Abstract
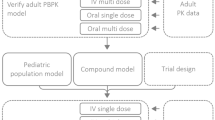
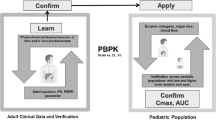
The project SAFEPEDRUG aims to provide guidelines for drug research in children, based on bottom-up and top-down approaches. Propofol, one of the studied model compounds, was selected because it is extensively metabolized in liver and kidney, with an important role for the glucuronidation pathway. Besides, being a lipophilic molecule, it is distributed into fat tissues, from where it redistributes into the systemic circulation. In the past, both bottom-up (Physiologically based pharmacokinetic, PBPK) and top-down approaches (population pharmacokinetic, popPK) were applied to describe its pharmacokinetics (PK). In this work, a combination of the two was used to check their performance to describe PK in children and neonates (both term and preterm) using propofol as a case compound. First, in vitro data was generated in human liver microsomes and recombinant enzymes and used to develop an adult PBPK model in Simcyp®. Activity adjustment factors (AAFs) were calculated to account for differences between in vitro and in vivo enzyme activity. Clinical data were analyzed using a 3-compartment model in NONMEM. These data were used to construct a retrograde PBPK model and for qualification of the PBPK models. Once an accurate in vivo clearance was obtained accounting for the contribution of the different metabolic pathways, the resulting PBPK models were challenged with new data for qualification. After that, the constructed adult PPBK model for propofol was extrapolated to the pediatric population. Both the default built-in and in vivo derived ontogeny functions were used to do so. The models were qualified by comparing their predicted PK parameters to published values, and by comparison of predicted concentration–time profiles to available clinical data. Clearance values were predicted well, especially when compared with values obtained from trials where long-term sampling was applied, whereas volume of distribution was lower compared to the most common popPK model predictions. Concentration–time profiles were predicted well up until and including the preterm neonatal population. In this work, it was thus shown that PBPK can be used to predict the PK up to and including the preterm neonatal population without the use of pediatric in vivo data. This work adds weight to the need for further development of PBPK models, especially regarding distribution modeling and the use of in vivo derived ontogeny functions.








Similar content being viewed by others
Abbreviations
- 4HP:
-
4-Hydroxy propofol
- AAF:
-
Activity adjustment factor
- CL int :
-
Intrinsic clearance
- CL int,u :
-
Unbound intrinsic clearance
- CYP:
-
Cytochrome P450
- HLM:
-
Human liver microsomes
- HKM:
-
Human kidney microsomes
- IVIVE:
-
In vitro in vivo extrapolation
- MPPGK:
-
Microsomal protein per gram kidney
- MPPGL:
-
Microsomal protein per gram liver
- PBPK:
-
Physiologically based pharmacokinetics
- PG:
-
Propofol glucuronide
- PopPK:
-
Population pharmacokinetics
- rhCYP:
-
Recombinant human CYP
- rhUGT:
-
Recombinant human UGT
- UGT:
-
Uridine 5′-diphospho-glucuronosyltransferase
- SPE:
-
Solid phase extraction
References
Rocchi F, Tomasi P (2011) The development of medicines for children. Pharmacol Res 64:169–175. https://doi.org/10.1016/j.phrs.2011.01.016
Bryson HM, Fulton BR, Faulds D (1995) Propofol. An update of its use in anaesthesia and conscious sedation. Drugs 50:513–559
