Abstract
Children with electrical status epilepticus in sleep (ESES) often present with cognitive deficits and behavioral difficulties. Children that present with autism spectrum disorder (ASD), attention deficit hyperactivity disorder (ADHD), intellectual disability, and ESES would be expected to manifest more complex symptoms and increased behavioral difficulties given the nature of these disorders. Despite the complex presentation, there is little research to support effective treatments that manage behavior challenges and associated symptoms of ASD in such patients. In the present case report, the authors implemented a validated parent management training intervention, The Research Unit on Behavioral Interventions (RUBI) Autism Network Parent Training program (RUBI-PT) via telemedicine to manage symptoms of ADHD, ASD, and disruptive behaviors in an 8-year-old South-Asian boy with ESES and associated mild intellectual disability. The family participated in 15 RUBI-PT sessions over 22 weeks. Parent report and ratings using the clinical global impression, improvement scale (CGI-I) indicated reductions in challenging behavior and improvement in adaptive skills. The current case report demonstrates the utility of RUBI-PT in the treatment of behavioral difficulties in a patient with ASD, ADHD, and ESES. Further, the present study explores future directions for the use of RUBI-PT to address behavioral challenges associated with ESES and commonly co-occurring conditions and highlights the importance of cultural responsive practice in the context of parent management training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Electrical status epilepticus in sleep (ESES) is a form of childhood-onset epileptic encephalopathy, characterized by epilepsy (with or without clinical seizures), cognitive regression, and marked activation of epileptiform activity during non-rapid eye movement (NREM) sleep to produce an electroencephalography (EEG) pattern of near-continuous spike-wave discharges (Loddenkemper et al., 2011; Samanta & Khalili, 2022). ESES is a rare condition, occurring in 0.02–0.05% of children with epilepsy that affects children between 2 and 12 years old, with a peak onset of 4–5 years old (Galanopoulou et al., 2000).
The terms “ESES” and “CSWS” (Continuous Spike-Wave During Slow-Wave Sleep) are often used interchangeably, as “CSWS” is the most common epileptic syndrome that is often associated with ESES (Kotagal, 2017). Many researchers and clinicians characterize ESES as the specific EEG pattern and CSWS as the broader clinical syndrome that also includes developmental, cognitive, and behavioral regression (MacAllister et al., 2017). CSWS results in global developmental and cognitive regression in the domains of language, behavior, learning, attention, memory, motor skills, social interaction, and global intelligence (Arican et al., 2021; Liu & Wong, 2000). ESES has also been associated with high rates of behavioral difficulties in children. For instance, Raha et al., (2012) found that 11 of 12 children with ESES displayed challenging behaviors including hyperactivity, aggressiveness, and poor social interaction. Moreover, 50% met the criteria for ADHD, which is consistent with other research on ESES/CSWS (Ng & Hodges, 2020; Raha et al., 2012).
The behavioral symptoms of ESES-related syndromes may often appear similar to those of autism spectrum disorder (ASD) (e.g., language regression in Landau-Kleffner Syndrome or global developmental regression in CSWS). However, the disorders are distinct. Within ESES, there must be an ESES pattern on EEG, and in ASD, an individual must display specific difficulties related to social communication and interaction, as well as restrictive interests and repetitive behaviors (APA, 2013; Panda & Panda, 2019). Notably, the high rates of co-occurrence of epilepsy and ASD have been established by research, as epilepsy and seizure disorders occur in around 10–20% of individuals with ASD (Liu et al., 2022; Lukmanji et al, 2019; Zarakoviti et al., 2022). Attention-deficit/hyperactivity disorder (ADHD) is another common co-occurring condition in children with ASD as ADHD is found in 20–50% of children with ASD (Sillanpää et al., 2016; Williams et al., 2016). Not surprisingly, rates of ADHD and epilepsy are higher in children with ASD. In a longitudinal study of 3237 individuals with ASD, it was found that individuals with ASD who were diagnosed with childhood-onset epilepsy were twice as likely to develop ADHD compared to those without epilepsy (Carson et al., 2022). Further, children with ASD, epilepsy, and ADHD may also present with cognitive challenges or intellectual disability given rates of epilepsy are significantly higher in individuals with ASD and intellectual disability compared to those without (Carson et al., 2022; Zarakoviti et al., 2022).
