Abstract
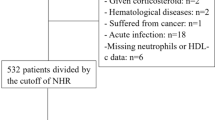
The neutrophil-to-platelet ratio (NPR) is considered to be an indicator of inflammatory status. The value of the NPR in predicting in-hospital adverse events (AEs) and long-term prognosis after percutaneous coronary intervention (PCI) in coronary artery disease (CAD) patients has not yet been reported. Meanwhile, the mechanisms behind its predictive value for long-term prognosis remain unreported as well. The study retrospectively enrolled 7284 consecutive patients with CAD undergoing PCI from January 2012 to December 2018. Multivariable logistic regression analysis, multivariable Cox regression analysis, Kaplan‒Meier (KM) curve analysis, restricted cubic spline (RCS) curve analysis, and sensitivity analysis were used in the study. All-cause death was the endpoint of the study. According to the median value of the NPR, the patients were divided into two groups: the high group (NPR ≥ 0.02, n = 3736) and the low group (NPR < 0.02, n = 3548). Multivariate logistic regression analysis demonstrated that a high NPR was a risk factor for in-hospital AEs [odds ratio (OR) = 1.602, 95% CI 1.347–1.909, p = 0.001]. During a mean follow-up period of 3.01 ± 1.49 years, the multivariate Cox regression analysis showed that a high NPR affected the long-term prognosis of patients (HR 1.22, 95% CI 1.03–1.45, p = 0.025) and cardiac death (HR 1.49, 95% CI 1.14–1.95, p = 0.003). The subgroup analysis showed that the NPR was affected by age and sex. The mediation analysis identified that the effect of the NPR on long-term outcomes is partially mediated by serum creatinine (Scr) and triglycerides. The NPR may be a convenient indicator of in-hospital AEs and poor long-term and cardiac outcomes in CAD patients. It might have impacted prognosis through effects on kidney function and lipid metabolism.





Similar content being viewed by others
Data availability
The data used are available from the corresponding author upon reasonable request.
References
Benjamin EJ, Virani SS, Callaway CW et al (2018) Heart disease and stroke statistics-2018 update: a report from the american heart association. Circulation 137(12):e67–e492
Björkegren J, Lusis AJ (2022) Atherosclerosis: recent developments. Cell 185(10):1630–1645
Crea F, Libby P (2017) Acute coronary syndromes: the way forward from mechanisms to precision treatment. Circulation 136(12):1155–1166
Libby P, Pasterkamp G, Crea F, Jang IK (2019) Reassessing the mechanisms of acute coronary syndromes. Circ Res 124(1):150–160
Libby P, Hansson GK (2019) From focal lipid storage to systemic inflammation: JACC review topic of the week. J Am Coll Cardiol 74(12):1594–1607
Alfonso F, Gonzalo N, Rivero F, Escaned J (2021) The year in cardiovascular medicine 2020: interventional cardiology. Eur Heart J 42(10):985–1003
Stähli BE, Klingenberg R, Heg D et al (2022) Mammalian target of rapamycin inhibition in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol 80(19):1802–1814
Libby P, Loscalzo J, Ridker PM et al (2018) Inflammation, immunity, and infection in atherothrombosis: JACC review topic of the week. J Am Coll Cardiol 72(17):2071–2081
Cahilog Z, Zhao H, Wu L et al (2020) The role of neutrophil NETosis in organ injury: novel inflammatory cell death mechanisms. Inflammation 43(6):2021–2032
Levey AS, James MT (2017) Acute kidney injury. Ann Intern Med 167(9):ITC66–ITC80
Boyle EM Jr, Pohlman TH, Johnson MC, Verrier ED (1997) Endothelial cell injury in cardiovascular surgery: the systemic inflammatory response. Ann Thorac Surg 63(1):277–284
Dziedzic EA, Gąsior JS, Tuzimek A et al (2022) Investigation of the associations of novel inflammatory biomarkers-systemic inflammatory index (SII) and systemic inflammatory response index (SIRI)-with the severity of coronary artery disease and acute coronary syndrome occurrence. Int J Mol Sci 23(17):9553
Allencherril J, Jneid H, Atar D et al (2019) Pathophysiology, diagnosis, and management of the no-reflow phenomenon. Cardiovasc Drugs Ther 33(5):589–597
Swirski FK (2020) Platelets have a dangerous hold over immune cells in cardiovascular disease. Nature 577(7790):323–324
