Abstract
Purpose
Hemorrhage increases the effect of propofol and could contribute to false-positive transcranial motor-evoked potential (TcMEP) responses under total intravenous anesthesia (TIVA). We investigated the influence of hemorrhage and subsequent fluid resuscitation on TcMEPs under desflurane anesthesia.
Methods
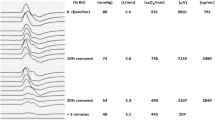
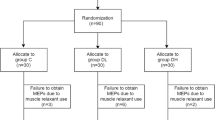
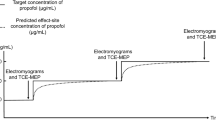
Sixteen swine (25.4 ± 0.4 kg) were anesthetized with a 4% end-tidal desflurane concentration (EtDes), which was incrementally increased to 6%, 8%, and 10% and then returned to 4% every 15 min. This procedure was repeated twice (baseline). After baseline measurements, animals were allocated to either the hemorrhage (n = 12) or control (n = 4) group. In the hemorrhage group, 600 ml of blood was removed and the EtDes protocol described above was applied. Hypovolemia was resuscitated using 600 ml of hydroxyethyl starch and the EtDes protocol was applied again. TcMEPs were measured at each EtDes. In the control group, measurements were performed without hemorrhage or fluid infusion.
Results
TcMEP responses were observed in all conditions in all limbs with 4% EtDes (0.4 MAC). TcMEP amplitudes decreased according to the EtDes to a greater degree in the lower limbs compared with the upper limbs. Hemorrhage enhanced the effect of desflurane on TcMEP amplitudes, and decreased TcMEP by 41 ± 12% in upper limbs and 63 ± 17% in lower limbs compared with baseline. Subsequent fluid resuscitation did not reverse TcMEP amplitudes.
Conclusions
TcMEP amplitudes decrease during hemorrhage under desflurane anesthesia. This phenomenon might result from an enhanced effect of desflurane on the spinal motor pathway without increasing the desflurane concentration.


Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Malhotra N, Shaffrey C. Intraoperative electrophysiological monitoring in spine surgery. Spine. 2010;35:2167–79.
Fehlings M, Brodke D, Norvell D, et al. The evidence for intraoperative neurophysiological monitoring in spine surgery: does it make a difference? Spine. 2010;35:S37-46.
Kobayashi S, Matsuyama Y, Shinomiya K, et al. A new alarm point of transcranial electrical stimulation motor evoked potentials for intraoperative spinal cord monitoring: a prospective multicenter study from the Spinal Cord Monitoring Working Group of the Japanese Society for Spine Surgery and Related Research. J Neurosurg Spine. 2014;20:102–7.
Balvin M, Song K, Slimp J. Effects of anesthetic regimens and other confounding factors affecting the interpretation of motor evoked potentials during pediatric spine surgery. Am J Electroneurodiagnostic Technol. 2010;50:219–44.
Tamkus AA, Rice KS, Kim HL. Differential rates of false-positive findings in transcranial motor evoked potential monitoring when using inhalational anesthesia versus total intravenous anesthesia during spine surgeries. Spine J. 2014;14:1440–6.
Kawaguchi M, Iida H, Tanaka S, et al. A practical guide for anesthetic management during intraoperative motor evoked potential monitoring. J Anesth. 2020;34:5–28.
Kurita T, Nakajima Y. Letter to the editor. Is the total propofol dose associated with false-positive motor evoked potentials? J Neurosurg Spine. 2019;26:1–2.
Kurita T, Kazama T, Morita K, et al. Influence of fluid infusion associated with high-volume blood loss on plasma propofol concentrations. Anesthesiology. 2004;100:871–8.
Kurita T, Uraoka M, Morita K, et al. Influence of haemorrhage on the pseudo-steady-state remifentanil concentration in a swine model: a comparison with propofol and the effect of haemorrhagic shock stage. Br J Anaesth. 2011;107:719–25.
Kurita T, Takata K, Morita K, et al. The influence of hemorrhagic shock on the electroencephalographic and immobilizing effects of propofol in a swine model. Anesth Analg. 2009;109:398–404.
Kurita T, Uraoka M, Jiang Q, et al. Influence of cardiac output on the pseudo-steady state remifentanil and propofol concentrations in swine. Acta Anaesthesiol Scand. 2013;57:754–60.
Johnson KB, Egan TD, Kern SE, et al. The influence of hemorrhagic shock on propofol: a pharmacokinetic and pharmacodynamic analysis. Anesthesiology. 2003;99:409–20.
Lyon R, Lieberman J, Grabovac M, et al. Strategies for managing decreased motor evoked potential signals while distracting the spine during correction of scoliosis. J Neurosurg Anesthesiol. 2004;16:167–70.
Lieberman J, Feiner J, Lyon R, et al. Effect of hemorrhage and hypotension on transcranial motor-evoked potentials in swine. Anesthesiology. 2013;119:1109–19.
