Abstract
Worldwide, lack of access to safe drinking water together with inadequate sanitation and hygiene is an overwhelming contributor to approximately 4 billion cases of illness annually. This study was set out to understand the effects of hygiene and sanitation interventions on targeted health outcomes including diarrhoeal prevalence in children’s of Turkana District, Kenya. The interventions undertaken included capacity building and empowerment approach to trigger communities to demand hygiene and sanitation facilities. Three hundred mothers were randomly sampled in a baseline survey carried out in 2007 and in a post-intervention survey carried out in 2008 (a repeat cross-sectional study design). Specimens were collected for microbiological tests of key diarrhoea related pathogens. Overall, Faecal coliform counts per 100 ml sample had significant variations between 2007 and 2008; in Kakuma, reduced from 88 to 30.2 colony units (P = 0.005), Lodwar Central where the number reduced from 91 to 17.3 units (P = 0.003), and in Lokichogio Division, the number reduced from 63.8 to 23.6 units (P = 0.006). From the 230 stool samples examined, the proportion of children from whom infectious pathogens of Proteus spp. was isolated reduced from 16 to 7 % while Escherichia coli reduced from 54 to 41 %. Overall, prevalence of diarrhoea related microbes in children aged <5 years reduced from 91.3 % in 2007 to 78.3 % after intervention (2008). It is notable that sanitation and hygiene promotion leads to significant reduction of diarrhoea prevalence in children aged <5 years. Its application should therefore be up-scaled in resource constrained areas.
Similar content being viewed by others
Introduction
Turkana District is classified as arid and semi-land (ASAL). It has varied climate of dry and semi arid, with less than one-third of the land mass being arable. Turkana is the largest District in Kenya, covering an area of 77,000 square kilometres and population of about 855,399 people [1]. The topographical features, includes mountain ranges to the west, open plains in the middle, and several seasonal rivers and Lake Turkana to the East. Inadequate water supply and access are major problems; people walk long distances to collect water from rivers and streams, which are likely to be contaminated. Water scarcity is likely to affect sanitation and hygiene practices and especially hand washing practices.
Problem Statement
Diarrhoeal diseases are responsible for childhood mortality and morbidity, primarily in developing Countries. Despite advances in case management of diarrhoeal diseases, it still remains a major cause of morbidity and mortality among young children in developing countries [2]. In developing countries, diarrhoea accounts for the deaths of nearly 1.6 million children aged <5 years annually—or almost 15 % of all deaths for this sector of the population [3].
Justification
Inadequate disposal of human excreta and other waste can lead to transmission and spread of diseases that originate from excreta. Out of all the sanitation and hygiene related diseases, diarrhoea disease is the most deadly especially for children [4]. However, a significant reduction on deaths from diarrhoeal diseases has been observed in the last decades due to public based interventions [5].
Methods
Study Area/Location
The study was conducted in Lokichoggio, Kakuma and Central Divisions of Turkana District. These three Divisions were purposively selected due to ongoing Ministry of Health and UNICEF sanitation and hygiene programme.
Study Population
The study participants were mothers living in the Divisions who had children aged <5 years.
Sample Size Determination
The formula used by Lemeshow et al. (1990) in WHO health related studies for sample size determination was used.
where;
n = Population sample.
P 1 = Prevalence of diarrhoea, where from previous studies it is estimated at 25 %
P 2 = Post intervention prevalence of core baseline practices estimated at 12.5 %, assuming that the intervention will reduce prevalence of diarrhoea by 50 %. This gave a sample size of approximately 140. Considering a maximum design effect of 2, this gave a sample size of (140 × 2) = 280. This was approximated to 300.
Data Collection
Household survey was carried out before and after interventions based on a structured household questionnaire and observation checklist. The key indicators used as proxy health indicators included faecal coliform count in drinking water, microbes in stool specimen and survey on prevalence of diarrhoea. Water samples were taken at the point of use in the households for further examination in the laboratory for chlorine level and presence or absence of faecal coliforms. The levels of chlorine were detected using DPD complex tablets. Chlorine level of <0.2 mg/l was regarded as low and in-effective while chlorine levels of more than 0.2 mg/l was regarded as effective in protecting the water from bacterial contamination. Bacterial contamination was detected by presence or absence of faecal coliforms using Filter Membrane Technique.