Simons PJ, Cockshott ID, Douglas EJ, Gordon E, Hopkins K, Rowland M (1988) Disposition in male volunteers of a subanaesthetic intravenous dose of an oil in water emulsion of 14c-propofol. Xenobiotica 18:429–440. https://doi.org/10.3109/00498258809041679
Favetta P, Degoute CS, Perdrix JP, Dufresne C, Boulieu R, Guitton J (2002) Propofol metabolites in man following propofol induction and maintenance. Br J Anaesth 88:653–658. https://doi.org/10.1093/bja/88.5.653
Eleveld DJ, Proost JH, Cortínez LI, Absalom AR, Struys MMRF, Cortínez LI, Absalom AR, Struys MMRF (2014) A general purpose pharmacokinetic model for propofol. Anesth Analg 118:1221–1237. https://doi.org/10.1213/ane.0000000000000165
Schüttler J, Ihmsen H (2000) Population pharmacokinetics of propofol. Anesthesiology 92:727–738. https://doi.org/10.1097/00000542-200003000-00017
Peeters MYM, Pharm D, Prins SA, Knibbe CAJ, Ph D (2006) Propofol pharmacokinetics and pharmacodynamics for depth of sedation in nonventilated infants after major craniofacial surgery. Anesthesiology 104:466–474
Abad-Santos F, Gálvez-Múgica MA, Santos MA, Novalbos J, Gallego-Sandín S, Méndez P, Casimiro C, Gilsanz F, Gallego-Sandín S, Méndez P, Casimiro C, Gilsanz F (2003) Pharmacokinetics and pharmacodynamics of a single bolus of propofol 2% in healthy volunteers. J Clin Pharmacol 43:397–405. https://doi.org/10.1177/0091270003251391
Raoof AA, Van Obbergh LJ, De Ville De Goyet J, Verbeeck RK (1996) Extrahepatic glucuronidation of propofol in man: possible contribution of gut wall and kidney. Eur J Clin Pharmacol 50:91–96. https://doi.org/10.1007/s002280050074
Gill KL, Houston JB, Galetin A (2012) Characterization of in vitro glucuronidation clearance of a range of drugs in human kidney microsomes: comparison with liver and intestinal glucuronidation and impact of albumin. Drug Metab Dispos
Gill KL, Gertz M, Houston JB, Galetin A (2013) Application of a physiologically based pharmacokinetic model to assess propofol hepatic and renal glucuronidation in isolation: utility of in vitro and in vivo data. Drug Metab Dispos 41:744–753. https://doi.org/10.1124/dmd.112.050294
Gu J, Lu K, Xia P, Tang M, Dai Q, Ma D, Tao G (2009) Pharmacokinetics of propofol and extrahepatic ugt1a6 gene expression in anhepatic rats. Pharmacology 84:219–226. https://doi.org/10.1159/000236523
Hiraoka H, Yamamoto K, Miyoshi S, Morita T, Nakamura K, Kadoi Y, Kunimoto F, Horiuchi R (2005) Kidneys contribute to the extrahepatic clearance of propofol in humans, but not lungs and brain. Br J Clin Pharmacol 60:176–182. https://doi.org/10.1111/j.1365-2125.2005.02393.x
Al-Jahdari WS, Yamamoto K, Hiraoka H, Nakamura K, Goto F, Horiuchi R (2006) Prediction of total propofol clearance based on enzyme activities in microsomes from human kidney and liver. Eur J Clin Pharmacol 62:527–533. https://doi.org/10.1007/s00228-006-0130-2
Allegaert K, Vancraeynest J, Rayyan M, de Hoon J, Cossey V, Naulaers G, Verbesselt R (2008) Urinary propofol metabolites in early life after single intravenous bolus. Br J Anaesth 101:827–831. https://doi.org/10.1093/bja/aen276
Tsamandouras N, Rostami-Hodjegan A, Aarons L (2013) Combining the “bottom-up” and “top-down” approaches in pharmacokinetic modelling: fitting pbpk models to observed clinical data. Br J Clin Pharmacol 79:16. https://doi.org/10.1111/bcp.12234
Rostami-hodjegan A (2017) Reverse translation in pbpk and qsp : going backwards in order to go forward with confidence. Clin Pharmacol Ther. https://doi.org/10.1002/cpt.904
Zhuang X, Lu C (2016) PBPK modeling and simulation in drug research and development. Acta Pharm Sin B 6:430–440. https://doi.org/10.1016/j.apsb.2016.04.004