Children with ESES, ASD, intellectual disability, and ADHD are likely to display higher rates of challenging behaviors due to the nature of symptoms of all four disorders. Such behaviors may include difficulty sustaining attention, adaptive skill deficits, restrictive interests and repetitive behaviors, challenges with transitioning to non-preferred activities, social communication differences, irritability, and challenges with impulse control (APA, 2016; Dominick et al., 2007; Ng & Hodges, 2020). However, research on treatment for the behavioral difficulties associated with ESES and co-occurring disorders is limited (Besag, 2018). Further, as it stands, there is no research examining the utility of behavioral treatment for children presenting with ESES with co-occurring ASD, intellectual disability, and ADHD.
Parent management training (PMT) is an evidence-based treatment approach to managing behaviors that create challenges for children and their families. Although PMT has not yet been studied in patients who present with ESES and co-occurring neurobehavioral disorders (i.e., ASD and ADHD), a variety of PMT programs exist (e.g., Brief Behavioral Intervention, Kazdin’s PMT, Parent–Child Interaction Therapy, Incredible Years). These programs are effective in reducing disruptive behaviors for children with epilepsy (Treble-Barna et al., 2013; Fein et al., 2019), ADHD (Axelrad et al., 2013), and ASD (Webster-Stratton et al., 2018). However, such programs do not specifically address ASD symptoms, such as deficits in non-verbal communication, restrictive repetitive behaviors, and adaptive skills deficits, which may exacerbate behaviors and create additional challenges for children and their families. Past studies assert that function-based treatments that target replacing problem behaviors and teaching new skills are the most effective in increasing independence and reducing problem behaviors (Bearss et al., 2015).
To date, only one PMT program has been developed with this in mind and specifically for children with ASD. The Research Unit on Behavioral Interventions (RUBI) Autism Network developed the structured Parent Training program (RUBI-PT), which is a function-based treatment program derived from an applied behavioral analysis framework. RUBI-PT is designed to reduce behavioral problems and increase adaptive skills in preschoolers (Bearss et al., 2018a). In randomized trials, RUBI-PT was found to be superior to parent education in reducing disruptive behavior and noncompliance, being acceptable to caregivers, and increasing adaptive skills in children aged 3–7 with ASD and co-occurring disruptive behavior (Bearss et al., 2015; Scahill et al., 2016). Moreover, RUBI-PT has shown promise with older children (age 8) and delivery via telemedicine (Bearss et al., 2018b; Shanok et al., 2021).
In this case report, the authors implemented RUBI-PT via telemedicine to treat symptoms of ASD and ADHD in an 8-year-old male patient with ESES and mild intellectual disability. The objectives of this case study were to (1) demonstrate the utility of using RUBI-PT to treat a child with the complex presentation of ESES and co-occurring mild intellectual disability, ASD, and ADHD and (2) add to the literature on the use of telehealth to deliver culturally responsive treatment using RUBI-PT.
Patient Presentation
The patient, “CJ,” was referred for a neuropsychological assessment by his pediatric neurologist given his medical history of generalized epilepsy complicated by Electrical Status Epilepticus during Slow-Wave Sleep (ESES). The primary referral question was to determine if there was evidence of change in his developmental trajectory given concern for the syndrome of Continuous Spike and Wave during Slow-Wave Sleep (CSWS). At the time of the evaluation, he was described by his family as being a bilingual Asian American male with unbalanced language proficiency in Telugu and English. Specifically, English was the first language he learned, his strongest language, and the language in which all academic instruction was provided. He was described as understanding much of what is spoken to him in Telugu, but not speaking and not receiving academic instruction in Telugu. As such, he was presumed to not have acquired Cognitive and Academic Language Proficiency Skills in Telugu.
With regard to developmental history, CJ was born full term with normal birthweight and without serious pre-, peri-, or post-natal complications. He attained early developmental milestones within expectations but evidenced regression in speech and language development by the age of 2 years. Specifically, he spoke in short phrases by the age of 2 years but gradually stopped speaking by age 4 years. He received speech-language therapy (SLT), which resulted in improved speech and language functioning. Medically, his first seizure occurred at the age of 4 years, which was a generalized tonic–clonic (GTC) seizure in nature. Comprehensive epilepsy genetic panel identified a mutation in the PACS1 gene, which has been described in the literature as being associated with intellectual disability, epilepsy, ASD, and ADHD (Lusk et al., 2020). His seizures were well controlled with Onfi, but interictal electroencephalograms (EEGs) worsened over time and he inevitably met criteria for ESES by the age of 5 years (spike-wave index, SWI, of > 86%).
