Abstract
Objective
To understand topical fluoride-related beliefs and refusal behaviors for caregivers of children with special health care needs (CSHCN).
Methods
This was an explanatory sequential mixed methods study. For the quantitative analyses, we surveyed 520 caregivers to (a) compare fluoride-related beliefs between caregivers of CSHCN and caregivers of healthy children and (b) evaluate the association between special health care need (SHCN) status and topical fluoride refusal. We used logistic regression models to generate unadjusted odds ratios, confounder-adjusted odds ratios (AOR), and 95% confidence intervals (CI). For the qualitative analyses, we interviewed 56 caregivers who refused or were hesitant about topical fluoride. Data were coded deductively and compared by SHCN status to an existing conceptual model of topical fluoride refusal.
Results
In the quantitative analysis, 41.3% of caregivers refused or thought about refusing topical fluoride. There were no significant differences in fluoride beliefs by SHCN status (p-values > 0.05) nor was there a significant association between SHCN status and topical fluoride refusal (AOR: 0.65, 95% CI 0.37–1.14; p = 0.13). In the qualitative analysis, the relative importance of each domain of the conceptual model was similar between the caregiver groups. Two differences were that all caregivers of CSHCN thought fluoride was unnecessary and wanted to keep chemicals out of their child’s body.
Conclusions for Practice
While caregivers of CSHCN were not more likely to refuse topical fluoride than caregivers of healthy children, there may be important differences in the underlying reasons for refusing topical fluoride.
Significance
What is already known on this subject? CSHCN are at increased risk for tooth decay. Topical fluoride helps prevent tooth decay, but large numbers of caregivers refuse topical fluoride. A conceptual model of caregiver topical fluoride refusal has been developed, but its applicability to caregivers of CSHCN has not yet been evaluated.
What this study adds? This study provides empirical insight into fluoride refusal behaviors for caregivers of CSHCN. Caregivers of CSHCN may have different reasons for refusing topical fluoride. Findings from this study will help guide the development of tailored communication approaches for caregivers of CSHCN who refuse or may be hesitant about topical fluoride.
Similar content being viewed by others
Introduction
One-in-four US families has a child with special health care needs (SHCN) (HRSA, 2020). Dental care is the most prevalent unmet need for children with SHCN (CSHCN), and dental needs are greater for CSHCN from low-income families and those with more complex needs (Lewis, 2009). Furthermore, many CSHCN are prescribed sugary medications, given sweets to manage behaviors, have disabilities that can make toothbrushing difficult, and encounter barriers to dental care (Campanaro et al., 2014; Liu et al., 2010). As a result, subgroups of CSHCN are at increased risk for tooth decay (Chi et al., 2013).
While topical fluoride prevents tooth decay (Weintraub et al., 2006), caregiver refusal of topical fluoride has become a growing problem (Chi, 2017; Chi & Basson, 2018). Topical fluoride behaviors are thought to be on a continuum, with acceptance at one end, refusal at the other, and varying degrees of hesitancy along the continuum (Chi, 2017). One preliminary study reported that 12.7% of caregivers refused topical fluoride for their child during dental visits (Chi, 2014). The proportion of CSHCN caregivers who refuse or are hesitant about topical fluoride is unknown.
The reasons for topical fluoride hesitancy and refusal are not fully understood. One potential explanation is incomplete knowledge about fluoride (Chi et al., 2018). This could lead not only to refusal of topical fluoride during dental visits but also to avoidance of other common fluoride sources including water and toothpaste (Ko & Chi, 2023). Caregivers of CSHCN are known to actively seek information prior to making healthcare decisions (Du et al., 2019), which could expose caregivers to Internet-based misinformation- and disinformation (Hoffman et al., 2019). Between 2009 and 2017, 60% of water fluoridation mentions on Twitter were negative compared to 15% that were positive (Oh et al., 2020). Some caregivers believe fluoride is a neurotoxin that leads to lower IQ, autism, cancer, and other diseases (Choi et al., 2012; Strunecka & Strunecky, 2019). More recently, researchers have sought to identify the reasons for topical fluoride hesitancy and refusal. Based on qualitative interviews with 56 caregivers, Chi and colleagues developed a conceptual model with six domains to explain why caregivers are hesitant about topical fluoride (Chi et al., 2023).
