Abstract
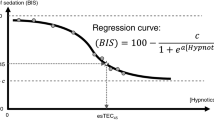
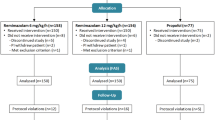
Dose-dependent effects of ketamine on processed electroencephalographic depth-of-hypnosis indices have been reported. Limited data are available for the NeuroSENSE WAVCNS index. Our aim was to establish the feasibility of closed-loop propofol-remifentanil anesthesia guided by the WAVCNS index in the presence of an analgesic dose of ketamine. Thirty ASA I-II adults, 18–54 years, requiring general anesthesia for anterior cruciate ligament surgery were randomized to receive: full-dose [ketamine, 0.5 mg kg−1 initial bolus, 10 mcg kg−1 min−1 infusion] (recommended dose for postoperative pain management); half-dose [ketamine, 0.25 mg kg−1 bolus, 5 mcg kg−1 min−1 infusion]; or control [no ketamine]. After the ketamine bolus, patients received 1.0 mcg kg−1 remifentanil over 30 s, then 1.5 mg kg−1 propofol over 30 s, followed by manually-adjusted propofol-remifentanil anesthesia. The WAVCNS was > 60 for 7/9 patients in the full-dose group at 7 min after starting the propofol infusion. This was inconsistent with clinical observations of depth-of-hypnosis and significantly higher than control (median difference [MD] 17.0, 95% confidence interval [CI] 11.4–26.8). WAVCNS was median [interquartile range] 49.3 [42.2–62.6] in the half-dose group, and not different to control (MD 5.1, 95% CI − 4.9 to 17.9). During maintenance of anesthesia, the WAVCNS was higher in the full-dose group compared to control (MD 14.7, 95% CI 10.2–19.2) and in the half-dose group compared to control (MD 11.4, 95% CI 4.7–20.4). The full-dose of ketamine recommended for postoperative pain management had a significant effect on the WAVCNS. This effect should be considered when using the WAVCNS to guide propofol-remifentanil dosing.
Trial Registration ClinicalTrails.gov No. NCT02908945.




Similar content being viewed by others
References
Punjasawadwong Y, Phongchiewboon A, Bunchungmongkol N. Bispectral index for improving anaesthetic delivery and postoperative recovery. Cochrane Database Syst Rev. 2014;6:CD003843.
Purdon PL, Sampson A, Pavone KJ, Brown EN. Clinical electroencephalography for anesthesiologists: Part I: background and basic signatures. Anesthesiology. 2015;123:937–60.
Elia N, Tramèr MR. Ketamine and postoperative pain – a quantitative systematic review of randomised trials. Pain. 2005;113:61–70.
Himmelseher S, Durieux ME. Ketamine for perioperative pain management. Anesthesiology. 2005;102:211–20.
De Kock M, Lavand’homme P, Waterloos H. “Balanced analgesia” in the perioperative period: Is there a place for ketamine? Pain. 2001;92:373–80.
Remérand F, Le Tendre C, Baud A, Couvret C, Pourrat X, Favard L, et al. The early and delayed analgesic effects of ketamine after total hip arthroplasty: a prospective, randomized, controlled, double-blind study. Anesth Analg. 2009;109:1963–71.
Loftus RW, Yeager MP, Clark JA, Brown JR, Abdu WA, Sengupta DK, et al. Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology. 2010;113:639–46.
Laskowski K, Stirling A, McKay WP, Lim HJ. A systematic review of intravenous ketamine for postoperative analgesia. Can J Anaesth. 2011;58:911–23.
Jouguelet-Lacoste J, La Colla L, Schilling D, Chelly JE. The use of intravenous infusion or single dose of low-dose ketamine for postoperative analgesia: a review of the current literature. Pain Med. 2015;16:383–403.
Zikov T, Bibian S, Dumont GA, Huzmezan M, Ries CR. Quantifying cortical activity during general anesthesia using wavelet analysis. IEEE Trans Biomed Eng. 2006;53:617–32.
West N, van Heusden K, Görges M, Brodie S, Rollinson A, Petersen CL, et al. Design and evaluation of a closed-loop anesthesia system with robust control and safety system. Anesth Analg. 2018;127:883–94.