CJ was hospitalized at the age of 6 years due to septic shock, associated mycoplasma pneumonia, and acute respiratory failure. During this time, EEG documented multiple subclinical seizures. He was later transferred to an inpatient rehabilitation unit to aid in recovery of functional skills. It was during this time that he was diagnosed with ASD and ADHD (Combined Presentation) by the treating pediatric neuropsychologist. Observed and/or reported behaviors considered in the diagnosis of ADHD included difficulties with inattention (e.g., makes careless mistakes, challenges following directions, and distractibility) and hyperactivity and impulsivity (e.g., interrupting others, often leaving his seat in class). Symptoms of ASD included deficits in social communication (e.g., poor social-emotional reciprocity, including difficulty with back-and-forth conversation; deficits in non-verbal communicative behaviors, including atypical range and use of facial expressions, as well as poor modulation and use of eye contact; and deficits in developing and maintaining relationships, including lack of friends, no approach of or interest in other children, difficulties sharing imaginative play, not recognizing or responding to others’ emotions, and not starting conversations to be friendly) and restricted, repetitive interests and behaviors (e.g., stereotyped and repetitive speech, including idiosyncratic use of language, pronoun confusion, and echolalia; repetitive use of objects; and highly restricted and intense interest in cars). During his inpatient evaluation, CJ was also diagnosed with major neurocognitive disorder given reported regression in functioning thought to be due to his medical condition.
CJ was 7 years, 11 months old at the time of his most recent follow-up neuropsychological evaluation, and his epilepsy was being treated with a combination of Onfi, Keppra, and Zonisamide. In terms of psychosocial context, CJ’s mother earned a high school diploma and worked in the home to care for the family. His father earned a college degree and was employed in software development. Cognitive concerns reported by his parents included problems with memory (e.g., forgetfulness, need for prompts, and reminders), comprehension, and expressive language, with worsening functioning since the onset of his seizures. With respect to social-emotional functioning, he was described by his family as being happy overall. His family reported new-onset fearfulness, however, including being afraid of monsters, school work, and reading. Behaviorally, his parents endorsed a long-standing history of behavioral challenges including noncompliance, verbal defiance, spitting, yelling, and worsening social functioning. CJ was in the 2nd grade at the time of the evaluation. He participated in virtual instruction in response to the COVID-19 pandemic and received special education services for reading, writing, and academics.
Tests used as part of the neuropsychological assessment conducted with CJ are listed in Table 1. Testing modifications were not needed with the exception of COVID-19-related safety precautions. Notable observations during the assessment included irritability and distress when performing some tests, rigidity, preference for routines, unresponsiveness to social praise, atypical prosody, non-fluent speech, repetitive and stereotyped behaviors and speech, sensory interests, and clear problems with attention, focus, and concentration. Observations also suggested variable effort and engagement with testing procedures. For example, he often put forth strong effort, but he sometimes refused to perform tests or discontinued them early when they were non-preferred. Note that scores from tests that were clearly invalid are not reported or interpreted. Nevertheless, findings were thought to be a slight underestimate of the CJ’s abilities, but provided an accurate reflection of his day-to-day functioning in similar environments within the context of his neurobehavioral and medical history. Considering all information available, the CJ’s clinical presentation was consistent with diagnoses of mild intellectual disability (which was given provisionally pending his response to behavioral interventions, potential improvements with reductions in anti-seizure medications, and results of re-assessment), ASD, and ADHD. See Table 1 for a complete summary of inpatient and outpatient neuropsychological results.
Treatment Procedures
Following participation in a separate parent management training program when CJ was 6 years old, (Brief Behavioral Intervention), his family continued to endorse behavioral challenges including noncompliance, spitting, screaming, and were subsequently referred to begin parent management training using the Research Unit on Behavioral Interventions (RUBI) Autism Network developed structured Parent Training program (RUBI-PT). CJ and his mother attended 15, 1 h family therapy sessions. RUBI-PT was created for use with preschool-aged children with ASD and co-occurring disruptive behaviors such as noncompliance, tantrums, aggression, interrupting others, difficulty following instructions, and difficulties with transitions. RUBI-PT is designed to be delivered in weekly sessions up to 16 weeks by a master’s or doctoral-level clinician who is familiar with behavior principles and has experience working with children with ASD.