Vaccine refusal is a documented correlate of topical fluoride refusal (Chi, 2014). The factors driving vaccine refusal may be similar to those that lead to topical fluoride refusal. Caregivers of CSHCN are more likely to refuse childhood vaccines than caregivers of healthy children (Cody & Lerand, 2013; Greenwood et al., 2013). One of the underlying concerns is that vaccines are unsafe and lead to conditions like autism (Abu Kuwaik et al., 2014; Dannetun et al., 2005; Roberts et al., 2015), a belief that has its origins in a now retracted publication from the 1990s (Eggertson, 2010).
Studies on topical fluoride refusal focusing on caregivers of CSHCN are limited. One study from Italy found that CSHCN have lower levels of fluoride exposure (Bagattoni et al., 2021). Another study from Singapore found that caregivers of CSHCN and caregivers of healthy children reported similar rates of refusal of silver diamine fluoride, which is another type of topical fluoride treatment (Hu et al., 2020). One US study reported that while caregivers of CSHCN had similar attitudes toward fluoridated products as caregivers of neurotypical children, the former were significantly less likely to use fluoridated toothpaste for their child (Capozza & Bimstein, 2012). Current literature in the US suggests that CSHCN caregivers are more likely to refuse topical fluoride because of safety concerns (Rada, 2010), but there is no empirical evidence for this. Thus, it is not clear whether caregivers of CSHCN have different beliefs regarding topical fluoride, whether they are more likely to refuse topical fluoride than caregivers of healthy children, and if the reasons for refusal or hesitancy are different.
There were three goals in this mixed methods study. The first goal was to compare fluoride-related beliefs for caregivers of CSHCN and caregivers of healthy children. The second goal was to evaluate the association between SHCN status and topical fluoride refusal. The third was to determine whether the reasons for topical fluoride refusal were different by SHCN status.
Methods
Study Design
This was an explanatory sequential mixed methods study involving secondary data collected by survey and interview from caregivers of CSHCN and healthy children (Fetters et al., 2013). The study was conducted in accordance with prevailing ethical principles and approved by the University of Washington Institutional Review Board.
Part 1: Quantitative Study
Participants
We recruited caregivers at five dental clinics in children’s hospitals or university-based pediatric dental clinics in the US. Survey participants were also recruited through social media, flyers, private dental practices, and naturopathic medicine practices. All participants were required to be at least 18 years old, provide informed consent, able to read and understand English, and to be a caregiver of a child under the age of 18 years. A sample size of at least 500 caregiver survey respondents was based on power calculations for the primary intent of the survey data, which was to conduct psychometric testing of a fluoride hesitancy identification tool (Carle et al., 2022; Edwards et al., 2023). We did not track survey participation rates.
Study Procedures
We piloted, revised, and finalized an 85-item questionnaire that included questions on caregiver beliefs about topical fluoride, history of fluoride hesitancy or refusal, and demographics (Online Appendix). We sent potential participants a postcard or an email link to an online REDCap survey. Additional participants completed the online survey on study tablets at one of the study sites or accessed the survey link through QR codes placed on social media posts or study flyers. The survey was administered from November 2020 to April 2021. For caregivers with multiple children, the youngest child was designated as a referent. Before the survey, participants were asked to read and accept a written consent statement. Written documentation of consent was not obtained. After completing the survey, caregivers had the option to enter a raffle to win an Apple iPad or a pair of electric toothbrushes.
Independent Variable
The independent variable was being a caregiver of a child with SHCN (no/yes). Caregivers were classified as having a child with SHCN if they reported their child required a medication other than vitamins prescribed by a doctor (Carle et al., 2011).
Primary Outcome Variables
The primary outcome variables were topical fluoride beliefs, which were measured with six items (Table 1). Response options were on a 0–10 scale or a four-category Likert-like response. For the statistical analyses, all responses were dichotomized.
Secondary Outcome Variable
The secondary outcome, topical fluoride refusal, was measured with the following item: “Regarding topical fluoride in general for your child, which statement below best describes you.” The five-category response options included: (1) “I always say no”, (2) “Most of the time I say no”, (3) “Sometimes I say no”, (4) “I say yes, but I have thought about saying no”, or (5) “I always say yes.” Caregivers who responded 1–4 were classified as expressing some degree of topical fluoride hesitancy or refusal and those who responded 5 were classified as accepting topical fluoride.
