferred from maximum likelihood analysis of ERG11 sequences of M. pachydermatis strains. Bootstrap values > 70% in 1,000 replications are shown at the nodes. Sequences of Cryptococcus neoformans, Candida albicans, Candida tropicalis and Saccharomyces cerevisiae were selected as outgroup for the tree construction
Multilocus Sequence Typing
Sequence types obtained for each gene are listed in Supplementary Table S2. Six different sequence types of D1/D2 region were recovered, five from them were previously described and one is new from this study (VI). Eleven out of the 30 strains (36.66%) had sequence type I which was the most abundant. Strains from healthy animals only showed sequence types I or II.
The ITS 5.8S rRNA was successfully amplified and sequenced. Fifteen different sequence types were recovered from which four were new (XIV, XV, XVI and XVII). Ten strains had one of the new ITS sequence types. The sequence type I was the majority (n = 5; 16.6%) and was recovered from strains from dogs.
Ten different sequence types of β-tubulin were recovered from which two were new ones (X and XI). Sequence type VIII was the most abundant and was recovered from eight strains (26%) isolated from dogs with otitis or dermatitis.
Regarding CHS2 gene, nine different sequence types were recovered in total, and all of them have been described previously. Sequence type I was majority and was obtained from a total of nine strains (30%) of dogs (n = 6), horse (n = 1), cat (n = 1) and cow (n = 1).
The sequences obtained in this study have been deposited at the GenBank database under accession numbers ON787824 (D1D2), ON791562-ON791565 (ITS), and ON814675- ON814676 (β-tubulin).
When the four loci (D1D2, ITS, CHS2 and β-tubulin) were combined, a total of 25 genotypes were identified. Among all genotypes, 22 were only found once. Two genotypes were shared by two strains, and one genotype was shared by five strains. When the presence of amino acid substitutions was considered, the graphing algorithm analysis revealed small clusters of ERG11-mutated isolates. As shown in Fig. 3, a cluster of 12 strains of 10 different genotypes (I) with a few amino acid substitutions (0–3) was observed. All the strains within this group showed wide inhibition diameters to azoles except for one strain (MA1716) with a small inhibition diameter to FLZ and a higher MIC to ITZ. A second cluster (II) included seven strains of seven different genotypes with five to 11 amino acid mutations. One strain within this cluster (MA1429) showed no inhibition zone to FLZ. Also, a third cluster (III) of seven strains of three different genotypes was obtained with five to six amino acid substitutions. One strain was considered as R to KTZ and SDD to ITZ, and two strains were considered SDD to FLZ.
Minimum spanning trees using the goeBURST algorithm of 31 Malassezia pachydermatis strains based on analysis of the four loci used for genotyping. Each circle represents a unique genotype. The diameter of each circle corresponds to the number of isolates sharing the same genotype and the numbers within circles represent strain number. The color of the circle is related to the presence of amino acid substitutions in ERG11: black for strains with 6 to 11 amino acid substitutions, dark gray for strains with 4 to 5 amino acid substitutions, light gray for strains with 1 to 3 amino acid substitutions and white for strains without any amino acid substitution
Discussion
Antifungal susceptibility testing for M. pachydermatis must be interpreted with caution neither breakpoints nor a reference method have been yet stablished for this yeast species. This means that any classification of the strains into susceptible, intermediate, and resistant remains speculative. However, according to the manufacturer’s breakpoints available for yeasts the four antifungals tested in our study were active against most of the strains selected. Only one strain in our study showed an increased MIC to ITZ. As reported by some authors [8, 16, 37, 38], M. pachydermatis is highly susceptible to KTZ and ITZ which is consistent with the results observed in our study. Since now, only two M. pachydermatis isolates have demonstrated to be resistant to both ITZ and KTZ [22, 23]. In our study, only one strain showed no inhibition zone to FLZ. Fluconazole consistently returns significantly higher MICs when compared to other antifungals tested among studies with M. pachydermatis [17, 39, 40]. It has been demonstrated that M. pachydermatis isolates can become resistant during treatment with FLZ by inducing resistance in vitro to this antifungal [41]. Thus, the clinical utility of this azole in dogs and cats is questionable [8, 42]. Bernardo et al. [43] found a M. pachydermatis isolate resistant to AMB. However, due to the potential toxicity of AMB its use in veterinary medicine is limited to serious progressive or disseminated systemic mycoses [8].