RUBI-PT consists of 11 core sessions and up to two supplemental sessions, 1 home visit, and up to six parent–child coaching sessions (Bearss et al., 2018a). The core sessions are outlined in Table 2. RUBI-PT is designed to be flexible, such that while the listed order in Table 2 is the recommended order for treatment sessions, sessions can be implemented flexibly (introduced earlier or later) as indicated by clinical judgment and family need. During treatment, one to two supplemental sessions are offered that are unique to the needs of the family and address common difficulties for young children with ASD such as toileting, time-out, sleep problems, and feeding problems. Additionally, parent–child coaching sessions were offered throughout treatment as needed by the family. While this is not a requirement of RUBI-PT, these sessions allow for the clinician to coach the caregiver and child through additional practice of strategies learned in session (e.g., time-out, planned ignoring). During the last core session, caregivers are provided with a Behavior Support Plan that is specific to each patient. The Behavior Support Pan outlines the strategies that caregivers have learned throughout treatment and steps on when and how to use them. Caregivers are provided with a completed copy of the Behavior Support Plan at the end of treatment. RUBI-PT also includes opportunities for home visits and telephone booster sessions, although these are not offered within this current setting. However, follow-up appointments are available for patients as needed.
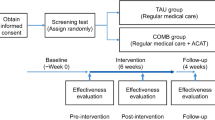
After an intake appointment was conducted by a licensed clinical psychologist (RF) to determine the appropriateness of RUBI-PT for the family, CJ and his mother participated in 15 total sessions over 22 weeks. Several sessions had to be rescheduled due to patient illness and scheduling conflicts. Sessions were conducted in English via telemedicine, in response to the COVID-19 pandemic, within a children’s hospital/academic medical setting. Sessions were led by an advanced graduate student (EJ) who provided co-therapy with a licensed clinical psychologist (RF) trained in providing RUBI-PT.
Because the sessions were provided using telemedicine, a few modifications were made to the treatment protocol. As opposed to being held in clinic, sessions were delivered using a secure, HIPPA-compliant telemedicine platform. Supplemental materials used during sessions (e.g., parent handouts and video vignettes) were shared with the CJ and his mother via screen sharing features on the computer, naturalistic observations of the parent–child interaction as well as parent–child coaching were delivered via the telemedicine platform, and the parent handouts were also sent to the family electronically.
Course of Treatment
CJ’s mother attended 15 sessions, four of which CJ was present with his mother to allow for in vivo modeling and coaching of strategies. Each RUBI-PT session began with a review of the previous week’s homework and prior strategies outlined in the Behavior Support Plan. The clinicians encouraged the family to share successes and challenges from the past week’s strategies, and problem solved as needed to support the CJ’s mother’s use of previously learned skills. Following review of previous strategies and homework, the next strategy was introduced. To facilitate learning of the strategies during the session, video vignettes and parent handouts with practice activities and outlines of the steps were shared with the CJ’s mother. At the end of the session, CJ’s parent was assigned homework to practice implementing the newly introduced strategy. For the sessions where CJ was present, he was given choices of activities to engage in at home while his mother attended to the telemedicine visit (e.g., playing with cars, building with blocks, playing on his tablet).
CJ was present for the first three sessions of RUBI-PT, during which he was observed to engage in several behaviors that created challenges for himself and his family. He engaged in noncompliance when given instructions by EJ and his parents, exhibited physical aggression toward his sister (hitting), and frequently interrupted the visit by climbing on his mother or grabbing the laptop his parents were using for the telemedicine visit. CJ was then present for the 10th session, where he did not display any instances of physical aggression and gave his mother appropriate space. He did, however, engage in mild noncompliance, but quickly modified his behavior in response to his mother’s use of prevention and compliance training strategies.
During the sessions in which CJ was present, the clinicians modeled strategies to shape behavior (e.g., providing him with high-frequency specific praise and ignoring attention-seeking behaviors). The clinicians also highlighted opportunities for parent coaching and for CJ’s mother to practice previously introduced strategies in session (e.g., prompting her to offer labeled praise to the CJ, using transitional warnings with him, and briefly removing attention when CJ engaged in attention-seeking behaviors). Given CJ’s unique challenges in adaptive functioning as a result of his diagnoses of ASD, intellectual disability, and ESES, treatment sessions also focused on increasing adaptive skills. Many challenging behaviors that occurred were due to CJ’s lack of adaptive skills ability and behavioral challenges (e.g., following directions to brush his teeth and bathing independently). To address these challenges, strategies were combined to help CJ’s mother prevent noncompliance, give directions more effectively and use a task analysis to teach CJ the steps needed to complete tasks he did not know how to do.