Confounding Variables
There were six confounders: caregiver age, gender, race, ethnicity, education, and household income. Age was modeled as a continuous variable. There were three gender categories (male, female, nonbinary/other). Caregiver race was a self-reported nine-category variable corresponding to the US Census Bureau categories (white, Black, Asian, American Indian or Alaskan Native, Native Hawaiian or other Pacific Islander, other, multiple race). Ethnicity was defined as Hispanic, Latino, or Spanish origin (no/yes). There were five education categories, ranging from “less than a high school diploma” to “more than a four-year college degree.” Income was a seven-category variable.
Statistical Analysis
Descriptive statistics were generated for the study population and either the independent t-test (continuous variables) or chi-square test (categorical variables) was used to compare the distribution of demographic characteristics by SHCN status. We generated the distribution of the primary and secondary outcome variables for the overall study population and by SHCN status. Logistic regression models were used to generate unadjusted odds ratios (OR) and confounder-adjusted odds ratios (AOR) with corresponding 95% confidence intervals (CI) for the associations between SHCN status and (a) topical fluoride beliefs and (b) topical fluoride refusal (α = 0.05). Participants with missing data were excluded from the regression models. All analyses were completed using SPSS v 27.
Part 2: Qualitative Study
Participants
Caregivers were eligible if they were at least 18 years old, able to communicate in English, the caregiver of a child under the age of 18 years, and if they did not decline topical fluoride exclusively for financial reasons. Caregivers who answered ≥ 2 to the screening question “On a scale of 1 to 10, with 1 being not opposed at all and 10 being totally opposed, how opposed are you to topical fluoride for your child or any of your children?” were eligible for the study. We used billing codes and health records from two pediatric dentistry clinics in Washington State to identify children who did not receive topical fluoride during a routine dental visit between August 2016 and September 2018. Additional caregivers were identified through private practice clinic referrals, social media, personal networks of study team members, and through snowball sampling. Trained research assistants contacted 513 caregivers of these children by telephone to verify eligibility. We were able to reach 173 caregivers, of whom 56 were not interested and 12 did not speak English. Of the remaining 95 caregivers, 23 were not eligible. Of the remaining 76 caregivers, 56 completed an interview.
Data Collection, Management, and Analysis
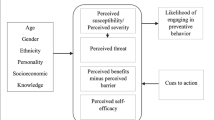
Interview data were collected using procedures described previously with informed consent obtained prior to the start of the interview (Chi et al., 2023). Caregiver participants were recruited and interviewed until saturation on themes was reached. The interview transcripts were manually reviewed and collated into two groups based on whether the caregiver voluntarily stated during the interview that their child has a SHCN. We generated descriptive statistics on the interview population and compared characteristics by SHCN status (yes/no) using the t-test or chi-square test (α = 0.05). Based on previous qualitative work (Chi et al., 2023), we created a codebook with 21 categories organized into six domains, with each domain indicating a reason for refusing topical fluoride: (1) thinking topical fluoride is unnecessary; (2) wanting to keep chemicals like fluoride out of my child’s body; (3) thinking fluoride is harmful; (4) thinking there is too much uncertainty with fluoride; (5) feeling pressured to get fluoride; and (6) feeling fluoride should be a choice (Fig. 1). Transcripts were coded using a deductive coding approach and content analytic techniques (Corbin & Strauss, 2008; Krippendorf, 1980). A unit of data consisted of one complete thought. Units were grouped together based on common themes in the category. To ensure accuracy, we used comparative analysis to compare the unitized data across the categories (Corbin & Strauss, 2008). Coding discrepancies were addressed and resolved through debriefing between coders. After coding, caregiver responses within each category and domain were calculated as percentages. While caregivers could be represented across multiple categories, responses from each caregiver were counted only once per category. All quotes reported were from caregivers of CSHCN. Analyses were completed using SPSS v 27.
Results
Part 1: Quantitative Study
Descriptive Statistics
Among the 520 surveyed caregivers, 87 (16.7%) reported having a child with SHCN and 433 (82.3%) had a healthy child (Table 2). Caregivers of CSHCN were significantly older than caregivers of healthy children (44.6 years and 41.1 years, respectively; p < 0.001). There were no other significant differences between caregiver groups.
Beliefs about Topical Fluoride
Caregiver beliefs about topical fluoride are summarized in Table 3. In the confounder-adjusted models, there were no significant differences in topical fluoride beliefs by SHCN status.