Literature Review
Diarrhoea continues to be one of the leading causes of death and loss of disability adjusted life years in the developing world [6]. Estimates from the past four decades indicate that, although there has been a decrease in mortality rates, diarrheal disease-related morbidity has remained high [7]. Interventions to reduce diarrhea incidence generally focus on water supply, water quality, sanitation and hygiene for all age groups, as well as breastfeeding, adequate nutrition and immunizations specifically for children aged <5 years.
According to Black and Fawcett [8], more than 1.2 billion people worldwide gained access to improved sanitation between 1990 and 2004. However, even with this progress, some 41 % of the world’s population (an estimated 2.6 billion people), including 980 million children lack access to proper sanitation. Lack of adequate sanitation, poor hygiene and safe portable water are serious global health problems and contribute to deaths of 1.5 million children under the age of 5 years annually due to diarrhoeal diseases.
Although infant and child mortality rates have reduced significantly in most nations in the recent decades, 1.5–2 million children still die every year from water and sanitation related diseases (Murray 2000). According to WHO, an estimated 2.2 million children aged <5 years die from diarrhoeal diseases each year [9]. More children are debilitated by illness, pain and discomfort primarily from diarrhoeal diseases, intestinal worms, from various eye and skin diseases and diseases related to insufficient and unsafe water [10]. WHO notes further that 4 billion cases of diarrhoea occur annually; of which 88 % are attribute to unsafe water and inadequate sanitation and hygiene. The report adds that diarrhoeal diseases also account for 1.8 million deaths every year, with the majority being children aged <5 years (WHO 2007). WHO data on the burden of disease shows that, “approximately 3.1 % of deaths (1.7 million) and 3.7 % of disability adjusted life-years (DALYs) or equivalence of 54.2 million sufferings worldwide is attributed to unsafe water and sanitation and hygiene”. In Africa and other developing Countries in South East Asia, 4–8 % of all disease burdens are attributable to these factors.
In Kenya, WHO estimated that in 2002 only 52 % of Kenyans don’t have access to improved sanitation. According to Central Bureau of Statistics, most common form of sanitation facility being pit latrine at 64 % of the population, while more than 16 % have no facility and defecates in the brush, field or in the open. Apart from those that do not use a latrine, 49 % shared their toilet with other households [11].
Diarrheal diseases are frequently transmitted by faecally-contaminated water. Consequently, Most of the burden of diarrhoeal disease is preventable with improvement in sanitation, water quality, and hygiene. Improved water supply reduces diarrhea morbidity by 21 % while improved sanitation reduces diarrhea morbidity by 37.5 % (WHO 2004). However in rural areas of low income countries, it is often prohibitively expensive to provide residents with networked sanitation and water treatment that provide microbiologically and chemically safe water and consistently separate faeces from the environment (Ezzati et al. 2003). This therefore requires targeted hygiene and sanitation interventions at the point of use.
Results
The results in this section detail the observed changes in the quality of drinking water at the point of use and microbes in stool of children aged below 5 years.
Chlorine Level and Faecal Coliform Count Before and After Intervention
Residual chlorine test was only carried out in households that claimed to be treating their water or consuming treated water as an indicator and measure of reduced risk to ill health. Chlorine level of <0.2 mg/l as cut off was regarded low and in-effective against harmful microbes; levels of chlorine of more than 0.2 mg/l in water were regarded effective in protection against bacterial contamination. Overall, there was marginal change in proportion of households whose drinking water had residual chlorine of more than 0.2 mg/l; in Kakuma, the proportion of households whose drinking water had residual chlorine of more than 0.2 mg/l increased from 12.9 % in 2007 to 22.6 in 2008. Similar marginal changes were noted for Lodwar Central and Lokichogio Divisions as shown in the table shown in Table 1.
The proportion of households which had water with chlorine levels above 0.2 mg/l marginally increased though the changes recorded were not statistically significant. These observations are consistent with field expectations since there were no direct interventions targeting increased chlorine use. This was by design so as to avoid possible confounding effects arising from the known effects of chlorine in reducing diarrhoea related diseases as compared to changing mothers’ behaviour.