The clinicians actively provided culturally responsive assessment and treatment by asking the CJ’s mother about family dynamics, values, stressors, religion, and cultural practices during the intake assessment. Further, at the beginning of every treatment session, the clinician (EJ) would ask the family about their weekend and assess any upcoming holidays, special events, or routine changes that are important to the family. From these discussions, CJ’s mother shared specific South-Asian cultural practices, family preferences, and family values that were actively assessed, discussed, and incorporated into treatment.
While going through the family’s daily routine, the CJ’s mother emphasized the importance of dedicated prayer time for herself and CJ’s father. During which, she reported that he frequently interrupts her. Consequently, the clinicians worked with her to develop preventative strategies such as offering CJ choices of activities he can do while his parents are praying, using a transitional warning timer to signal the change in routine, and using a token economy system to reward positive behaviors. Additionally, CJ’s mother shared that bed-sharing was an important family value, as well as a way to monitor CJ’s ESES. She noted that while there are difficulties in the CJ’s bedtime routine, that he particularly enjoys getting the bed ready for his family. Through discussions with her, this practice was incorporated into the treatment and the clinicians encouraged the CJ’s mother to use “first then” statements during parts of the bedtime routine that may be more challenging (e.g., “first brush your teeth then you can help set up the bed”).
Given that CJ’s mother had previously endorsed prayer as a value, as sessions continued, she was encouraged to share updates about upcoming religious and spiritual events that may impact their family’s schedule. CJ’s mother shared that during specific holidays family and friends frequently came over. She also shared plans for family from out of the country to visit. She expressed concerns about CJ spitting on others during these engagements and that family members’ and friends’ reactions to CJ’s behavior often resulted in escalating his behavior. Therefore, the clinicians spent time discussing how to respond to concerns from guests and opportunities to use preventative strategies when guests are over (e.g., removing the television remote from the area), ensuring that those directly with CJ enforce consistent consequences for spitting (e.g., by removing stickers from his sticker chart), and highlighting opportunities to use and model positive attention and planned ignoring with house guests.
Progress Monitoring
As part of routine clinical care, the Clinical Global Impression- Improvement Scale (CGI-I; Guy, 1976) is administered at three times points throughout treatment. The CGI-I captures the patient’s overall degree of improvement on a 7-point scale from very much improved (score of 1) to no change (score of 4) and very much worse (score of 7). CJ’s mother was asked to complete the CGI-I after completing sessions on antecedent-based strategies (e.g., prevention strategies), consequence-based strategies, and at the one-month follow-up visit from treatment. At each time point, she was asked: “How much do you think your child’s behavior has changed since the beginning of treatment?” She was also asked to share noted instances of target behaviors that were addressed throughout treatment. Such behaviors included decreasing spitting at others, following instructions, using and “indoor” voice, bathing and brushing teeth independently. While specific frequency counts were not reported for all behaviors targeted in treatment, they were reported for instances of spitting and following instructions to teeth brush independently.
Treatment Outcomes
At each time point, the CJ’s mother was asked: “How much do you think your child’s behavior has changed since the beginning of treatment?” and instructed to use the CGI-I anchors to rate her answer. The scores from the CGI-I across the three-time points are summarized in Table 3. On the CGI-I, CJ’s mother reported that she noticed that CJ’s behavior had substantially improved since the beginning of treatment. With regard to parent report of challenging behaviors, she also reported decreases in the behaviors of following directions to brush teeth and spitting throughout treatment. The reported observations are summarized in Table 4.
Discussion
This case report demonstrates the successful application of RUBI-PT in management of disruptive behaviors in an 8-year-old male with a history of ESES, ASD, ADHD, and mild intellectual disability. In addition to the parent-reported CGI-I rating, CJ’s parent reported other treatment gains including an increase in self-regulation (e.g., CJ stopping himself before he spits and correcting himself when he uses “mean” language), compliance with instructions (e.g., following morning and bedtime routine), reduction in physical aggression (e.g., spitting and hitting), and CJ learning new skills (e.g., buttoning pants, brushing teeth by himself, and bathing himself). The family also indicated that family members visiting from abroad shared positive reactions to improvements in his behavior. The strategies emphasized in this case study may be beneficial for clinicians working with children with ASD, ADHD, and co-occurring intellectual disability and seizure disorders in the future.