Topical Fluoride Refusal
The prevalence of topical fluoride refusal was 34.5% for caregivers of CSHCN and 43.3% for caregivers of healthy children. There was no significant difference in topical fluoride refusal by SHCN status in the unadjusted and confounder-adjusted models (unadjusted OR: 0.70; 95% CI 0.43–1.14; p = 0.15; AOR: 0.65; 95% CI 0.37–1.14; p = 0.13, respectively). Among caregivers of CSHCN, 7.0% always said no to topical fluoride, 3.5% said no most of the time, 9.3% sometimes said no, 15.1% said yes but thought about saying no, and 65.1% always said yes, which was not statistically different from caregivers of healthy children (p = 0.73).
Part 2: Qualitative Study
Descriptive Statistics
Of the 56 interviewed caregivers, 12 reported having a child with SHCN (Table 4). Caregivers of CSHCN were significantly older than caregivers of healthy children (47.4 years and 40.5 years, respectively; p = 0.03). There were no other differences by SHCN status.
Reasons for Refusing Topical Fluoride
Responses from caregivers of CSHCN were represented across all six domains from the conceptual model (Table 5). Caregivers of CSHCN provided similar reasons for topical fluoride refusal as caregivers of healthy children, but there were observed differences. Below, we provide a summary of findings by domain and report frequencies of responses, highlighting differences by SHCN status.
Domain 1: Thinking Topical Fluoride Is Unnecessary
All caregivers of CSHCN (100%) believed topical fluoride was unnecessary to keep their child’s teeth healthy compared to 89% of caregivers of healthy children. A 63-year-old caregiver of a 13-year-old child with SHCN said
He reacts to things differently than regular children…I don’t introduce anything into his world that isn’t absolutely necessary.
Among caregivers of CSHCN, 75% believed topical fluoride is ineffective in preventing cavities compared to 59% of caregivers of healthy children. About 25% of caregivers of CSHCN compared to 50% of caregivers of healthy children believed diet is more important than topical fluoride.
Domain 2: Wanting to Keep Chemicals Like Fluoride Out of My Child’s Body
All caregivers of CSHCN (100%) wanted to keep chemicals like fluoride out of their child’s body compared to 82% of caregivers of healthy children. About 67% of caregivers of CSHCN expressed not wanting their child to have too much fluoride, especially if their child already received fluoride from other sources like water or toothpaste, compared to 41% of caregivers of healthy children. A 61-year-old caregiver of a 15-year-old child with SHCN said
I would rather err on the side of caution than introduce potentially harmful chemicals into his body that may or may not disrupt his system more than it already is disrupted.
Domain 3: Thinking Fluoride Is Harmful
Similar proportions of caregivers by SHCN status expressed concerns about the negative health consequences of topical fluoride (92% for CSHCN and 89% for healthy). While only 25% of caregivers of CSHCN believed fluoride is dangerous to their child’s health (compared to 82% of caregivers of healthy children), relatively larger proportions of caregivers of CSHCN believed fluoride would damage their child’s body, affect their child’s developing mind, or upset their child. A 34-year-old caregiver of a 6-year-old son with SHCN and a 12-year-old daughter with SHCN shared
My daughter [is] very sensitive and seems to have a hormone imbalance, so I just didn’t want to continue with [topical fluoride]…[Also, my son] is already significantly delayed in his development. I can’t risk a chance that it could be hindered any further…since I was told [topical fluoride] was a neurotoxin.
Notably, 50% of caregivers of CSHCN described their child having past negative experiences with topical fluoride compared to 7% of caregivers of healthy children. Caregivers of CSHCN expressed concerns that topical fluoride could cause their child discomfort, especially if they were sensitive to stimuli like the taste, smell, or texture of topical fluoride. A 42-year-old caregiver of an 8-year-old child with SHCN stated
I’ve never refused treatment just because I feel differently about fluoride. It’s always how my kid’s doing that day, how they’re behaving…and if I feel like he [my son] would tolerate it.
Domain 4: Thinking There Is Too Much Uncertainty with Fluoride
Similar proportions of caregivers of CSHCN and caregivers of healthy children felt there is too much uncertainty about fluoride (75% and 70%, respectively). No caregivers of CSHCN (0%) mentioned feeling that they did not know enough about fluoride (compared to 36% of caregivers of healthy children), whereas 58% had heard negative things about it (compared to 25% for healthy).