Regarding observed changes in faecal coliform counts per 100 ml sample, there were significant variations between 2007 and 2008. The reduction in mean faecal coliform counts was significant in all Divisions; in Kakuma, mean faecal coliforms per 100 ml sample reduced from 88 to 30.2 colony units (P = 0.005), similar results were recorded in Lodwar Central where the number reduced from 91 to 17.3 units (P = 0.003), while in Lokichogio Division, the number reduced from 63.8 to 23.6 units (P = 0.006). This is as shown in the Table 2.
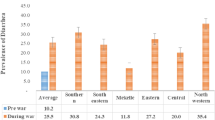
Diarrhea Prevalence in Children Aged <5 years (Before and After Intervention)
Overall prevalence of diarrhea in children reduced from 43.7 % in 2007 to 30.7 % in 2008. There was consistent reduction in diarrhea among children as reported by mothers and by level of education of mothers. Children of mothers with no education reported about 10 % reduction in diarrhea (42.9 % in 2007–33.3 % in 2008), those of mothers with primary education reducing from 37.2 % in 2007 to 31.8 % in 2008, while those of mothers with post-primary education reducing from 57.6 % in 2007 to 24.2 % in 2008. This is as detailed in Table 3.
As depicted above, the noted reduction in prevalence of diarrhea increased with education. The observed changes where only statistically significant for the children of mothers with post-primary education (χ² = 4.85, P = 0.028).
Diarrhoea Related Microbes in Children Stool Before and After Intervention
A total of 230 stool specimens from children aged <5 years were examined at baseline and 1 year thereafter (end-line). Overall, prevalence of diarrhea related microbes in children aged <5 years reduced from 91.3 % in 2007 to 78.3 % after intervention (2008); this is as depicted in the Figs. 1 and 2.
From the 230 stool samples examined, the proportion of children from whom infectious pathogens of Proteus spp. was isolated reduced from 16 to 7 % while E. coli reduced from 54 to 41 %. Specimen outside from children aged more than 5 years where excluded, they increased from 8 to 27 %. The detailed distribution of the microbes is as shown in the Table 4.
Subsequently, it is notable from the test statistic that there was no significant effective change in diarrhoea related microbes in children stool (χ2 = 47.32, P = 0.5).
Prevalence of Bacterial and Parasitic Organisms in Children Aged <5 Years
From the 285 and 291 stool samples examined at baseline and after intervention studies respectively, potential infectious pathogen was isolated from 21.5 % of the children at baseline and 10 % of the children after intervention. Bacterial pathogens were isolated from 6.0 % the children at the baseline study and 3.4 % of the children after intervention while parasitic pathogens were isolated from 15.5 % of the children at baseline and 6.6 % of the children after intervention.
The pathogens isolated were; Salmonella species in 5.3 % of the children at baseline study and 1 % of the children after intervention. Giardia lamblia Trophozoite was isolated in 3.5 % of the children at baseline study and in 0.4 % child after intervention. Ascaris Lumbricoides was isolated in 3.5 of the children at baseline and in 2.1 % of the children after intervention. Trichuris Trichiura was isolated in 0.4 % children at baseline and none of the children after intervention. E. histolytica trophozoite was isolated in 8.1 % of the children at baseline study and in 4.1 % of the children after intervention. This is as detailed in Table 5.
Drugs Susceptibility Testing
This was carried out on the commonly prescribed drugs in order to control for possible confounding effects of drug resistance. All isolates were highly sensitive to Gentamicin and ceftriaxone 23 (96 %) but highly resistant to Amoxycillin-clavulanic acid (Augmentin) (50 %). The order of increasing resistance was ceftriaxone, cefotaxim, ceftazidim, norfloxacine, ciprofloxacin, Amikacin, Naladixic acid, sxt, Gentamicin, Augmentin. Resistance to norfloxacine, ciprofloxacine and ceftazidime was <8 % with ceftriaxone and cefotaxim showing least resistance at 16.9 %. This is as detailed in Fig. 3.
Discussion
The function of hygienic behaviour is to prevent transmission of the agents of infection to human. In the developing world today, diarrhoeal diseases are amongst the biggest killers of children and it has been shown that the simple act of washing hands with soap can cut diarrhoea risk by almost half. A study on hand washing in Korea noted that out of the 942 student participants, there was a 30.3 % increase in hand washing practice compared to 1 year prior to the study (Jae-Hyun Park et al. 2010).
