Abstract
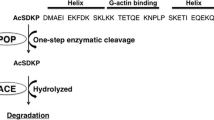
Angiotensin converting enzyme inhibitor is a one of the best anti-hypertension well known drugs for treatment of hypertension (Cushman and Ondetti, Hypertension 17:589–592, 1991). In available ACE inhibitors have various side effects like angioedema, dry cough, skin irritation, and multiple dosing due to less bioavailability (Natesh et al., Nature 421:551–554, 2003, Natesh et al., Biochemistry 43:8718–8724, 2004). We had previously published the data for pharmacological profile and potency of a peptidomimetic compound, 3-Thienylalanine-Ornithine-Proline (TOP) is in-house compound. TOP has shown potent activity and a promising profile in in-vitro, ex-vivo and in-vivo assays as published previously from our laboratory (Seth et al., Drug Des Devel Ther, 2016, Chaudhary et al., J Cardiovasc Pharmacol 61:311–317, 2013). The potent and interesting pharmacological activity shown by this compound further forced us to look at the toxicological profile of this compound in in-vivo in sub-chronic dosing in different dose regime above its pharmacological dose. Therefore, in the current study, we aimed to evaluate the toxicity study that is the 28 days toxicity of our inhouse compound TOP applying the recommended OECD guidelines for safety. In this study, we have taken the dose 10 times higher dose than effective dose. However, our compound (TOP) did not show any toxic sign and symptom and no significantly adverse effect in blood chemistry, hematologic values and histology till higher dose 100 mg/kg. In conclusion, in this study TOP showed promising pharmacological activity without any signs of toxicity in animals.






Similar content being viewed by others
References
ALLHAT Officers and Coordinators for the ALLHAT Collaborative Research Group. The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (2002) Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT). JAMA 288(23):2981–2997
Al-Mamary M, Al-Habori M, Al-AghbariAM BMM (2002) Investigation into the toxicological effects of Catha edulis leaves: a short -term study in animals. Phytother Res 16:127–132
Androulakis ES et al (2009) Essential hypertension: is there a role for inflammatory mechanisms. Cardiol Rev 17(5):216–221
Anon (1999) Canadian led landmark study demonstrates ACE inhibitor ramipril reduces risk of cardiovascular death and life-threatening events. Can J Cardiol 15(9):1027
Bala M, Gupta S, Pasha MAQ (2000) Angiotensin converting enzyme assay optimization: Influence of various buffers and their concentrations. Clin Biochem 33:687–689
Bala M, Qadar Pasha MA, Bhardwaj DK (2002) Novel peptidomimics as angiotensin converting enzyme inhibitors: a combinatorial approach. Bioorg Med Chem 10:3685–3691
Ball SG, Hall AS (1994) What to expect from ACE inhibitors after myocardial infarction. Br Heart J 72(suppl):S70–S74
Ball SG, Hall AS, Murray GD (1995) Angiotensin-converting enzyme inhibitors after myocardial infarction: indications and timing. J Am Coll Cardiol 25(Suppl 7):42S
Barlos K, Gatos D, Kutsogianni S, Papaphotiou G, Poulos C, Segenidis T (1991) Solid phase synthesis of partially protected and free peptides containing disulphide bonds by simultaneous cysteine oxidation-release from 2-chlorotrityl resin. Int J Peptides Protein Res 38:555
Beelay N (1994) Peptidomimetics and small- molecule drug design: towards improved bio-availability and in-vivo stability. Tibtech 12:213–216
Bernátová I, Pecháňová O, Šimko F (1999a) Effect of captopril in L-NAME-induced hypertension on the rat myocardium, aorta, brain and kidney. Exp Physiol 84:1095–1105
Bernátová I, Pecháňová O, Šimko F (1999b) Effect of captopril in L-NAME-induced hypertension on the rat myocardium, aorta, brain and kidney. Exp Physiol 84:1095–1105