Domain 5: Feeling Pressured to Get Fluoride
Similar proportions of caregivers by SHCN status felt pressured to get fluoride (58% for CSHCN and 61% for healthy). Two times as many caregivers of CSHCN felt that they were not being told the whole truth about fluoride (58% for CSHCN and 30% for healthy) whereas one-half as many felt like there was an agenda on the part of others to push fluoride (17% for CSHCN and 41% for healthy).
Domain 6: Feeling Fluoride Should Be a Choice
About 50% of caregivers of CSHCN believed they should have autonomy over health care decisions for their child, which was comparable to the 45% of caregivers of healthy children.
Discussion
The study goal was to understand topical fluoride-related beliefs and refusal behaviors for caregivers of CSHCN compared to caregivers of healthy children. There were three main findings. First, fluoride-related beliefs were similar for the two caregiver groups. Second, SHCN status was not significantly associated with fluoride refusal. Third, the reasons for refusal were similar but all caregivers of CSHCN thought fluoride was unnecessary and wanted to keep chemicals out of their child’s body. Collectively, our findings suggest that while caregivers of CSHCN have similar beliefs to caregivers of healthy children and are not more likely to refuse topical fluoride, there may be clinically meaningful differences in the reasons for refusing topical fluoride for caregivers of CSHCN.
Fluoride-related beliefs were similar for both groups of caregivers. A 2010 study found that caregivers of children with autism reported concerns about the safety of fluoride and its side effects (Rada, 2010). Our findings suggest that caregivers of CSHCN are not more likely to believe that topical fluoride lowers IQ or causes autism or other health problems. One potential explanation for this inconsistency is that the Rada publication focused only on caregivers of children with autism whereas we included both caregivers of CSHCN and caregivers of healthy children. Current literature suggests that vaccine related beliefs are closely related to vaccine related beliefs (Carpiano & Chi, 2018). An HPV vaccination study found that caregivers of immunosuppressed children have concerns about the side effects of vaccines, but like the Rada study, these beliefs were not compared to the beliefs of caregivers of healthy children (Seale et al, 2012). Caregivers of CSHCN may have concerns about preventive care like topical fluoride and vaccines, but more research is needed to determine whether these concerns are different.
We also found no difference in topical fluoride refusal prevalence between caregiver groups. This is consistent with a study from Singapore on silver diamine fluoride, which also found no difference in the prevalence of acceptance by autism status (Hu et al., 2020). Another study found that dentists believe caregivers of CSHCN are more likely to refuse topical fluoride, but our current findings do not support this belief (Chi & Basson, 2018). While there may not be a statistically significant difference in topical fluoride refusal by SHCN status, it is important to note that the prevalence of topical fluoride hesitancy and refusal among caregivers of CSHCN in our study was high (34.5%). Given that caregivers of CSHCN are more likely to report their child to have poor oral health, not getting topical fluoride may have disproportionately negative consequences for children at higher risk for tooth decay. Future research should assess whether topical fluoride refusal leads to poorer health outcomes for CSHCN compared to healthy children.
We also found that reasons for refusal were similar across caregiver groups, with two notable differences. All interviewed caregivers of CSHCN thought that fluoride was unnecessary and wanted to keep chemicals out of their child’s body. Vaccine hesitancy studies on caregivers of CSHCN have also cited concerns about toxins and vaccines being unnecessary as reasons why caregivers refuse vaccines for their child (Hofstetter et al., 2018; Mensah-Bonsu et al., 2021). Although the literature implies that the six-domain conceptual model of topical fluoride hesitancy applies to all caregivers, our findings suggest that the reasons underlying refusal are nuanced (Chi et al., 2023). Future work should focus on validating our findings to determine if the conceptual model is applicable to subgroups of caregivers.
While additional research is needed to understand how caregivers of CSHCN make decisions about topical fluoride, our study findings have immediate clinical relevance. Several chairside strategies can be used to address topical fluoride hesitancy and refusal including the following: (1) assess the child’s tooth decay risk; (2) determine caregiver’s beliefs about topical fluoride and reasons for refusal or hesitancy; (3) ask about willingness to try other forms of fluoride and alternative prevention strategies, such as dietary changes (Chi, 2017).