Martin DP, Bhalla T, Thung A, et al. A preliminary study of volatile agents or total intravenous anesthesia for neurophysiological monitoring during posterior spinal fusion in adolescents with idiopathic scoliosis. Spine. 2014;39:E1318-1324.
Sloan TB, Toleikis JR, Toleikis SC, et al. Intraoperative neurophysiological monitoring during spine surgery with total intravenous anesthesia or balanced anesthesia with 3% desflurane. J Clin Monit Comput. 2015;29:77–85.
Holderfer RN, Anderson C, Furman M, et al. A comparison of the effects of desflurane versus propofol on transcranial motor-evoked potentials in pediatric patients. Childs Nerv Syst. 2014;30:2103–8.
Malcharek MJ, Loeffler S, Schiefer D, et al. Transcranial motor evoked potentials during anesthesia with desflurane versus propofol-a prospective randomized trial. Clin Neurophysiol. 2015;126:1825–32.
Kurita T, Morita K, Fukuda K, et al. Influence of hemorrhagic shock and subsequent fluid resuscitation on the electroencephalographic effect of isoflurane in a swine model. Anesthesiology. 2005;103:1189–94.
Kurita T, Takata K, Uraoka M, et al. The influence of hemorrhagic shock on the minimum alveolar anesthetic concentration of isoflurane in a swine model. Anesth Analg. 2007;105:1639–43.
Rampil IJ, King BS. Volatile anesthetics depress spinal motor neurons. Anesthesiology. 1996;85:129–34.
Zhou HH, Jin TT, Qin B, et al. Suppression of spinal cord monitoring excitability correlates with surgical immobility during isoflurane anesthesia. Anesthesiology. 1998;88:955–61.
Zhou HH, Zhu C. Comparison of isoflurane effects on motor evoked potential and F wave. Anesthesiology. 2000;93:32–8.
Eger EI 2nd, Johnson BH, Weiskopf RB, et al. Minimum alveolar concentration of I-653 and isoflurane in pigs: definition of a supramaximal stimulus. Anesth Analg. 1988;67:1174–6.
Johnson KB, Egan TD, Kern SE, et al. Influence of hemorrhagic shock followed by crystalloid resuscitation on propofol: a pharmacokinetic and pharmacodynamic analysis. Anesthesiology. 2004;101:647–59.
Lieberman JA, Feiner J, Rollins M, et al. Changes in transcranial motor evoked potentials during hemorrhage are associated with increased serum propofol concentrations. J Clin Monit Comput. 2018;32:541–8.
Parikh P, Cheongsiatmoy J, Shilian P, et al. Differences in the transcranial motor evoked potentials between proximal and distal lower extremity muscles. J Clin Neurophysiol. 2018;35:155–8.
Scheufler KM, Zentner J. Total intravenous anesthesia for intraoperative monitoring of the motor pathways: an integral view combining clinical and experimental data. J Neurosurg. 2002;96:571–9.
Kurita T, Kawashima S, Morita K, et al. Assessment of cerebral and renal autoregulation using near-infrared spectroscopy under normal, hypovolaemic and postfluid resuscitation conditions in a swine model: An observational study. Eur J Anaesthesiol. 2019;36:531–40.
Kurita T, Kawashima S, Morita K, et al. Spinal cord autoregulation using near-infrared spectroscopy under normal, hypovolemic, and post-fluid resuscitation conditions in a swine model: a comparison with cerebral autoregulation. J Intensive Care. 2020;8:27.
Chong CT, Manninen P, Sivanaser V, et al. Direct comparison of the effect of desflurane and sevoflurane on intraoperative motor-evoked potentials monitoring. J Neurosurg Anesthesiol. 2014;26:306–12.
Acknowledgements
We thank Emily Woodhouse, PhD, from Edanz Group (https://en-author-services.edanzgroup.com/ac) for editing a draft of this manuscript.
Funding
Support was received solely from institutional and/or departmental sources.
Author information
Authors and Affiliations
Contributions
TK contributed to the study design, data collection, analysis of data, and manuscript preparation. SK contributed to the study design and data collection. MMSIK contributed to the data collection and analysis of data. YN contributed to the study design. The first and revised drafts of the manuscript were written by TK, and all authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare.
Human and Animal rights
This study was approved by the Committee of the Animal Research Division at Hamamatsu University School of Medicine (approval number 2019052).
Ethical approval
All procedures performed in studies involving animals were in accordance with the ethical standards of the institution at which the studies were conducted (The Committee of the Animal Research Division at Hamamatsu University School of Medicine, approval number 2019052). This article does not contain any studies with human participants performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kurita, T., Kawashima, S., Ibrahim Khaleelullah, M.M.S. et al. Influence of hemorrhage and subsequent fluid resuscitation on transcranial motor-evoked potentials under desflurane anesthesia in a swine model. J Clin Monit Comput 36, 239–246 (2022). https://doi.org/10.1007/s10877-020-00644-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00644-2