In our study, all the strains with a reduced inhibition zone or no inhibition zone were recovered from animals with otitis and/or dermatitis. These results agree with the ones obtained in three different studies where the MICs of various antifungals agents were higher for isolates from animals with otitis/dermatitis [21, 38, 44]. Also, in our study, differences were observed in the inhibition diameters between strains from chronic otitis externa and otitis media, and strains from purulent and acute otitis externa. The mean inhibition diameters to KTZ were higher in the strains from acute and purulent otitis externa. A study by Chiavassa et al. [20] compared the MIC values of two different antifungal agents between isolates of M. pachydermatis from chronic otitis and acute otitis externa. The results showed that the isolates from chronic otitis externa had MIC values higher than the isolates from acute otitis externa. It was hypothesized that those increased MICs were a result to the exposure of isolates to antifungal agents. In our study, strains MA1716, with an increased MIC to ITZ, and MA1429, with complete absence of inhibition zone to FLZ, were recovered from dogs with previous antifungal treatments with ITZ and miconazole, respectively.
In the E-test method, only one strain (MA1716) showed higher MICs in MH-GM and SGA + 1% Tween 80 and thus, could be considered to have a reduced susceptibility against ITZ. An increase of 64-fold of the MIC was observed when the media used was SGA with lipid supplementation. This increase in MIC values when the culture medium has a lipid supplementation was also observed in M. pachydermatis CBS1879 (Fig. 1). This medium was also used to assess susceptibility to ITZ and KTZ by the E-test technique [23]. Different testing variables are known to have an impact on in vitro determinations as lipid supplementation enhancing the yeast growth [8, 45]. Thus, the isolates could appear to be susceptible or resistant only by modifying test conditions. Due to this, it is essential to establish a set of standardized criteria for in vitro susceptibility testing of Malassezia spp. [14, 46].
Mutations of the ERG11 gene could reduce the susceptibility of fungi to azoles [26,27,28, 47,48,49]. In our study, a high variability of this gene was observed. Sequence differences in the ERG11 gene among strains ranged from 0.1 to 4.0%, which is greater than those described with CHS2 (1.9 to 3.4%) or β-tubulin (0.3 to 3.4%) [34]. Indeed, only 6 of the strains displayed the sequence of the M. pachydermatis neotype strain CBS1879. This strain has been previously used as comparison to detect possible amino acid mutations [23]. The analysis of the ERG11 gene grouped M. pachydermatis strains in three different clades. This aggrupation correlates quite well with the groups defined by multilocus sequencing.
Even though many polymorphisms were observed, not all lead into amino acid substitutions. Our data clearly show that in M. pachydermatis point mutations leading to amino acid changes are a frequent event in ERG11 gene. A total of 23 different amino acid substitutions were recovered from which nine were deleterious substitutions. The analysis of multilocus groups using ERG11 amino acid substitutions as discriminant parameter revealed some closely related genotypes carrying more amino acid substitutions. This suggested a correlation between certain genotypes of M. pachydermatis and in vitro susceptibility results, in agreement with other authors [38, 50].
Of the amino acid substitutions identified, only two (G459D, G461D) have been reported previously in M. pachydermatis associated with azole resistance [51, 52]. One of the mutations present in our study, G461D, recovered from a strain with no inhibition zone to FLZ, was also observed in a clinical isolate with in vitro resistance to ravuconazole [51].
The other mutation, G459D, was reported in miconazole tolerant clones of the CBS1879, selected by serial passage on miconazole supplemented media [52]. This mutation was also present in a strain (MA1716) with a higher MIC to ITZ and with a reduced inhibition zone to FLZ in our study. This strain also showed a mutation at point A302T. This point mutation but with a different amino acid change (A302V) has been described by Kano et al. [23] in an isolate with proven in vitro resistance to ITZ and KTZ. The different amino acid change could explain the results obtained in susceptibility testing of our strain. Another point mutation described by Kano et al. [23] and associated with azole resistance, M138V, was not detected in our study.
Point mutations of the ERG11 gene leading to amino acid substitutions that induce antifungal resistance have also been observed in other Malassezia species [47, 53]. In M. furfur a point mutation Y67F (130 in M. pachydermatis) is associated with fluconazole resistance [53]. In M. globosa three-point mutations Y127F, A169S and K176N (synonymous with 130, 172 and 179 in M. pachydermatis) are associated with azole resistance [47]. However, none of these point mutations were observed in the strains of this study.