There were two main study limitations. First, we recruited a small number of caregivers of CSHCN. Future studies should focus on recruiting large groups of caregivers of CSHCN to assess the validity of our findings. Second, because of the heterogeneity within the CSHCN population, our screening question for CSHCN in the quantitative survey may have led to misclassification. We did not collect specific diagnostic information about the child. However, the prevalence of CSHCN in our study is consistent with previously reported national prevalence of CSHCN, which is an indication that our SHCN measure is accurate. Future studies should focus on identifying specific subgroups at high risk for dental caries, such as children with intellectual or developmental disabilities.
Conclusions for Practice
While caregivers of CSHCN had similar beliefs and were equally as likely to refuse topical fluoride as caregivers of healthy children, they may have different reasons for refusing topical fluoride. These reasons are important in guiding the development of tailored interventions for caregivers of CSHCN, which can ultimately help to address oral health disparities experienced by children who have the most to benefit from the preventive effects of topical fluoride.
Data Availability
The data used in this manuscript are not publicly available.
Code Availability
Not applicable.
Abbreviations
- CSHCN:
-
Children with special health care needs
- SHCN:
-
Special health care needs
- ASD:
-
Autism spectrum disorder
- OR:
-
Odds ratios
- AOR:
-
Adjusted odds ratios
References
Abu Kuwaik, G., Roberts, W., Zwaigenbaum, L., Bryson, S., Smith, I. M., Szatmari, P., Modi, B. M., Tanel, N., & Brian, J. (2014). Immunization uptake in younger siblings of children with autism spectrum disorder. Autism: the International Journal of Research and Practice, 18(2), 148–155. https://doi.org/10.1177/1362361312459111
Bagattoni, S., Lardani, L., D’Alessandro, G., & Piana, G. (2021). Oral health status of Italian children with Autism Spectrum Disorder. European Journal of Paediatric Dentistry, 22(3), 243–247. https://doi.org/10.23804/ejpd.2021.22.03.12
Campanaro, M., Huebner, C. E., & Davis, B. E. (2014). Facilitators and barriers to twice daily tooth brushing among children with special health care needs. Special Care in Dentistry, 34(4), 185–192. https://doi.org/10.1111/scd.12057
Capozza, L. E., & Bimstein, E. (2012). Preferences of parents of children with autism spectrum disorders concerning oral health and dental treatment. Pediatric Dentistry, 34(7), 480–484.
Carle, A., Kerr, D., Edwards, T., Carpiano, R. M., Patiño Nguyen, D. P., Shands, M. E., Chi, D. L. (2022). Developing and validating a measure of caregiver topical fluoride hesitancy. In 2022 CityMatCH Leadership and MCH Epidemiology Conference.
Carle, A., Pallotto, I., Edwards, T., Carpiano, R., Kerr, D., & Chi, D. L. (2023). Psychometric properties of the fluoride hesitancy identification tool. Under review.
Carle, A. C., Blumberg, S. J., & Poblenz, C. (2011). Internal psychometric properties of the children with special health care needs screener. Academic Pediatrics, 11(2), 128–135. https://doi.org/10.1016/j.acap.2009.11.006
Carpiano, R. M., & Chi, D. L. (2018). Parents’ attitudes towards topical fluoride and vaccines for children: Are these distinct or overlapping phenomena? Preventive Medicine Reports, 10, 123–128. https://doi.org/10.1016/j.pmedr.2018.02.014
Chi, D. L. (2014). Caregivers who refuse preventive care for their children: The relationship between immunization and topical fluoride refusal. American Journal of Public Health, 104(7), 1327–1333. https://doi.org/10.2105/AJPH.2014.301927
Chi, D. L. (2017). Parent refusal of topical fluoride for their children: clinical strategies and future research priorities to improve evidence-based pediatric dental practice. Dental Clinics of North America, 61(3), 607–617. https://doi.org/10.1016/j.cden.2017.03.002
Chi, D. L., & Basson, A. A. (2018). Surveying dentists’ perceptions of caregiver refusal of topical fluoride. JDR Clinical and Translational Research, 3(3), 314–320. https://doi.org/10.1177/2380084418761846
Chi, D. L., Kerr, D., Patiño-Nguyen, D., Shands, M. E., Cruz, S., Edwards, T., Carle, A., Carpiano, R., & Lewis, F. (2023). A conceptual model caregivers’ hesitancy of topical fluoride for their children. PLoS One, 18(3), e0282834. https://doi.org/10.1371/journal.pone.0282834
Chi, D. L., Richman, J., Senturia, K., & Zahlis, E. (2018). Caregivers’ understanding of fluoride varnish: Implications for future clinical strategies and research on preventive care decision making. Journal of Public Health Dentistry, 78(4), 282–286. https://doi.org/10.1111/jphd.12277
Chi, D. L., Rossitch, K. C., & Beeles, E. M. (2013). Developmental delays and dental caries in low-income preschoolers in the USA: A pilot cross-sectional study and preliminary explanatory model. BMC Oral Health, 13, 53. https://doi.org/10.1186/1472-6831-13-53
Choi, A. L., Sun, G., Zhang, Y., & Grandjean, P. (2012). Developmental fluoride neurotoxicity: A systematic review and meta-analysis. Environmental Health Perspectives, 120(10), 1362–1368. https://doi.org/10.1289/ehp.1104912
Cody, P. J., & Lerand, S. J. (2013). HPV vaccination in female children with special health care needs. Journal of Pediatric and Adolescent Gynecology, 26(4), 219–223. https://doi.org/10.1016/j.jpag.2013.03.003
Corbin, J. M., & Strauss, A. L. (2008). Basics of qualitative research: Techniques and procedures for developing grounded theory. Sage Publications.