Nestorov I (2003) Whole body pharmacokinetic models. Clin Pharmacokinet 42:883–908. https://doi.org/10.2165/00003088-200342100-00002
Barrett JS, Della Casa Alberighi O, Läer S, Meibohm B (2012) Physiologically based pharmacokinetic (pbpk) modeling in children. Clin Pharmacol Ther 92:40–49. https://doi.org/10.1038/clpt.2012.64
Khalil F, Läer S (2014) Physiologically based pharmacokinetic models in the prediction of oral drug exposure over the entire pediatric age range-sotalol as a model drug. AAPS J 16:226–239. https://doi.org/10.1208/s12248-013-9555-6
Teorell T (1937) Kinetics of distribution of substances administered to the body. Arch Int Pharmacodyn Thérapie 57:205–240
Edginton AN, Schmitt W, Willmann S, Edginton A (2006) Application of physiology-based pharmacokinetic and pharmacodynamic modeling to individualized target-controlled propofol infusions. Adv Ther 23:143–158
Mahmood I, Ahmad T, Mansoor N, Sharib SM (2016) Prediction of clearance in neonates and infants (less than 3 months of age) for drugs that are glucuronidated: a comparative study between allometric scaling and physiologically based pharmacokinetic modeling. J Clin Pharmacol 57:476
T’jollyn H, Snoeys J, van Bocxlaer J, de Bock L, Annaert P, van Peer A, Allegaert K, Mannens G, Vermeulen A, Boussery K (2016) Strategies for determining correct cytochrome p450 contributions in hepatic clearance predictions: in vitro–in vivo extrapolation as modelling approach and tramadol as proof-of concept compound. Eur J Drug Metab Pharmacokinet. https://doi.org/10.1007/s13318-016-0355-0
Johnson TN, Rostami-Hodjegan A, Tucker GT (2006) Prediction of the clearance of eleven drugs and associated variability in neonates, infants and children. Clin Pharmacokinet 45:931–956. https://doi.org/10.2165/00003088-200645090-00005
T’jollyn H, Vermeulen A, Boussery K, Bocxlaer AJ Van (2017) Characterizing hepatic clearance in early life: pbpk as modeling tool and tramadol as guide. Ghent University
Nagar S, Argikar UA, Tweedie DJ (2014) Enzyme kinetics in drug metabolism. Humana Press, Totowa
Peng M, Le J, Yang Y (2013) Simultaneous determination of 11 related impurities in propofol by gas chromatography/tandem mass spectrometry coupled with pulsed splitless injection technique. J Sep Sci 36:1959–1966. https://doi.org/10.1002/jssc.201300075
Food and Drug Administration (FDA) (2001) Guidance for industry: bioanalytical method validation. Maryland
Knights KM, Rowland A, Miners JO (2013) Renal drug metabolism in humans: the potential for drug-endobiotic interactions involving cytochrome p450 (cyp) and udp-glucuronosyltransferase (ugt). Br J Clin Pharmacol 76:587–602. https://doi.org/10.1111/bcp.12086
Jamei M, Marciniak S, Feng K, Barnett A (2009) The simcyp® population-based adme simulator. Expert Opin drug Metab Toxicol 5:211–223
Barter ZE, Tucker GT, Rowland-Yeo K (2013) Differences in cytochrome p450-mediated pharmacokinetics between chinese and caucasian populations predicted by mechanistic physiologically based pharmacokinetic modelling. Clin Pharmacokinet 52:1085–1100. https://doi.org/10.1007/s40262-013-0089-y
Barnes KJ, Rowland A, Polasek TM, Miners JO (2014) Inhibition of human drug-metabolising cytochrome p450 and udp-glucuronosyltransferase enzyme activities in vitro by uremic toxins. Eur J Clin Pharmacol 70:1097–1106. https://doi.org/10.1007/s00228-014-1709-7
Veroli P, O’Kelly B, Bertrand F, Trouvin JH, Faranotti R, Ecoffey C (1992) Extrahepatic metabolism of propofol in man during the anhepatic phase of orthotopic liver transplantation. Br J Anaesth 68:183–186. https://doi.org/10.1093/bja/68.2.183