Lin Y, Dai W, Chen Y, He X, Xu Y (2022) Neutrophil-to-platelet ratio predicts mortality following percutaneous coronary intervention in patients with acute ST-elevation myocardial infarction. Front Physiol 13:1011048. https://doi.org/10.3389/fphys.2022.1011048
Custodio-Chablé SJ, Lezama RA, Reyes-Maldonado E (2020) Platelet activation as a trigger factor for inflammation and atherosclerosis. Cir Cir 88(2):233–243
Seferović PM, Ašanin M, Ristić AD (2018) Acute stress disorder and C-reactive protein in patients with acute myocardial infarction. Eur J Prev Cardiol 25(7):702–705
Lin KY, Chen HC, Jiang H et al (2020) Predictive value of admission D-dimer for contrast-induced acute kidney injury and poor outcomes after primary percutaneous coronary intervention. BMC Nephrol 21(1):90
You ZB, Lin KY, Zheng WP et al (2018) Association of prealbumin levels with contrast-induced acute kidney injury in elderly patients with elective percutaneous coronary intervention. Clin Interv Aging 13:641–649
Žaliaduonytė-Pekšienė D, Lesauskaitė V, Liutkevičienė R et al (2017) Association of the genetic and traditional risk factors of ischaemic heart disease with STEMI and NSTEMI development. J Renin Angiotensin Aldosterone Syst 18(4):1470320317739987
Dziedzic EA, Gąsior JS, Tuzimek A, Kochman W (2023) Blood count-derived inflammatory markers and acute complications of ischemic heart disease in elderly women. J Clin Med 12(4):1369
Butt K, D’Souza J et al (2020) Correlation of the neutrophil-to-lymphocyte ratio (nlr) and platelet-to-lymphocyte ratio (plr) with contrast-induced nephropathy in patients with acute coronary syndrome undergoing percutaneous coronary interventions. Cureus 12(12):e11879
He J, Li J, Wang Y, Hao P, Hua Q (2014) Neutrophil-to-lymphocyte ratio (NLR) predicts mortality and adverse-outcomes after ST-segment elevation myocardial infarction in Chinese people. Int J Clin Exp Pathol 7(7):4045–4056
Nording H, Baron L, Langer HF (2020) Platelets as therapeutic targets to prevent atherosclerosis. Atherosclerosis 307:97–108
Cornara S, Crimi G, Somaschini A et al (2018) Systemic inflammatory status is associated with increased platelet reactivity in the early period after acute coronary syndromes. Platelets 29(5):528–530
Muller O, Hamilos M, Bartunek J et al (2010) Relation of endothelial function to residual platelet reactivity after clopidogrel in patients with stable angina pectoris undergoing percutaneous coronary intervention. Am J Cardiol 105(3):333–338
Mangiacapra F, Bartunek J, Bijnens N et al (2012) Periprocedural variations of platelet reactivity during elective percutaneous coronary intervention. J Thromb Haemost 10(12):2452–2461
Leader A, Pereg D, Lishner M (2012) Are platelet volume indices of clinical use? Multidiscip Rev Ann Med 44(8):805–816
Mangiacapra F, Colaiori I, Ricottini E et al (2018) Impact of platelet reactivity on 5-year clinical outcomes following percutaneous coronary intervention: a landmark analysis. J Thromb Thrombolysis 45(4):496–503
Li J, Sun X, Yang N et al (2023) Phosphoglycerate mutase 5 initiates inflammation in acute kidney injury by triggering mitochondrial DNA release by dephosphorylating the pro-apoptotic protein Bax. Kidney Int 103(1):115–133
Ohashi SN, DeLong JH, Kozberg MG et al (2023) Role of inflammatory processes in hemorrhagic stroke. Stroke 54(2):605–619
Chou WC, Jha S, Linhoff MW, Ting JP (2023) The NLR gene family: from discovery to present day. Nat Rev Immunol. https://doi.org/10.1038/s41577-023-00849-x
Li JW, Chen YD, Chen WR, Jing J, Liu J, Yang YQ (2016) Plasma DPP4 activity is associated with no-reflow and major bleeding events in Chinese PCI-treated STEMI patients. Sci Rep 6:39412
Hamann L, Koch A, Sur S et al (2013) Association of a common TLR-6 polymorphism with coronary artery disease—implications for healthy ageing. Immun Ageing 10(1):43
Jenny NS, Tracy RP, Ogg MS et al (2002) In the elderly, interleukin-6 plasma levels and the -174G>C polymorphism are associated with the development of cardiovascular disease. Arterioscler Thromb Vasc Biol 22(12):2066–2071