In addition to demonstrating the utility of RUBI-PT within the context of a complex patient presentation not previously reported, this study adds to the existing literature in a variety of other ways. As the use of telemedicine for service delivery expands, this study is beneficial as it further highlights the effectiveness of RUBI-PT via telemedicine (Bearss et al., 2018a). This case illustrates specific modifications that can be made when delivering RUBI-PT via telemedicine. This has wide implications for service provision and access for patients in the future who may not be able to participate in treatment in-person. Additionally, this case presented an opportunity for clinicians to provide culturally responsive treatment by discussing and addressing cultural factors with the CJ’s mother to support treatment. Culturally responsive treatment was facilitated by incorporating questions about culture, language, and values into the diagnostic intake and throughout treatment sessions, as well as inviting CJ’s mother to share her familial and cultural values, traditions, and celebrations with the clinicians. These practices facilitated the implementation of culturally responsive treatment that fits within CJ and his family’s values.
This is an area of importance that may contribute to the existing literature, as recent research highlights that the use of culturally responsive intervention and treatment practices is reported as an area of need by culturally and linguistically diverse caregivers of children with ASD(de Leeuw et al., 2020; Papoudi et al., 2021). The use of culturally responsive intervention and treatment with this population may facilitate earlier intervention and assessment practices, parent participation, and involvement in assessment and intervention, and may help mitigate disparities in intervention outcomes among culturally and linguistically diverse families (Davenport et al., 2018).
While this case demonstrates promising results, there are limitations to the study. First, the data collected in this case report are subjective parent report data from the CGI-I. The use of pre and post-treatment narrowband behavioral measures may provide more clinically significant information. Moreover, due to the nature of single-case designs, the present study is limited by generalizability. Further, due to the lack of a treatment control group, the direct causality of treatment on behavior change cannot be assumed as there may be other factors (e.g., time, medication changes) that contributed to treatment outcomes. To overcome this limitation, future studies should continue to examine the use of parent-mediated interventions for children with ESES who present with disruptive behaviors. Although ESES is rare, many children with ESES display disruptive behaviors and co-occurring conditions that may contribute to behavioral difficulties; therefore, the investigation of this treatment method within this population is suggested.
RUBI-PT is unique in comparison to other parent management training programs in that it is not only effective in reducing disruptive behavior but also addressing the core symptoms of ASD and is effective in increasing adaptive skills (Bearss et al., 2015, 2018b; Scahill et al., 2016). Moreover, RUBI-PT has demonstrated feasibility in being delivered in a telemedicine format, making it accessible to a wider variety of families (Bearss et al., 2018b; Shanok et al., 2021). Despite the effectiveness of the RUBI-PT for preschool-aged children with ASD and co-occurring disruptive behavior, it has yet to be validated for use with patients with other neurological conditions that may co-occur with ASD (e.g., epilepsy, ESES, intellectual disability) as well as cross-culturally. Therefore, the current study lays the foundation for future research aimed at considering culturally responsive practices when using parent training models such as the RUBI-PT. This study also lends itself for future studies to examine the utility and validity of RUBI-PT for use in autistic children with other neurological conditions.
References
Arican, P., Gencpinar, P., Dundar, N. O., & Tekgul, H. (2021). Electrical status epilepticus during slow-wave sleep (ESES): Current perspectives. Journal of Pediatric Neurosciences, 16(2), 91.
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA
Axelrad, M. E., Butler, A. M., Dempsey, J., & Chapman, S. G. (2013). Treatment effectiveness of a brief behavioral intervention for preschool disruptive behavior. Journal of Clinical Psychology in Medical Settings, 20, 323–332. https://doi.org/10.1007/s10880-013-9359-y
Bearss, K., Burrell, T. L., Challa, S. A., Postorino, V., Gillespie, S. E., Crooks, C., & Scahill, L. (2018a). Feasibility of parent training via telehealth for children with autism spectrum disorder and disruptive behavior: A demonstration pilot. Journal of Autism and Developmental Disorders, 48(4), 1020–1030.