Eugene AR (2017) CYP2B6 genotype guided dosing of propofol anesthesia in the elderly based on nonparametric population pharmacokinetic modeling and simulations. Int J Clin Pharmacol Toxicol 6:242–249. https://doi.org/10.1038/nbt.3121.ChIP-nexus
Kansaku F, Kumai T, Sasaki K, Yokozuka M, Shimizu M, Tateda T, Murayama N, Kobayashi S, Yamazaki H (2011) Individual differences in pharmacokinetics and pharmacodynamics of anesthetic agent propofol with regard to cyp2b6 and ugt1a9 genotype and patient age. Drug Metab Pharmacokinet 26:532–537. https://doi.org/10.2133/dmpk.DMPK-11-RG-039
Guitton J, Buronfosse T, Desage M, Flinois JP, Perdrix JP, Brazier JL, Beaune P (1998) Possible involvement of multiple human cytochrome p450 isoforms in the liver metabolism of propofol. Br J Anaesth 80:788–795. https://doi.org/10.1093/bja/80.6.788
Restrepo JG, Garcia-Martín E, Martínez C, Agúndez JAG (2009) Polymorphic drug metabolism in anaesthesia. Curr Drug Metab 10:236–246. https://doi.org/10.2174/138920009787846305
Court MH, Duan SX, Hesse LM, Venkatakrishnan K, Greenblatt DJ (2001) Cytochrome p-450 2b6 is responsible for interindividual variability of propofol hydroxylation by human liver microsomes. Anesthesiology 94:110–119. https://doi.org/10.1097/00000542-200101000-00021
Mikstacki A, Zakerska-Banaszak O, Skrzypczak-Zielinska M, Tamowicz B, Prendecki M, Dorszewska J, Molinska-Glura M, Waszak M, Slomski R (2016) The effect of ugt1a9, cyp2b6 and cyp2c9 genes polymorphism on individual differences in propofol pharmacokinetics among polish patients undergoing general anaesthesia. J Appl Genet. https://doi.org/10.1007/s13353-016-0373-2
Tateishi T, Nakura H, Asoh M, Watanabe M, Tanaka M, Kumai T, Takashima S, Imaoka S, Funae Y, Yabusaki Y, Kamataki T, Kobayashi S (1997) A comparison of hepatic cytochrome p450 protein expression between infancy and postinfancy. Life Sci 61:2567–2574. https://doi.org/10.1016/S0024-3205(97)01011-4
Croom EL, Stevens JC, Hines RN, Wallace AD, Hodgson E (2009) Human hepatic cyp2b6 developmental expression: the impact of age and genotype. Biochem Pharmacol 78:184–190. https://doi.org/10.1016/j.bcp.2009.03.029
Treluyer J-M, Gueret G, Cheron G, Sonnier M, Cresteil T (1997) Developmental expression of cyp2c and cyp2c-dependent activities in the human liver: in vivo/in vitro correlation and inducibility. Pharmacogenetics 7:441–452. https://doi.org/10.1097/00008571-199712000-00002
Hines RN (2007) Ontogeny of human hepatic cytochromes p450. J Biochem Mol Toxicol 21:169–175. https://doi.org/10.1002/jbt.20179
Koukouritaki SB, Manro JR, Marsh SA, Stevens JC, Rettie AE, McCarver DG, Hines RN (2003) Developmental expression of human hepatic cyp2c9 and cyp2c19. J Pharmacol Exp Ther 308:965–974. https://doi.org/10.1124/jpet.103.060137
Strassburg CP, Strassburg A, Kneip S, Barut A, Tukey RH, Rodeck B, Manns MP (2002) Developmental aspects of human hepatic drug glucuronidation in young children and adults. Gut 50:259–265. https://doi.org/10.1136/gut.50.2.259
Michelet R, Van Bocxlaer J, Vermeulen A (2017) PBPK in preterm and term neonates: a review. Curr Pharm Des. https://doi.org/10.2174/1381612823666171009143840
Somani A, Thelen K, Zheng S, Trame MN, Coboeken K, Meyer M, Schnizler K, Ince I, Willmann S, Schmidt S (2015) Evaluation of changes in oral drug absorption in preterm and term neonates for biopharmaceutics classification system (bcs) class i and ii compounds. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.12752
Mooij MG, de Koning BAE, Lindenbergh-Kortleve DJ, Simons-Oosterhuis Y, van Groen BD, Tibboel D, Samsom JN, de Wildt SN (2016) Human intestinal pept1 transporter expression and localization in preterm and term infants. Drug Metab Dispos. https://doi.org/10.1124/dmd.115.068809