Some of the amino acid substitutions observed in our study had been described in other fungal species associated to a reduced antifungal susceptibility. In Candida albicans, point mutations at positions 54, 145, 226 and 307 (synonymous with 52, 143, 202, and 226 in M. pachydermatis, respectively) were associated with a reduced azole susceptibility [54,55,56,57]. These point mutations are deleterious in M. pachydermatis and were observed in our study in some strains. Also, the presence of two amino acid substitutions in combination G307S + G450E in C. albicans was reported to increase by 16-fold the MICs to FLZ [56]. This combination is synonymous with the combination A306S + G461D in M. pachydermatis observed in one strain of our study (MA1429) with a disk diffusion with no inhibition zone to FLZ.
The relationship between ERG11 amino acid mutations and drug resistance has been reported in many pathogenic fungi such as Aspergillus fumigatus, Candida spp. and Cryptococcus spp. [58]. This is not the case of M. pachydermatis. Since now, few strains of M. pachydermatis have demonstrated to be resistant to azoles and only four amino acid mutations in ERG11 have been described [23, 51, 52]. None of these substitutions have been confirmed to cause azole resistance using in vitro experiments and it’s not known which part of the protein is involved probably because there is no experimentally determined three-dimensional structure of the ERG11 protein available. Based on the three-dimensional structure of C. albicans ERG11, the mutations G448D and G450D in C. albicans (synonymous with G459D and G461D in M. pachydermatis) are located near the heme-binding site and near the end of helix I of the protein, respectively [59, 60]. Also, mutation F145L (synonymous with F143S in M. pachydermatis) is located near the substrate channel [60]. Based on the three-dimensional structure of C. neoformans CYP51, residues A317 and F158 in C. neoformans (synonymous with A306S and F143S in M. pachydermatis, respectively) are in the heme binding site and mutation A313 in C. neoformans (A302T in M. pachydermatis) is part of one of the active site cavities [61]. However, the possibility that other deleterious substitutions, which are located outside of the active side, may also contribute to fungal resistance via other structural changes cannot be ruled out.
The presence or absence of amino acid substitutions may not be the solely cause of antifungal resistance [25, 55]. Other mechanisms of resistance against azoles have been suggested in M. pachydermatis as efflux pumps [14, 25]. Other possibility for these reduced susceptibilities is a chromosomal rearrangement that leads to an overexpression of the ERG11 and ERG4 genes. Kim et al. [29] found a tandemly quadruplicated region in chromosome 4 of two M. pachydermatis isolates with high in vitro MICs of KTZ. Thus, an overexpression of this region was observed that could be responsible of the higher MIC.
In conclusion, this study highlights the high diversity of sequences in ERG11 gene, the primary target of azole antifungal drugs. This high diversity could be part of the high intrinsic variability of this gene in M. pachydermatis. Even though we found three mutations that were already reported, we also found some new mutations. Also, genotyping revealed small clusters of ERG11-mutate isolates. Although some mutant strains showed a reduced susceptibility to some antifungals, further studies would be necessary to completely understand the role of these mutations in the susceptibility against antifungal agents.
References
Xu J, Saunders CW, Hu P, et al. Dandruff-associated Malassezia genomes reveal convergent and divergent virulence traits shared with plant and human fungal pathogens. Proc Natl Acad Sci USA. 2007;104:18730–5.
Wu G, Zhao H, Li C, et al. Genus-wide comparative genomics of Malassezia delineates its phylogeny, physiology, and niche adaptation on human skin. PLoS Genet. 2015;11:1–26.
Puig L, Bragulat MR, Castellá G, Cabañes FJ. Characterization of the species Malassezia pachydermatis and re-evaluation of its lipid dependence using a synthetic agar medium. PLoS ONE. 2017;12: e0179148.
Cabañes FJ. Malassezia pachydermatis: to be, or not to be lipid-dependent. Rev Iberoam Micol. 2020;37:3–4.
Chen TA, Hill PB. The biology of Malassezia organisms and their ability to induce immune responses and skin disease. Vet Dermatol. 2005;16:4–26.
Bond R. Superficial veterinary mycoses. Clin Dermatol. 2010;28:226–36.
Velegraki A, Cafarchia C, Gaitanis G, Iatta R, Boekhout T. Malassezia infections in humans and animals: pathophysiology, detection, and treatment. PLoS Pathog. 2015;11: e1004523.