Bilazarian SD, Currier JW, Haudenschild C, Heyman D, Powell J, Ryan TJ, Faxon DP (1990) Angiotensin converting enzyme inhibition reduces restenosis in experimental angioplasty. Circulation 17(2S1):82–297
Bodanszky M (1985) In search of new methods in peptide synthesis. Int J Pep Prot Res M 25:449
Brown NJ, Vaughan DE (1998) Angiotensin-converting enzyme inhibitors. Circulation 97:1411–1420
Buccafusco JJ (1996) The role of central cholinergic neurons in the regulation of blood pressure and in experimental hypertension. Pharmacol Rev 48:179–211
Burger D, Nishigaki N, Touyz RM (2010) New insights into molecular mechanisms of hypertension. Curr Opin Nephrol Hypertens 19(2):160–162
Burt VL, Whelton P, Roccella EJ, Brown C, Cutler JA, Higgins M, Horan MJ, Labarthe D (1995) Prevalence of hypertension in the US adult population. Results from the third national health and nutrition examination survey 1988–1991. Hypertension. https://doi.org/10.1161/01.hyp.25.3.305
Bustin SA (2000) Absolute quantification of mRNA using real-time reverse transcription polymerase chain reaction assays. J Mol Endocrinol 25:169–193
Bustin SA (2002) Quantification of mRNA using real-time reverse transcription PCR (RT-PCR): trends and problems. J Mol Endocrinol 29:23–39
Butwell FGW, Epton R, Mclaren JV, Small PW, Welling DA (1985) Gel phase 13C nmr spectroscopy as a method of analytical control in ultra high loads solid (gel) phase peptides synthesis with special reference to LH-RH. In: Deber CM, Hruby VJ, Kopple KD (eds) Peptides: structure and Function. Pierce Chemical co, Rockford, p 273
Cai H, Harrison DG (2000) Endothelial dysfunction in cardiovascular diseases: The role of oxidant stress. Circ Res 87:840–844
Campbell DJ (2006) L-NAME hypertension: trying to fit the pieces together. J Hypertens 24(1):33–36
Campese VM et al (2004) Reactive oxygen species stimulate central and peripheral sympathetic nervous system activity. Am J Physiol Heart Circ Physiol 287(2):H695-703
Carretero OA, Oparil S (2000) Essential hypertension. Part I: definition and etiology. Circulation 101(3):329–335
Chaudhary S, Seth MK, Vats ID, Kumar K, Biswas P, Karar J, Hussain ME, Pasha MA, Pasha S (2013) Sulfur-containingangiotensin-convertingenzymeinhibitor3-thienylalanine-ornithyl-proline activates endothelial function and expression of genes involved in Renin-Angiotensin system. J Cardiovasc Pharmacol 61(4):311–317
Chisolm GM, Steinberg D (2000) The oxidative modification hypothesis of atherogenesis: an overview. Free RadicBiol Med 28(12):1815–1826
Chobanian AV, Brecher PI, Handenschild CC (1986) The effects of hypertension and antihypertensive therapy on atherosclerosis. Hypertension 8(suppl 1):15–21
Chobanian AV, Haudenschild CC, Nickerson C, Drago R (1990) Antiatherogenic effect of captopril in the Watanabe heritable hyperlipidemic rabbit. Hypertension 15:327–331
Choi KM, Park HS, Han JH, Lee JS, Lee J, Ryu OH, Kim SM (2006) Prevalence of prehypertension and hypertension in a Korean population: Korean National Health and Nutrition Survey 2001. J Hypertens 24(8):1515–1521
Cushman DW, Ondetti MA (1991) History of design of captopril and related inhibitors of angiotensin-converting enzyme. Hypertension 17:589–592
Dabiré H, Barthélémy I, Blanchard-Gutton N, Sambin L, Sampedrano CC, Gouni V, Unterfinger Y, Aguilar P, Thibaud JL, Ghaleh B, Bizé A, Pouchelon JL, Blot S, Berdeaux A, Hittinger L, Chetboul V, Su JB (2012) Vascular endothelial dysfunction in Duchenne muscular dystrophy is restored by bradykinin through upregulation of eNOS and nNOS. Basic Res Cardiol 107(1):1–9