George I, Mekahli D, Rayyan M, Levtchenko E, Allegaert K (2011) Postnatal trends in creatinemia and its covariates in extremely low birth weight (elbw) neonates. Pediatr Nephrol 26:1843–1849. https://doi.org/10.1007/s00467-011-1883-0
Upreti VV, Wahlstrom JL (2016) Meta-analysis of hepatic cytochrome p450 ontogeny to underwrite the prediction of pediatric pharmacokinetics using physiologically based pharmacokinetic modeling. J Clin Pharmacol 56:266–283. https://doi.org/10.1002/jcph.585
Campbell G, Morgan D, Kumar K, Crankshaw D (1988) Extended blood collection period required to define distribution and elimination kinetics of propofol. Br J Clin Pharmacol 26:187–190. https://doi.org/10.1111/j.1365-2125.1988.tb03386.x
Smuszkiewicz P, Wiczling P, Przybyłowski K, Borsuk A, Trojanowska I, Paterska M, Matysiak J, Kokot Z, Grześkowiak E, Bienert A (2016) The pharmacokinetics of propofol in icu patients undergoing long-term sedation. Biopharm Drug Dispos 37:456–466. https://doi.org/10.1002/bdd.2028
Joubert KE (2009) Computer simulations of propofol infusions for total intravenous anaesthesia in dogs. J S Afr Vet Assoc 80:2–9. https://doi.org/10.4102/jsava.v80i1.161
Morgan D, Campbell G, Crankshaw D (1990) Pharmacokinetics of propofol when given by intravenous infusion. Br J Clin Pharmacol 30:144–148. https://doi.org/10.1111/j.1365-2125.1990.tb03755.x
Bauer R (2010) NONMEM users guide: introduction to nonmem 7. ICON Dev. Solut. Ellicott City, MD 1–61
European Medicines Agency (2016) Guideline on the qualification and reporting of physiologically based pharmacokinetic (pbpk) modelling and simulation 44:1–18
Musther H, Gill KL, Chetty M, Rostami-Hodjegan A, Rowland M, Jamei M (2015) Are physiologically based pharmacokinetic models reporting the right cmax? central venous versus peripheral sampling site. AAPS J. https://doi.org/10.1208/s12248-015-9796-7
Allegaert K, Peeters MY, Verbesselt R, Tibboel D, Naulaers G, de Hoon JN, Knibbe C (2007) Inter-individual variability in propofol pharmacokinetics in preterm and term neonates. Br J Anaesth 99:864–870. https://doi.org/10.1093/bja/aem294
Wang C, Peeters MYM, Allegaert K, Blussé Van Oud-Alblas HJ, Krekels EHJ, Tibboel D, Danhof M, Knibbe CAJ (2012) A bodyweight-dependent allometric exponent for scaling clearance across the human life-span. Pharm Res 29:1570–1581. https://doi.org/10.1007/s11095-012-0668-x
Wang C, Allegaert K, Peeters MYM, Tibboel D, Danhof M, Knibbe CAJ (2014) The allometric exponent for scaling clearance varies with age: a study on seven propofol datasets ranging from preterm neonates to adults. Br J Clin Pharmacol 77:149–159. https://doi.org/10.1111/bcp.12180
Kobayashi Y, Yokozuka M, Miyakawa H, Watanabe M, Kumai T, Tateda T (2015) Effects of genetic polymorphism of cyp2b6 and ugt1a9 and sex differences on pharmacokinetics of propofol. J St Marian Univ 6:183–193. https://doi.org/10.17264/stmarieng.6.183
Oda Y, Hamaoka N, Hiroi T, Imaoka S, Hase I, Tanaka K, Funae Y, Ishizaki T, Asada A (2001) Involvement of human liver cytochrome p4502b6 in the metabolism of propofol. Br J Clin Pharmacol 51:281–285. https://doi.org/10.1046/j.1365-2125.2001.00344.x
Burgess KS, Ipe J, Swart M, Metzger IF, Lu J, Gufford BT, Thong N, Desta Z, Gaedigk R, Pearce R, Gaedigk A, Liu Y, Skaar TC (2017) Variants in the cyp2b6 3’utr alter in vitro and in vivo cyp2b6 activity: potential role of micrornas. Clin Pharmacol Ther. https://doi.org/10.1002/cpt.892