Bond R, Morris DO, Guillot J, et al. Biology, diagnosis and treatment of Malassezia dermatitis in dogs and cats Clinical Consensus Guidelines of the World Association for Veterinary Dermatology. Vet Dermatol. 2020;31:28–74.
Zisova LG. Fluconazole and its place in the treatment of seborrheic dermatitis, new therapeutic possibilities. Folia Med (Plovdiv). 2006;48:39–45.
Alizadeh N, Monadi Nori H, Golchi J, Eshkevari SS, Kazemnejad E, Darjani A. Comparison the efficacy of fluconazole and terbinafine in patients with moderate to severe seborrheic dermatitis. Dermatol Res Pract. 2014;2014: 705402.
Schlemmer KB, de Jesus FPK, Loreto ES, Farias JB, Alves SH, Ferreiro L, Santurio JM. In vitro combination of antifungal agents against Malassezia pachydermatis. Med Mycol. 2019;57:324–7.
Clinical Laboratory and Standards Institute. Reference method for broth dilution antifungal susceptibility testing of yeasts. Approved standards, 3rd edn, document M27-A3. Wayne, PA: Clinical Laboratory and Standards Institute. 2008.
Peano A, Pasquetti M, Tizzani P, Chiavassa E, Guillot J, Johnson E. Methodological issues in antifungal susceptibility testing of Malassezia pachydermatis. J Fungi. 2017;3:37.
Peano A, Johnson E, Chiavassa E, Tizzani P, Guillot J, Pasquetti M. Antifungal resistance regarding Malassezia pachydermatis: where are we now? J Fungi. 2020;6:93.
Velegraki A, Alexopoulos EC, Kritikou S, Gaitanis G. Use of fatty acid RPMI 1640 media for testing susceptibilities of eight Malassezia species to the new triazole posaconazole and to six established antifungal agents by a modified NCCLS M27–A2 microdilution method and Etest. J Clin Microbiol. 2004;242:3589–93.
Nijima M, Kano R, Nagata M, Hasegawa A, Kamata H. An azole-resistant isolate of Malassezia pachydermatis. Vet Microbiol. 2011;149:288–90.
Cafarchia C, Figueredo LA, Favuzzi V, et al. Assessment of the antifungal susceptibility of Malassezia pachydermatis in various media using a CLSI protocol. Vet Microbiol. 2012;159:536–40.
Tenover FC. Antibiotic susceptibility testing. In: Schaechter M, editor. Encyclopedia of microbiology. 3rd ed. San Diego: San Diego State University; 2009. p. 67–77.
Brilhante RSN, Rocha MGD, Guedes GMM, et al. Malassezia pachydermatis from animals: planktonic and biofilm antifungal susceptibility and its virulence arsenal. Vet Microbiol. 2018;220:47–52.
Chiavassa E, Tizzani P, Peano A. In vitro antifungal susceptibility of Malassezia pachydermatis strains isolated from dogs with chronic and acute otitis externa. Mycopathologia. 2014;178:315–9.
Watanabe S, Koike A, Kano R, Nagata M, Chen C, Hwang CY, et al. In vitro susceptibility of Malassezia pachydermatis isolates from canine skin with atopic dermatitis to ketoconazole and itraconazole in East Asia. J Vet Med Sci. 2014;76:579–81.
Angileri M, Pasquetti M, De Lucia M, Peano A. Azole resistance of Malassezia pachydermatis causing treatment failure in a dog. Med Mycol Case Rep. 2019;23:58–61.
Kano R, Yokoi S, Kariya N, Oshimo K, Kamata H. Multi-azole-resistant strain of Malassezia pachydermatis isolated from a canine Malassezia dermatitis. Med Mycol. 2019;57:346–50.
Crespo MJ, Abarca ML, Cabañes FJ. Evaluation of different preservation and storage methods for Malassezia spp. J Clin Microbiol. 2000;38:3872–5.
Iatta R, Puttilli MR, Immediato D, Otranto D, Cafarchia C. The role of drug efflux pumps in Malassezia pachydermatis and Malassezia furfur defence against azoles. Mycoses. 2017;60:178–82.
Joseph-Horne T, Hollomon DW. Molecular mechanisms of azole resistance in fungi. FEMS Microbiol Lett. 1997;149:141–9.