Like in this study, a similar study undertaken to determine whether a large 3-year hygiene promotion programme in Bobo-Dioulasso, Burkina Faso was effective in changing behaviours associated with the spread of diarrhoeal diseases, some notable gains included safe disposal of children’s stools, that increased from 80 % at pre-intervention (1995) to 84 % post (1998). There was reduced prevalence of diarrhoea and improved general health status of children aged <5 years.
Promotion of hygienic behaviours especially hand washing has been identified as a public health intervention likely to have considerable impact in the reduction of diarrhoeal diseases in young children in developing Countries (McLennan 2000). While washing hands at critical times is accepted as an effective intervention against diarrhoeal disease, evidence is also now growing for its effectiveness against respiratory infections (Cairncross 2003). Based on the results of the Turkana study, up-scaling of hand washing with soap practice, is highly recommended especially using the germ theory to promote healthy behaviours and reduce diarrhoea infection in children.
Conclusion and Recommendations
The Turkana study interventional approach involved Participatory Hygiene and Sanitation Transformation (PHAST) that integrated the principles of Community Led Total Sanitation (CLTS). CLTS basically trigger communities into demanding hygiene and sanitation facilities. The observed health gains are likely associated with community involvement through the participatory approaches. The key challenge in implementation of effective sanitation and hygiene interventions is up-scaling in the local communities and domesticating the tools to suit the local conditions. In this study there was overall significant improvement in community health outcomes before and after the intervention with comparative reduction in faecal coliform count in drinking water ranging from 40.2 to 73.7 %. Similarly, diarrhoea related microbes in children stool reduced by 13 %. These significant achievements attest to the importance of such participatory approaches in resource constrained areas. Their wider application in such communities is hence highly recommended.
References
Central Bureau of Statistics. (2002). Ministry of finance and planning in Nairobi, Kenya. Kenya 1999 population and housing census, the popular report.
Murray, C. J., Lopez, A. D., & Jammison, D. T. (1994). The global burden of diseases in 1990: Summary of results, sensitivity analysis and future directions. Bulletin of the World Health Organization, 72(3), 495–509.
World Health Organization. (2003). Shaping the future. Geneva: World Health Organization.
Pruss, A., Kay, D. K., Fewtrell, F., & Bartram, J. (2002). Estimating the burden of disease from water, sanitation and hygiene. Journal of Environmental health perspectives, 110, 537–542.
Ahmed, F., Clemens, J. D., Rao, M. R., & Banik, A. K. (1994). Family latrines and pediatric shigellosis in rural Bangladesh: benefit or risk? International Journal of Epidemiology, 23(4), 856–862.
Lopez, A. D., Mathers, C. D., Ezzati, M., Jamison, D. T., & Murray, C. J. (2006). Global and regional burden of disease and risk factors, systematic analysis of population health data. Lancet, 367, 1747–1757.
Kosek, M., Bern, C., & Guerrant, R. L. (2003). The global burden of diarrhoeal disease, as estimated from studies published between 1992 and 2000. Bulletin of World Health Organisation, 81, 197–204.
Murray, C. J., Lopez, A. D., Mathers, C. D., & Stein, C. (2001). The Global Burden of Disease 2000 Project: Aims methods and data sources, global programme on evidence for health policy. Discussion paper No. 36 World Health Organisation. Geneva.
World Health Organization Water. (2004). Sanitation and hygiene links to health: Facts and figures. http://www.who.int/water_sanitation_health/publications/factsfigures04/en/. Accessed on Nov 12, 2011.
UNICEF. (2007). Progress for children: a world fit for children statistical review, MDG 4: Reduce child mortality, NewYork 6:18–24.
Central Bureau of Statistics (CBS) [Kenya], Ministry of Health (MOH) [Kenya], and ORC Macro. (2004). Kenya Demographic and Health Survey 2003. Calverton, Maryland: CBS, MOH, and ORC Macro.
Acknowledgments
We thank Unicef, Kenya Country Office who accepted this nested repeat cross-sectional study to be undertaken in their project.
Confilct of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kariuki, J.G., Magambo, K.J., Njeruh, M.F. et al. Effects of Hygiene and Sanitation Interventions on Reducing Diarrhoea Prevalence Among Children in Resource Constrained Communities: Case Study of Turkana District, Kenya. J Community Health 37, 1178–1184 (2012). https://doi.org/10.1007/s10900-012-9560-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10900-012-9560-1