Bearss, K., Johnson, C. R., Handen, B. L., Butter, E., Lecavalier, L., Smith, T., & Scahill, L. (2018b). Parent training for disruptive behavior: The RUBI Autism Network, clinician manual. Oxford University Press.
Bearss, K., Johnson, C., Smith, T., Lecavalier, L., Swiezy, N., Aman, M., McAdam, D. B., Butter, E., Stillitano, C., Minshawi, N., & Sukhodolsky, D. G. (2015). Effect of parent training vs parent education on behavioral problems in children with autism spectrum disorder: A randomized clinical trial. JAMA, 313(15), 1524–1533.
Besag, F. M. (2018). Epilepsy in patients with autism: Links, risks and treatment challenges. Neuropsychiatric Disease and Treatment, 14, 1.
Carson, L., Parlatini, V., Safa, T., Baig, B., Shetty, H., Phillips-Owen, J., Prasad, V., & Downs, J. (2022). The association between early childhood onset epilepsy and attention-deficit hyperactivity disorder (ADHD) in 3237 children and adolescents with Autism Spectrum Disorder (ASD): A historical longitudinal cohort data linkage study. European Child & Adolescent Psychiatry. https://doi.org/10.1007/s00787-022-02041-3
Davenport, M., Mazurek, M., Brown, A., & McCollom, E. (2018). A systematic review of cultural considerations and adaptation of social skills interventions for individuals with autism spectrum disorder. Research in Autism Spectrum Disorders, 52, 23–33.
Dominick, K. C., Davis, N. O., Lainhart, J., Tager-Flusberg, H., & Folstein, S. (2007). Atypical behaviors in children with autism and children with a history of language impairment. Research in Developmental Disabilities, 28(2), 145–162.
Fein, R. H., Banks, G. G., Gragert, M. N., & Axelrad, M. E. (2019). Brief behavioral intervention for disruptive behavior in a child with a hypothalamic hamartoma: A case report. Journal of Clinical Psychology in Medical Settings, 26, 507–515. https://doi.org/10.1007/s10880-018-9592-5
Galanopoulou, A. S., Bojko, A., Lado, F., & Moshé, S. L. (2000). The spectrum of neuropsychiatric abnormalities associated with electrical status epilepticus in sleep. Brain and Development, 22(5), 279–295.
Guy, W. B. R. R. (1976). Clinical global impression. Assessment manual for Psychopharmacology, 217–222.
Kotagal, P. (2017). Current status of treatments for children with electrical status in slow-wave sleep (ESES/CSWS). Epilepsy Currents, 17(4), 214–216.
de Leeuw, A., Happé, F., & Hoekstra, R. A. (2020). A conceptual framework for understanding the cultural and contextual factors on autism across the globe. Autism Research, 13(7), 1029–1050. https://doi.org/10.1002/aur.2276
Liu, X., Sun, X., Sun, C., Zou, M., Chen, Y., Huang, J., Wu, L., & Chen, W. X. (2022). Prevalence of epilepsy in autism spectrum disorders: A systematic review and meta-analysis. Autism, 26(1), 33–50.
Liu, X. Y., & Wong, V. (2000). Spectrum of epileptic syndromes with electrical status epilepticus during sleep in children. Pediatric Neurology, 22(5), 371–379.
Loddenkemper, T., Fernández, I. S., & Peters, J. M. (2011). Continuous spike and waves during sleep and electrical status epilepticus in sleep. Journal of Clinical Neurophysiology, 28(2), 154–164.
Lukmanji, S., Manji, S. A., Kadhim, S., Sauro, K. M., Wirrell, E. C., Kwon, C. S., & Jetté, N. (2019). The co-occurrence of epilepsy and autism: A systematic review. Epilepsy & Behavior, 98, 238–248.
Lusk, L., Smith, S., Martin, C., Taylor, C., Chung, W. (2020). PCS1 Neurodevelopmental Disorder. In Adam MP, Mirzaa GM, Pagon RA, et al (Eds). GeneReviews® [Internet]. Seattle (WA):University of Washington, Seattle; 1993–2022. https://www.ncbi.nlm.nih.gov/books/
MacAllister, W. S., Murphy, H., & Coulehan, K. (2017). Serial neuropsychological evaluation of children with severe epilepsy. Journal of Pediatric Epilepsy, 6(1), 37–43.