Feng W, Yang J, Xi Z, Qiao Z, et al. Mutations and/or overexpressions of ERG4 and ERG11 genes in clinical azoles-resistant isolates of Candida albicans. Microb Drug Resist. 2017;23:563–70.
Park M, Cho Y, Lee YW, Jung WH. Genomic multiplication and drug efflux influence ketoconazole resistance in Malassezia restricta. Front Cell Infect Microbiol. 2020;10:191.
Kim M, Cho Y, Park M, Choi Y, Hwang SY, Jung WH. Genomic tandem quadruplication is associated with ketoconazole resistance in Malassezia pachydermatis. J Microbiol Biotechnol. 2018;28:1937–45.
Pasquetti M, Chiavassa E, Tizzani P, Danesi P, Peano A. Agar diffusion procedures for susceptibility testing of Malassezia pachydermatis: Evaluation of Mueller-Hinton agar plus 2 % glucose and 0.5 µg/ml methylene blue as the test medium. Mycopathologia. 2015;180:153–8.
Larkin MA, Blackshields G, Brown NP, et al. Clustal W and Clustal X version 2.0. Bioinformatics. 2007;23:2947–8.
Choi Y, Chan AP. PROVEAN web server: a tool to predict the functional effect of amino acid substitutions and indels. Bioinformatics. 2015;31:2745–7.
Tamura K, Stecher G, Kumar S. MEGA11: molecular evolutionary genetics analysis version 11. Mol Biol Evol. 2021;38:3022–7.
Puig L, Castellá G, Cabañes FJ. Cryptic diversity of Malassezia pachydermatis from healthy and diseased domestic animals. Mycopathologia. 2016;181:681–8.
Castellá G, Coutinho SD, Cabañes FJ. Phylogenetic relationships of Malassezia species based on multilocus sequence analysis. Med Mycol. 2014;52:99–105.
Nascimento M, Sousa A, Ramirez M, Francisco AP, Carriço JA, Vaz C. PHYLOViZ 2.0: providing scalable data integration and visualization for multiple phylogenetic inference methods. Bioinformatics. 2017;33:128–9.
Gupta AK, Kohli Y, Li A, Faergemann J, Summerbell RC. In vitro susceptibility of the seven Malassezia species to ketoconazole, voriconazole, itraconazole and terbinafine. Br J Dermatol. 2000;142:758–65.
Cafarchia C, Figueredo LA, Iatta R, Montagna MT, Otranto D. In vitro antifungal susceptibility of Malassezia pachydermatis from dogs with and without skin lesions. Vet Microbiol. 2012;155:395–8.
Carrillo-Muñoz AJ, Rojas F, Tur-Tur C, et al. In vitro antifungal activity of topical and systemic antifungal drugs against Malassezia species. Mycoses. 2013;56:571–5.
Álvarez-Pérez S, García ME, Peláez T, Blanco JL. Genotyping and antifungal susceptibility testing of multiple Malassezia pachydermatis isolates from otitis and dermatitis cases in pets: is it really worth the effort? Med Mycol. 2016;54:72–9.
Jesus FP, Lautert C, Zanette RA, et al. In vitro susceptibility of fluconazole-susceptible and -resistant isolates of Malassezia pachydermatis against azoles. Vet Microbiol. 2011;152:161–4.
Sickafoose L, Hosgood G, Snook T, Westermeyer R, Merchant S. A noninferiority clinical trial comparing fluconazole and ketoconazole in combination with cephalexin for the treatment of dogs with Malassezia dermatitis. Vet Ther. 2010;11:E1–13.
Bernardo FM, Martins HM, Martins ML. A survey of mycotic otitis externa of dogs in Lisbon. Rev Iberoam Micol. 1998;15:163–5.
Weiler CB, de Jesus FP, Nardi GH, et al. Susceptibility variation of Malassezia pachydermatis to antifungal agents according to isolate source. Braz J Microbiol. 2013;44:174–8.
Lorenzini R, de Bernardis F. Studies on the isolation, growth and maintenance of Malassezia pachydermatis. Mycopathologia. 1987;99:129–31.
Arikan S. Current status of antifungal susceptibility testing methods. Med Mycol. 2007;45:569–87.
Kim D, Lim YR, Ohk SO, Kim BJ, Chun YJ. Functional expression and characterization of CYP51 from dandruff-causing Malassezia globosa. FEMS Yeast Res. 2011;11:80–7.