El-Awaisi J, Kavanagh DP, Rink MR, Weston CJ, Drury NE, Kalia N (2022) Targeting IL-36 improves age-related coronary microcirculatory dysfunction and attenuates myocardial ischemia/reperfusion injury in mice. JCI Insight. https://doi.org/10.1172/jci.insight.155236
Crea F, Battipaglia I, Andreotti F (2015) Sex differences in mechanisms, presentation and management of ischaemic heart disease. Atherosclerosis 241(1):157–168
Aryan L, Younessi D, Zargari M et al (2020) The role of estrogen receptors in cardiovascular disease. Int J Mol Sci 21(12):4314
Lau ES, Paniagua SM, Guseh JS et al (2019) Sex differences in circulating biomarkers of cardiovascular disease. J Am Coll Cardiol 74(12):1543–1553
McRae JL, Vikstrom IB, Bongoni AK et al (2020) Blockade of the G-CSF receptor is protective in a mouse model of renal ischemia-reperfusion injury. J Immunol 205(5):1433–1440. https://doi.org/10.4049/jimmunol.2000390
Brinkmann V, Zychlinsky A (2007) Beneficial suicide: why neutrophils die to make NETs. Nat Rev Microbiol 5(8):577–582. https://doi.org/10.1038/nrmicro1710
Saisorn W, Saithong S, Phuengmaung P et al (2021) Acute kidney injury induced lupus exacerbation through the enhanced neutrophil extracellular traps (and apoptosis) in Fcgr2b deficient lupus mice with renal ischemia reperfusion injury. Front Immunol 12:669162. https://doi.org/10.3389/fimmu.2021.669162
Tao M, He Y, Li L et al (2023) Identification and validation of immune-associated NETosis subtypes and biomarkers in anti-neutrophil cytoplasmic antibody associated glomerulonephritis. Front Immunol 14:1177968. https://doi.org/10.3389/fimmu.2023.1177968
Neumann JT, Thao L, Callander E et al (2022) Cardiovascular risk prediction in healthy older people. Geroscience 44(1):403–413. https://doi.org/10.1007/s11357-021-00486-z
Kilis-Pstrusinska K, Akutko K, Braksator J et al (2021) Kidney dysfunction and its progression in patients hospitalized duo to COVID-19: contribution to the clinical course and outcomes. J Clin Med 10(23):5522. https://doi.org/10.3390/jcm10235522
Nkambule BB, Chan MV, Lachapelle AR et al (2023) The association between platelet reactivity and lipoprotein levels in Framingham heart study participants. Thromb Res 225:103–109. https://doi.org/10.1016/j.thromres.2023.03.013
Hsu LA, Chou HH, Teng MS, Wu S, Ko YL (2021) Circulating chemerin levels are determined through circulating platelet counts in nondiabetic Taiwanese people: a bidirectional Mendelian randomization study. Atherosclerosis 320:61–69. https://doi.org/10.1016/j.atherosclerosis.2021.01.014
Goeritzer M, Schlager S, Kuentzel KB et al (2022) Adipose triglyceride lipase deficiency attenuates in vitro thrombus formation without affecting platelet activation and bleeding in vivo. Cells. https://doi.org/10.3390/cells11050850
Nordestgaard BG, Benn M, Schnohr P, Tybjaerg-Hansen A (2007) Nonfasting triglycerides and risk of myocardial infarction, ischemic heart disease, and death in men and women. JAMA 298(3):299–308. https://doi.org/10.1001/jama.298.3.299
Funding
(1) National Natural Science Foundation of China General Program (Grant Number: 81873495, 82070375). (2) Natural Science Foundation for Distinguished Young Scholars of Fujian Province (Grant Number: 2021J06030). (3) National Key Clinical Specialty Construction Project of China (Cardiovascular Medicine 2021). (4) Fujian Research and Training Grants for Young and Middle-aged Leaders in Health care.
Author information
Authors and Affiliations
Contributions
YX, JZ–concept and design, analyzed data, created tables and figures, drafted paper. XL–concept and design, analyzed data, drafted paper. XC–analyzed data, drafted paper. LZ, ML, XC, GZ, XC, JC, FC, BL and XH–collected data. YG– concept and design, supervised, edited paper. K-YL– concept and design, supervised, edited paper.
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
About this article
Cite this article
Xiang, Y., Zeng, J., Lin, X. et al. The predictive value of the neutrophil/platelet ratio on in-hospital adverse events and long-term prognosis in patients with coronary artery disease after percutaneous coronary intervention and its possible internal mechanism. Mol Cell Biochem (2023). https://doi.org/10.1007/s11010-023-04901-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11010-023-04901-1