Dannetun, E., Tegnell, A., Hermansson, G., & Giesecke, J. (2005). Parents’ reported reasons for avoiding MMR vaccination: A telephone survey. Scandinavian Journal of Primary Health Care, 23(3), 149–153. https://doi.org/10.1080/02813430510031306
Du, R. Y., Yiu, C., & King, N. M. (2019). Oral health behaviours of preschool children with autism spectrum disorders and their barriers to dental care. Journal of Autism and Developmental Disorders, 49(2), 453–459. https://doi.org/10.1007/s10803-018-3708-5
Edwards, T. C., Carle, A., Kerr, D., Carpiano, R. M., Nguyen, D. P., Orack, J. C., Chi, D. L. (2023). Topical fluoride hesitancy among caregivers: Development of a content-valid topical fluoride hesitancy identification item pool. J Public Health Dent, 83(1):116–122. https://doi.org/10.1111/jphd.12558
Eggertson, L. (2010). Lancet retracts 12-year-old article linking autism to MMR vaccines. CMAJ: Canadian Medical Association Journal, 182(4), E199–E200. https://doi.org/10.1503/cmaj.109-3179
Fetters, M. D., Curry, L. A., & Creswell, J. W. (2013). Achieving integration in mixed methods designs-principles and practices. Health Services Research, 48(6 Pt 2), 2134–2156. https://doi.org/10.1111/1475-6773.12117
Greenwood, V. J., Crawford, N. W., Walstab, J. E., & Reddihough, D. S. (2013). Immunisation coverage in children with cerebral palsy compared with the general population. Journal of Paediatrics and Child Health, 49(2), E137–E141. https://doi.org/10.1111/jpc.12097
Hoffman, B. L., Felter, E. M., Chu, K. H., Shensa, A., Hermann, C., Wolynn, T., Williams, D., & Primack, B. A. (2019). It’s not all about autism: The emerging landscape of anti-vaccination sentiment on Facebook. Vaccine, 37(16), 2216–2223. https://doi.org/10.1016/j.vaccine.2019.03.003
Hofstetter, A. M., Simon, T. D., Lepere, K., Ranade, D., Strelitz, B., Englund, J. A., & Opel, D. J. (2018). Parental vaccine hesitancy and declination of influenza vaccination among hospitalized children. Hospital Pediatrics, 8(10), 628–635. https://doi.org/10.1542/hpeds.2018-0025
HRSA. (2020). Children with special health care needs NSCH data brief. Retrieved from https://www.hrsa.gov/
Hu, S., Meyer, B., Lai, B., Chay, P. L., & Tong, H. J. (2020). Parental acceptance of silver diammine fluoride in children with autism spectrum disorder. International Journal of Paediatric Dentistry, 30(4), 514–522. https://doi.org/10.1111/ipd.12624
Ko, A., & Chi, D. L. (2023). Fluoride hesitancy: A mixed methods study on decision-making about forms of fluoride. Community Dentistry and Oral Epidemiology, 51(5), 997–1008. https://doi.org/10.1111/cdoe.12800
Krippendorf, K. (1980). Content analysis: An introduction to its methodology. Sage.