Turner M, Affonso A, Fudin J, Rivera W, Turpeinen M, Raunio H, Pelkonen O (2001) Clinical case study the functional role of cyp2b6 in human drug metabolism: substrates and inhibitors in vitro, in vivo and in silico. Am J Hosp Palliat care 18:429–431
Kirkpatrick T, Cockshott ID, Douglas EJ, Nimmo WS (1988) Pharmacokinetics of propofol (diprivan) in elderly patients. Br J Anaesth 60:146–150. https://doi.org/10.1093/bja/60.2.146
Samant TS, Mangal N, Lukacova V, Schmidt S (2015) Quantitative clinical pharmacology for size and age scaling in pediatric drug development: a systematic review. J Clin Pharmacol 55:1207
Maharaj AR, Edginton AN (2014) Physiologically based pharmacokinetic modeling and simulation in pediatric drug development. CPT Pharmacomet Syst Pharmacol 3:e150. https://doi.org/10.1038/psp.2014.45
Edginton AN, Schmitt W, Willmann S (2006) Application of physiology-based pharmacokinetic and pharmacodynamic modeling to individualized target-controlled propofol infusions. Adv Ther 23:143–158. https://doi.org/10.1007/BF02850355
Kawai R, Mathew D, Tanaka C, Rowland M (1998) Physiologically based pharmacokinetics of cyclosporine a: extension to tissue distribution kinetics in rats and scale-up to human. J Pharmacol Exp Ther 287:457–468
Gaohua L, Wedagedera J, Small BG, Almond L, Romero K, Hermann D, Hanna D, Jamei M, Gardner I (2015) Development of a multicompartment permeability-limited lung pbpk model and its application in predicting pulmonary pharmacokinetics of antituberculosis drugs. CPT Pharmacomet Syst Pharmacol 4:605–613. https://doi.org/10.1002/psp4.12034
Miyagi SJSJ, Milne AMAM, Coughtrie MWH, Collier AC (2012) Neonatal development of hepatic ugt1a9: implications of pediatric pharmacokinetics. Drug Metab Dispos 40:1321–1327. https://doi.org/10.1124/dmd.111.043752
Zhang H, Gao N, Tian X, Liu T, Fang Y, Zhou J, Wen Q, Xu B, Qi B, Gao J, Li H, Jia L, Qiao H (2016) Content and activity of human liver microsomal protein and prediction of individual hepatic clearance in vivo. Nat Sci Rep 5:17671. https://doi.org/10.1038/srep17671
Hesse LM, Venkatakrishnan K, Court MH, Von Moltke LL, Duan SX, Shader RI, Greenblatt DJ (2000) CYP2B6 mediates the in vitro hydroxylation of bupropion: potential drug interactions with other antidepressants. Drug Metab Dispos 28:1176–1183
Faucette SR, Hawke RL, LeCluyse EL, Shord SS, Yan BF, Laethem RM, Lindley CM (2000) Validation of bupropion hydroxylation as a selective marker of human cytochrome p4502b6 catalytic activity. Drug Metab Dispos 28:1222–1230
Coles R, Kharasch ED (2008) Stereoselective metabolism of bupropion by cytochrome p4502b6 (cyp2b6) and human liver microsomes. Pharm Res 25:1405–1411. https://doi.org/10.1007/s11095-008-9535-1
Pearce RE, McIntyre CJ, Madan A, Sanzgiri U, Draper J, Bullock PL, Cook DC, Burton L, Latham J, Nevins C, Parkinson A (1996) Effects of freezing, thawing, and storing human liver microsomes on cytochrome p450 activity. Arch Biochem Biophys 331:145–169. https://doi.org/10.1006/abbi.1996.0294
Liu L, Pang KS (2006) An integrated approach to model hepatic drug clearance. Eur J Pharm Sci 29:215–230. https://doi.org/10.1016/j.ejps.2006.05.007
Naritomi Y, Nakamori F, Furukawa T, Tabata K (2015) Prediction of hepatic and intestinal glucuronidation using in vitro–in vivo extrapolation. Drug Metab Pharmacokinet 30:21–29. https://doi.org/10.1016/j.dmpk.2014.10.001
Zanger UM, Klein K (2013) Pharmacogenetics of cytochrome p450 2b6 (cyp2b6): advances on polymorphisms, mechanisms, and clinical relevance. Front Genet 4:1–12. https://doi.org/10.3389/fgene.2013.00024