Das S, Vasisht S, Das SN, Srivastava LM (2000) Correlation between total antioxidant status and lipid peroxidation in hypercholesterolaemia. Curr Sci 78:486
Davis S, Granner D (2001) Insulin, oral hypoglycemic agents, and the pharmacology of the endocrine pancreas. In: Hardman JG, Limbird LE (eds) Goodman and Gilman’s T Pharmacological Basis of Therapeutics. McGraw Hill, NewYork, pp 1679–1714
Dikalova A, Clempus R, Lassegue B, Cheng G, McCoy J, Dikalov S (2005) Nox1 overexpression potentiates angiotensin II-induced hypertension and vascular smooth muscle hypertrophy in transgenic mice. Circulation 112:2668–2676
Hagley MT, Hulisz DT, Burns CM (1993) Hepatotoxicity associated with angiotensin-converting enzyme inhibitors. Ann Pharmacother 27(2):228–231
Hsieh NK, Wang JY, Liu JC, Wang SD, Chen HI (2004) Nitric oxide inhibition accelerates hypertension and induces perivascular inflammation in rats. Clin Exp Pharmacol Physiol 31:212–218
Natesh R, Schwager SL, Sturrock ED, Acharya KR (2003) Crystal structure of the human angiotensin-converting enzyme-lisinopril complex. Nature 421:551–554
Natesh R, Schwager SL, Evans HR, Sturrock ED, Acharya KR (2004) Structural details on the binding of antihypertensive drugs captopril and enalaprilat to human testicular angiotensin-I converting enzyme. Biochemistry 43:8718–8724
Oktem F, Kirbas A, Armagan A, Kuybulu AE, Yilmaz HR, Ozguner F, Uz E (2011) Lisinopril attenuates renal oxidative injury in L-NAME-induced hypertensive rats. Mol Cell Biochem 352(1–2):247–253
Pavar MC, Hanif K, Azam A, Lata S, Qadar Pasha MA, Pasha S (2006) Structure-activity relationship study between Ornithyl-Proline and Lysyl-Proline based tripeptidomimics as angiotensin-converting enzyme inhibitors. Bioorg Med Chem Lett 16(8):2117–2121
Pohl U (1993) Role of endothelium-derived nitric oxide in the control of local blood flow under physiological and pathophysiological conditions. Can J Cardiol 9(suppl C):6C–1lC
Seth MK, Hussain ME, Pasha S, Fahim M (2016) Effects of a novel ACE inhibitor, 3-(3-thienyl)-l-alanyl-ornithyl-proline, on endothelial vasodilation and hepatotoxicity in l-NAME-induced hypertensive rats. Drug Des Devel Ther. https://doi.org/10.2147/DDDT.S77761
Syed AA et al (2016) Evaluation of anti-hypertensive activity of Ulmuswallichiana extract and fraction in SHR, DOCA-salt- and L-NAME-induced hypertensive rats. J Ethnopharmaco 193:555–565
Vats ID, Snehlata NM, Pasha MAQ, Pasha S (2009) Effect of chronic intra-peritoneally administered chimeric peptide of met-enkephalin and FMRFa-[D-Ala2] YFa on antinociception and opioid receptor regulation. Eur J Pain 14(3):295
Vercruysse L, Morel N, Camp JV, Szust J, Smagghe G (2008) Antihypertensive mechanism of the dipeptide Val-Tyr in rat aorta. Peptides 29:261–267
Zicha J, Dobešová Z, Kuneš J (2006) Antihypertensive mechanisms of chronic captopril or N-acetylcysteine treatment in L-NAME hypertensive rats. Hypertens Res 29:1021–1027
Acknowledgements
This study was supported by the Council of Scientific and Industrial Research, India.
Author information
Authors and Affiliations
Contributions
Mahesh Kumar Seth, I (Mahesh Kumar Seth) am corresponding author and all experiment performed by me with the help of co-authors i.e. Rakesh Kumar Singh, M Ejaz Hussain, Santosh Pasha, Mohammad Fahim and All co- authors reviewed the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest in this work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Seth, M.K., Singh, R.K., Hussain, M. et al. Toxicity Study of 3-Thienylalanine- Ornithine-Proline (TOP) Using as Novel ACE Inhibitor. Int J Pept Res Ther 28, 150 (2022). https://doi.org/10.1007/s10989-022-10449-3
Accepted:
Published:
DOI: https://doi.org/10.1007/s10989-022-10449-3