Lewis, C. W. (2009). Dental care and children with special health care needs: A population-based perspective. Academic Pediatrics, 9(6), 420–426. https://doi.org/10.1016/j.acap.2009.09.005
Liu, H. Y., Chen, C. C., Hu, W. C., Tang, R. C., Chen, C. C., Tsai, C. C., & Huang, S. T. (2010). The impact of dietary and tooth-brushing habits to dental caries of special school children with disability. Research in Developmental Disabilities, 31(6), 1160–1169. https://doi.org/10.1016/j.ridd.2010.08.005
Mensah-Bonsu, N., Mire, S. S., Sahni, L. C., Berry, L. N., Dowell, L. R., Minard, C. G., Cunningham, R. M., Boom, J. A., Voigt, R. G., & Goin-Kochel, R. P. (2021). Understanding vaccine hesitancy among parents of children with autism spectrum disorder and parents of children with non-autism developmental delays. Journal of Child Neurology, 36(10), 911–918. https://doi.org/10.1177/08830738211000505
Oh, H. J., Kim, C. H., & Jeon, J. G. (2020). Public sense of water fluoridation as reflected on Twitter 2009–2017. Journal of Dental Research, 99(1), 11–17. https://doi.org/10.1177/0022034519885610
Rada, R. E. (2010). Controversial issues in treating the dental patient with autism. Journal of the American Dental Association (1939), 141(8), 947–953. https://doi.org/10.14219/jada.archive.2010.0308
Roberts, J. R., Thompson, D., Rogacki, B., Hale, J. J., Jacobson, R. M., Opel, D. J., & Darden, P. M. (2015). Vaccine hesitancy among parents of adolescents and its association with vaccine uptake. Vaccine, 33(14), 1748–1755. https://doi.org/10.1016/j.vaccine.2015.01.068
Seale, H., Trung, L., Mackie, F. E., Kennedy, S. E., Boros, C., Marshall, H., Tidswell, J., Shaw, P. J., Montgomery, K., & MacIntyre, C. R. (2012). A qualitative study investigating knowledge and attitudes regarding human papillomavirus (HPV) and the HPV vaccine among parents of immunosuppressed children. Vaccine, 30(49), 7027–7031. https://doi.org/10.1016/j.vaccine.2012.09.066
Strunecka, A., & Strunecky, O. (2019). Chronic fluoride exposure and the risk of autism spectrum disorder. International Journal of Environmental Research and Public Health, 16(18), 3431. https://doi.org/10.3390/ijerph16183431
Weintraub, J. A., Ramos-Gomez, F., Jue, B., Shain, S., Hoover, C. I., Featherstone, J. D., & Gansky, S. A. (2006). Fluoride varnish efficacy in preventing early childhood caries. Journal of Dental Research, 85(2), 172–176. https://doi.org/10.1177/154405910608500211
Funding
This study was supported by the University of Washington Dr. Douglass L. Morell Dentistry Research Fund, the Lloyd and Kay Chapman Endowed Chair for Oral Health, and funding from the US National Institute of Dental and Craniofacial Research Grant No. R01DE026741.
Author information
Authors and Affiliations
Contributions
MK was responsible for the conception, analysis, and interpretation of data for the work; drafting the work; and final approval of the work. DK was responsible for conception, acquisition, analysis, and interpretation of data for the work; revising the work for critically important intellectual content; and final approval of the work. CMH was responsible for analysis and interpretation of data for the work; revising the work for critically important intellectual content; and final approval of the work. DLC was responsible for conception, acquisition, and interpretation of the work; revising the work for critically important intellectual content; and final approval of the work.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflicts of interest.
Ethical Approval
This study was approved by the University of Washington Institutional Review Board.
Consent to Participate
Prior to enrollment in this study, participants were asked to read and accept a written consent statement. All participants were offered a copy of the written statement. Written documentation of consent was not obtained.
Consent for Publication
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix A:
Survey demographics included caregiver age, gender, race, ethnicity, education, child SHCN status, and household income.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Koh, M., Kerr, D., Hill, C.M. et al. A Mixed-Methods Study on Topical Fluoride Beliefs and Refusal Behaviors for Caregivers of Children with Special Health Care Needs. Matern Child Health J 28, 104–115 (2024). https://doi.org/10.1007/s10995-023-03806-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03806-1