Vazquez JA, Manavathu EK. Molecular characterization of a voriconazole-resistant, posaconazole-susceptible Aspergillus fumigatus isolate in a lung transplant recipient in the United States. Antimicrob Agents Chemother. 2015;60:1129–33.
Selb R, Fuchs V, Graf B, et al. Molecular typing and in vitro resistance of Cryptococcus neoformans clinical isolates obtained in Germany between 2011 and 2017. Int J Med Microbiol. 2019;309: 151336.
Cafarchia C, Figueredo LA, Iatta R, Colao V, Montagna MT, Otranto D. In vitro evaluation of Malassezia pachydermatis susceptibility to azole compounds using E-test and CLSI microdilution methods. Med Mycol. 2012;50:795–801.
Kano R, Aramaki C, Murayama N, et al. High multi-azole-resistant Malassezia pachydermatis clinical isolates from canine Malassezia dermatitis. Med Mycol. 2020;58:197–200.
Kano R, Kamata H. Miconazole-tolerant strains of Malassezia pachydermatis generated by culture in medium containing miconazole. Vet Dermatol. 2020;31:97–101.
Leong C, Kit JCW, Lee SM, et al. Azole resistance mechanisms in pathogenic M. furfur. Antimicrob Agents Chemother. 2021;65:e01975-e2020.
Cernicka J, Subik J. Resistance mechanisms in fluconazole-resistant Candida albicans isolates from vaginal candidiasis. Int J Antimicrob Agents. 2006;27:403–8.
Morio F, Loge C, Besse B, Hennequin C, Le Pape P. Screening for amino acid substitutions in the Candida albicans Erg11 protein of azole-susceptible and azole-resistant clinical isolates: new substitutions and a review of the literature. Diagn Microbiol Infect Dis. 2010;66:373–84.
Flowers SA, Colón B, Whaley SG, Schuler MA, Rogers PD. Contribution of clinically derived mutations in ERG11 to azole resistance in Candida albicans. Antimicrob Agents Chemother. 2015;59:450–60.
Berkow EL, Lockhart SR. Fluconazole resistance in Candida species: a current perspective. Infect Drug Resist. 2017;10:237–45.
Zhang J, Li L, Lv Q, Yan L, Wang Y, Jiang Y. The fungal CYP51s: their functions, structures, related drug resistance, and inhibitors. Front Microbiol. 2019;10:691.
Xiang MJ, Liu JY, Ni PH, Wang S, Shi C, Wei B, Ni YX, Ge HL. Erg11 mutations associated with azole resistance in clinical isolates of Candida albicans. FEMS Yeast Res. 2013;13:386–93.
Marichal P, Koymans L, Willemsens S, Bellens D, Verhasselt P, Luyten W, Borgers M, Ramaekers FCS, Odds FC, Vanden BH. Contribution of mutations in the cytochrome P450 14alpha-demethylase (Erg11p, Cyp51p) to azole resistance in Candida albicans. Microbiology. 1999;145:2701–13.
Sheng C, Miao Z, Ji H, Yao J, Wang W, Che X, Dong G, Lü J, Guo W, Zhang W. Three-dimensional model of lanosterol 14 alpha-demethylase from Cryptococcus neoformans: active-site characterization and insights into azole binding. Antimicrob Agents Chemother. 2009;53:3487–95.
Acknowledgements
The authors thanks Laura Ordeix for a sample from a dog with recurrent dermatitis kindly provided for our work. The authors thank Carolina Gómez from the Veterinary Mycology Group of Universitat Autònoma de Barcelona (UAB) for valuable technical assistance.
Funding
Open Access Funding provided by Universitat Autonoma de Barcelona. Financial support came from Servei Veterinari de Bacteriologia i Micologia from the UAB.
Author information
Authors and Affiliations
Contributions
GC, MRB, and FJC contributed to the study conception and design. Material preparation, data collection and analysis were performed by LD, GC, MRB, and FJ C. The first draft of the manuscript was written by LD, and all authors commented and contributed to the preparation of the final manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Handling Editor: Takashi Sugita.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Díaz, L., Castellá, G., Bragulat, M.R. et al. ERG11 Gene Variability and Azole Susceptibility in Malassezia pachydermatis. Mycopathologia 188, 21–34 (2023). https://doi.org/10.1007/s11046-022-00696-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11046-022-00696-9