Abstract
Objective
Prior research suggests that children with a low socioeconomic status (SES) background are at an increased risk for special healthcare needs. Conversely, for hypersensitivity-related diseases, many studies reported a lower risk among children with lower SES according to the hygiene hypothesis. We aimed to evaluate the association between SES and several hypersensitivity diseases and autism in a representative American sample.
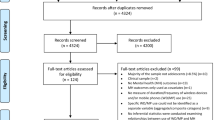
Methods
We used data from the 2016, 2017 and 2018 US National Survey of Children’s Health. A total of 102,341 children aged 0–17 years were included. The dependent variables were doctor-diagnosed allergies, arthritis, asthma, diabetes, and autism. The main SES indicators were family poverty levels, highest education of the reported adults and difficulty in family income. Our analysis used logistic regression that accounted for the survey sampling design.
Results
The sample had a mean age of 9.4 ± 5.3 years. The weighted prevalence for allergies was 24.4%, 0.3% for arthritis, 11.9% for asthma, 0.5% for diabetes and 2.6% for autism. Children with adults reporting higher educational levels had greater odds of allergies (adjusted odds ratio and 95% CI: 1.48, 1.23–1.78) than those with lower educational levels. But for all other diseases, most findings suggested that a higher odds of disease was associated with lower SES instead of higher SES.
Conclusions
A low SES background remains an important risk factor for hypersensitivity diseases in children. Most of our results suggested that children with low SES were associated with a higher risk of hypersensitivity diseases and autism.
Significance
Studies have shown that children from low SES backgrounds are at a lower risk for hypersensitivity-related diseases according to the hygiene hypothesis; however, most studies only explored one type of hypersensitivity disease at a time. We analyzed data from the 2016, 2017, and 2018 National Survey of Children’s Health and examined the association of SES with allergies, arthritis, asthma, diabetes, and autism. Except for allergies, most of our findings suggested that children with lower SES backgrounds were at an increased risk of hypersensitivity diseases and autism. Our results contradicted the notion that low SES backgrounds are protective against hypersensitivity-related diseases in children.
Similar content being viewed by others
Data Availability
Data can be accessed at the Child and Adolescent Health Measurement Initiative’s Data Resource Center for Child and Adolescent Health.
Code Availability
Codes are available upon request.
References
Becker, K. G. (2007). Autism, asthma, inflammation, and the hygiene hypothesis. Medical Hypotheses, 69(4), 731–740.
Becker, K. G. (2018). Autism and socioeconomic Status-An Immune Link? American Journal of Public Health, 108, e16.
Blanchard, L. T., Gurka, M. J., & Blackman, J. A. (2006). Emotional, developmental, and behavioral health of american children and their families: A report from the 2003 National Survey of Children’s Health. Pediatrics, 117, e1202–e1212.
Bruno, G., Spadea, T., Picariello, R., Gruden, G., Barutta, F., Cerutti, F., Cavallo-Perin, P., Costa, G., Gnavi, R., & Epidemiology Piedmont Study Group for Diabetes. (2013). Early life socioeconomic indicators and risk of type 1 diabetes in children and young adults. Journal of Pediatrics, 162, 600–05e1.
Durkin, M. S., Maenner, M. J., Baio, J., Christensen, D., Daniels, J., Fitzgerald, R., Imm, P., Lee, L. C., Schieve, L. A., Van Naarden Braun, K., Wingate, M. S., & Yeargin-Allsopp, M. (2017). Autism spectrum disorder among US children (2002–2010): Socioeconomic, racial, and ethnic disparities. American Journal of Public Health, 107, 1818–1826.
Elsabbagh, M. (2020). Linking risk factors and outcomes in autism spectrum disorder: Is there evidence for resilience? Bmj, 368, l6880.
Farfel, A., Tirosh, A., Derazne, E., Garty, B. Z., & Afek, A. (2010). Association between socioeconomic status and the prevalence of asthma. Annals of Allergy, Asthma & Immunology, 104, 490–495.
Gesundheit, B., Rosenzweig, J. P., Naor, D., Lerer, B., Zachor, D. A., Prochazka, V., & Ashwood, P. (2013). Immunological and autoimmune considerations of Autism Spectrum Disorders. Journal of Autoimmunity, 44, 1–7.
Ghandour, R. M., Jones, J. R., Lebrun-Harris, L. A., Minnaert, J., Blumberg, S. J., Fields, J., Bethell, C., & Kogan, M. D. (2018). The design and implementation of the 2016 National Survey of Children’s Health. Maternal and Child Health Journal, 22, 1093–1102.
Grieger, J. A., Clifton, V. L., Tuck, A. R., Wooldridge, A. L., Robertson, S. A., & Gatford, K. L. (2016). In utero programming of allergic susceptibility. International Archives of Allergy and Immunology, 169(2), 80–92.
Hoffmann, B., Kolahgar, B., Rauchfuss, K., Eberwein, G., Franzen-Reuter, I., Kraft, M., Wilhelm, M., Ranft, U., & Jockel, K. H. (2009). Childhood social position and associations between environmental exposures and health outcomes. International Journal of Hygiene and Environmental Health, 212, 146–156.