Hara M, Masui K, Eleveld DJ, Struys MMRF, Uchida O (2017) Predictive performance of eleven pharmacokinetic models for propofol infusion in children for long-duration anaesthesia. Br J Anaesth 118:415–423. https://doi.org/10.1093/bja/aex007
Poulin P, Theil FP (2000) A priori prediction of tissue: plasma partition coefficients of drugs to facilitate the use of physiologically-based pharmacokinetic models in drug discovery. J Pharm Sci 89:16–35. https://doi.org/10.1002/(SICI)1520-6017(200001)89:1%3c16:AID-JPS3%3e3.0.CO;2-E
Rodgers T, Rowland M (2007) Mechanistic approaches to volume of distribution predictions: understanding the processes. Pharm Res 24:918–933. https://doi.org/10.1007/s11095-006-9210-3
Sadiq MW, Nielsen EI, Khachman D, Conil JM, Georges B, Houin G, Laffont CM, Karlsson MO, Friberg LE (2016) A whole-body physiologically based pharmacokinetic (wb-pbpk) model of ciprofloxacin: a step towards predicting bacterial killing at sites of infection. J Pharmacokinet Pharmacodyn 44:69–79. https://doi.org/10.1007/s10928-016-9486-9
Peeters MYM, Allegaert K, Blussé van Oud-Alblas HJ, Cella M, Tibboel D, Danhof M, Knibbe CA (2010) Prediction of propofol clearance in children from an allometric model developed in rats, children and adults versus a 0.75 fixed-exponent allometric model. Clin Pharmacokinet 49:269–275. https://doi.org/10.2165/11319350-000000000-00000
Allegaert K, de Hoon J, Verbesselt R, Naulaers G, Murat I (2007) Maturational pharmacokinetics of single intravenous bolus of propofol. Paediatr Anaesth 17:1028–1034. https://doi.org/10.1111/j.1460-9592.2007.02285.x
Raoof AA, van Obbergh LJ, Verbeeck RK (1995) Propofol pharmacokinetics in children with biliary atresia. Br J Anaesth 74:46–49. https://doi.org/10.1093/bja/74.1.46
Saint-Maurice C, Cockshott ID, Douglas EJ, Ricjard MO, Harmey JL (1989) Pharamacokinetics of propofol in young children after a single dose. BJA Br J Anaesth 63:667–670. https://doi.org/10.1093/bja/63.6.667
Murat I, Billard V, Vernois J, Zaouter M, Marsol P, Souron R, Farinotti R (1996) Pharmacokinetics of propofol after a single dose in children aged 1-3 years with minor burns: comparison of three data analysis approaches. Anesthesiology 84:526–532
Valtonen M, Iisalo E, Kanto J, Rosenberg P (1989) Propofol as an induction agent in children: pain on injection and pharmacokinetics. Acta Anaesthesiol Scand 33:152–155
Jones RD, Chan K, Andrew LJ (1990) Pharmacokinetics of propofol in children. Br J Anaesth 65:661–667
Kataria BK, Ved SA, Nicodemus HF, Hoy GR, Lea D, Dubois MY, Mandema JW, Shafer SL (1994) The pharmacokinetics of propofol in children using three different data analysis approaches. Anesthesiology 80:104–122
Shangguan WN, Lian Q, Aarons L, Matthews I, Wang Z, Chen X, Freemantle N, Smith FG (2006) Pharmacokinetics of a single bolus of propofol in chinese children of different ages. Anesthesiology 104:27–32
Rigby-Jones AE, Nolan JA, Priston MJ, Wright PM, Sneyd JR, Wolf AR (2002) Pharmacokinetics of propofol infusions in critically ill neonates, infants, and children in an intensive care unit. Anesthesiology 97:1393–1400. https://doi.org/10.1097/01.sa.0000101092.14429.db
Acknowledgements
Funding was provided by Agentschap voor Innovatie door Wetenschap en Technologie (Grant No. IWT/SBO 130033).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Michelet, R., Van Bocxlaer, J., Allegaert, K. et al. The use of PBPK modeling across the pediatric age range using propofol as a case. J Pharmacokinet Pharmacodyn 45, 765–785 (2018). https://doi.org/10.1007/s10928-018-9607-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-018-9607-8