Ng, R., & Hodges, E. (2020). Neurocognitive profiles of pediatric patients with ESES, generalized epilepsy, or focal epilepsy. Epilepsy Research, 167, 106351.
Panda, P. K., & Panda, K. (2019). Current consensus on clinical features, pathogenesis, diagnosis and management of autism spectrum disorder in children: A brief review. Arch of Ped Research : Redelve| RD-PED. https://doi.org/10.17511/ijpr.2019.i03.07
Papoudi, D., Jørgensen, C. R., Guldberg, K., & Meadan, H. (2021). Perceptions, experiences, and needs of parents of culturally and linguistically diverse children with autism: a scoping review. Review Journal of Autism and Developmental Disorders, 8, 195–212. https://doi.org/10.1007/s40489-020-00210-1
Raha, S., Shah, U., & Udani, V. (2012). Neurocognitive and neurobehavioral disabilities in Epilepsy with Electrical Status Epilepticus in slow sleep (ESES) and related syndromes. Epilepsy & Behavior, 25(3), 381–385.
Samanta D, Al Khalili Y. Electrical Status Epilepticus In Sleep. [Updated 2022 Feb 4]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553167/
Scahill, L., Bearss, K., Lecavalier, L., Smith, T., Swiezy, N., Aman, M. G., & Johnson, C. (2016). Effect of parent training on adaptive behavior in children with autism spectrum disorder and disruptive behavior: Results of a randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 55(7), 602–609.
Shanok, N. A., Lozott, E. B., Sotelo, M., & Bearss, K. (2021). Community-based parent-training for disruptive behaviors in children with ASD using synchronous telehealth services: A pilot study. Research in Autism Spectrum Disorders, 88, 101861.
Sillanpää, M., Besag, F., Aldenkamp, A., Caplan, R., Dunn, D. W., & Gobbi, G. (2016). Psychiatric and behavioural disorders in children with epilepsy (ILAE Task Force Report): Epidemiology of psychiatric/behavioural disorder in children with epilepsy. Epileptic Disorders, 18(s1), S2–S7.
Singhal, N. S., & Sullivan, J. E. (2014). Continuous spike-wave during slow wave sleep and related conditions. International Scholarly Research Notices. https://doi.org/10.1155/2014/619079
Tiffin, J., & Asher, E. J. (1948). The purdue pegboard: norms and studies of reliability and validity. Journal of Applied Psychology, 32, 234–247.
Treble-Barna, A., Chapman, S. G., Schwartz, D. D., & Axelrad, M. E. (2013). Brief behavioral intervention for disruptive behavior in a child following frontal and temporal resection for medically intractable epilepsy: A case report. Clinical Practice in Pediatric Psychology, 1(4), 355–360. https://doi.org/10.1037/cpp0000039
Webster-Stratton, C., Dababnah, S., & Olson, E. (2018). The Incredible Years® group-based parenting program for young children with autism spectrum disorder. Handbook of parent-implemented interventions for very young children with autism, 261–282.
Williams, A. E., Giust, J. M., Kronenberger, W. G., & Dunn, D. W. (2016). Epilepsy and attention-deficit hyperactivity disorder: Links, risks, and challenges. Neuropsychiatric Disease and Treatment, 12, 287.
Zarakoviti, E., Shafran, R., Skuse, D., McTague, A., Batura, N., Palmer, T., & Reilly, C. (2022). Factor associated with the occurrence of epilepsy in autism: a systematic review. Journal of Autism and Developmental Disorders. https://doi.org/10.1007/s10803-022-05672-2
Funding
No funding was received for conducting this study. The authors have no relevant financial or non-financial interests to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interests
Emily R. Jellinek, Thomas A. Duda, Rachel H. Fein have no conflicts of interests to disclose.
Ethical approval
Single case study is not considered human subjects research by Baylor College of Medicine therefore IRB approval was not required.
Consent to Participate
CJ’s parent provided consent to publish the case study.
Consent to Publish
The participant has consented to the submission of the case report to the journal.
Human and Animal Rights and Informed Consent
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and the Helsinki declaration and its amendments. This article does not contain any studies with animals.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jellinek, E.R., Duda, T.A. & Fein, R.H. The RUBI Parent Training for Disruptive Behavior in a Child with Electrical Status Epilepticus in Sleep (ESES): A Case Report. J Clin Psychol Med Settings 30, 770–779 (2023). https://doi.org/10.1007/s10880-023-09949-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10880-023-09949-1