Hughes, H. K., Mills Ko, E., Rose, D., & Ashwood, P. (2018). Immune Dysfunction and Autoimmunity as pathological mechanisms in Autism Spectrum Disorders. Frontiers in Cellular Neuroscience, 12, 405.
Ko, Y., Kariyawasam, V., Karnib, M., Butcher, R., Samuel, D., Alrubaie, A., Rahme, N., McDonald, C., Cowlishaw, J., Katelaris, P., Barr, G., Jones, B., Connor, S., Paven, G., Chapman, G., Park, G., & Gearry, R., R. W. Leong, and I. B. D. Sydney Organisation. (2015). ‘Inflammatory Bowel Disease Environmental Risk Factors: A Population-Based Case-Control Study of Middle Eastern Migration to Australia’, Clinical Gastroenterology and Hepatology, 13: 1453–63e1.
Loprest, P., & Davidoff, A. (2004). How children with special health care needs affect the employment decisions of low-income parents. Maternal and Child Health Journal, 8, 171–182.
McPherson, M., Arango, P., Fox, H., Lauver, C., McManus, M., Newacheck, P. W., Perrin, J. M., Shonkoff, J. P., & Strickland, B. (1998). ‘A new definition of children with special health care needs’, Pediatrics, 102: 137 – 40.
Newacheck, P. W., Rising, J. P., & Kim, S. E. (2006). ‘Children at risk for special health care needs’, Pediatrics, 118: 334 – 42.
Newacheck, P. W., Kim, S. E., Blumberg, S. J., & Rising, J. P. (2008). ‘Who is at risk for special health care needs: findings from the National Survey of Children’s Health’, Pediatrics, 122: 347 – 59.
Okada, H., Kuhn, C., Feillet, H., & Bach, J. F. (2010). The ‘hygiene hypothesis’ for autoimmune and allergic diseases: An update. Clinical and Experimental Immunology, 160, 1–9.
Pearce, N., & Douwes, J. (2006). The latin american exception: Why is childhood asthma so prevalent in Brazil? J Pediatr (Rio J), 82, 319–321.
Pearce, N., Ait-Khaled, N., Beasley, R., Mallol, J., Keil, U., Mitchell, E., Robertson, C., & Isaac Phase Three Study Group. (2007). Worldwide trends in the prevalence of asthma symptoms: Phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax, 62, 758–766.
Sonnenschein-van der Voort, A. M., Arends, L. R., de Jongste, J. C., Annesi-Maesano, I., Arshad, S. H., Barros, H., & Duijts, L. (2014). Preterm birth, infant weight gain, and childhood asthma risk: A meta-analysis of 147,000 european children. The Journal of Allergy and Clinical Immunology, 133(5), 1317–1329.
Spencer, N. J., Blackburn, C. M., & Read, J. M. (2015). Disabling chronic conditions in childhood and socioeconomic disadvantage: A systematic review and meta-analyses of observational studies. British Medical Journal Open, 5, e007062.
Strachan, D. P. (1989). Hay fever, hygiene, and household size. Bmj, 299, 1259–1260.
Subbarao, P., Mandhane, P. J., & Sears, M. R. (2009). ‘Asthma: epidemiology, etiology and risk factors’, CMAJ, 181: E181-90.
U.S. Census Bureau (2019). ‘2018 National Survey of Children’s Health, Methodology Report’, Accessed December 1, 2022. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/2018-NSCH-Methodology-Report.pdf.
U.S. Census Bureau. (2020a). ‘National Survey of Children’s Health, Guide to Multi-Year Analysis’, Accessed December 1, 2022. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/NSCH-Guide-to-Multi-Year-Estimates.pdf.
U.S. Census Bureau (2020b). ‘National Survey of Children’s Health, Guide to Multiply Imputed Data Analysis’, Accessed December 1, 2022. https://www2.census.gov/programs-surveys/nsch/technical-documentation/methodology/NSCH-Analysis-with-Imputed-Data-Guide.pdf.
Uphoff, E., Cabieses, B., Pinart, M., Valdes, M., Anto, J. M., & Wright, J. (2015). A systematic review of socioeconomic position in relation to asthma and allergic diseases. European Respiratory Journal, 46, 364–374.
van Dyck, P. C., Kogan, M. D., McPherson, M. G., Weissman, G. R., & Newacheck, P. W. (2004). Prevalence and characteristics of children with special health care needs. Archives of Pediatrics and Adolescent Medicine, 158, 884–890.
Acknowledgements
This project was supported by the Ministry of Health and Welfare in Taiwan. The content is solely the responsibility of the authors and does not represent the official views of the funders.
Funding
This study was supported by the Ministry of Health and Welfare in Taiwan.
Author information
Authors and Affiliations
Contributions
Both Authors (TJW and TY) contributed to the design, analysis, interpretation and manuscript writing of this study.
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethics Approval
This is a secondary analysis of publicly available data and was exempt by ethics board review.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wong, TJ., Yu, T. Association Between Socioeconomic Status and Prevalence of Hypersensitivity Diseases and Autism: A Nationwide Study of Children. Matern Child Health J 27, 2194–2202 (2023). https://doi.org/10.1007/s10995-023-03789-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10995-023-03789-z