West N, Dumont GA, van Heusden K, Petersen CL, Khosravi S, Soltesz K, et al. Robust closed-loop control of induction and maintenance of propofol anesthesia in children. Paediatr Anaesth. 2013;23:712–9.
Lee U, Ku S, Noh G, Baek S, Choi B, Mashour G. a. Disruption of frontal-parietal communication by ketamine, propofol, and sevoflurane. Anesthesiology. 2013;118:1264–75.
John ER, Prichep LS. The anesthetic cascade: a theory of how anesthesia suppresses consciousness. Anesthesiology. 2005;102:447–71.
Hayashi K, Tsuda N, Sawa T, Hagihira S. Ketamine increases the frequency of electroencephalographic bicoherence peak on the α spindle area induced with propofol. Br J Anaesth. 2007;99(3):389–95.
Maksimow A, Särkelä M, Långsjö JW, Salmi E, Kaisti KK, Yli-Hankala A, et al. Increase in high frequency EEG activity explains the poor performance of EEG spectral entropy monitor during S-ketamine anesthesia. Clin Neurophysiol. 2006;117:1660–8.
Vereecke HEM, Vanluchene AL, Mortier EP, Everaert K, Struys MMRF. The effects of ketamine and rocuronium on the A-Line auditory evoked potential index, Bispectral Index, and spectral entropy monitor during steady state propofol and remifentanil anesthesia. Anesthesiology. 2006;105:1122–34.
Hirota K, Kubota T, Ishihara H, Matsuki A. The effects of nitrous oxide and ketamine on the bispectral index and 95% spectral edge frequency during propofol-fentanyl anaesthesia. Eur J Anaesthesiol. 1999;16:779–83.
Wu CC, Mok MS, Lin CS, Han SR. EEG-bispectral index changes with ketamine versus thiamylal induction of anesthesia. Acta Anaesthesiol Sin. 2001;39:11–5.
Phillips W, Anderson A, Rosengreen M, Johnson J, Halpin J. Propofol versus propofol/ketamine for brief painful procedures in the emergency department: clinical and bispectral index scale comparison. J Pain Palliat Care Pharmacother. 2010;24:349–55.
Sakai T, Singh H, Mi WD, Kudo T, Matsuki A. The effect of ketamine on clinical endpoints of hypnosis and EEG variables during propofol infusion. Acta Anaesthesiol Scand. 1999;43:212–6.
Faraoni D, Salengros JC, Engelman E, Ickx B, Barvais L. Ketamine has no effect on bispectral index during stable propofol-remifentanil anaesthesia. Br J Anaesth. 2009;102:336–9.
Vereecke HEM, Agrawal G, Bibian S, Struys MMRF. The effect of ketamine and rocuronium on the neurosense WAVcns index during steady-state anesthesia with propofol and remifentanil. San Francisco: The International Society for Anaesthetic Pharmacology; 2013.
Chou R, Gordon DB, de Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of postoperative pain: a clinical practice guideline from the American Pain Society, the American Society of Regional Anesthesia and Pain Medicine, and the American Society of Anesthesiologists’ Committee on Regional Anesthesia, Executive Committee, and Administrative Council. J Pain Elsevier. 2016;17:131–57.
Bibian S, Zikov T. NeuroSENSE Monitor with WAVcns Cortical Quantifier: A Deterministic Approach to EEG Analysis (white paper) [Internet]. 2018. http://www.neurowavesystems.com/pdfs/NeuroSENSE_White_Paper_September_2018.pdf.
Görges M, West N, Cooke E, Pi S, Brant RF, Dumont GA, et al. Evaluating NeuroSENSE for assessing depth of hypnosis during desflurane anesthesia: a randomized trial. Can J Anesth. 2019. https://doi.org/10.1007/s12630-019-01522-5.
Sahni N, Panda NB, Jain K, Batra YK, Dhillon MS, Jagannath P. Comparison of different routes of administration of clonidine for analgesia following anterior cruciate ligament repair. J Anaesthesiol Clin Pharmacol. 2015;31:491–5.
Schnider TW, Minto CF, Gambus PL, Andresen C, Goodale DB, Shafer SL, et al. The influence of method of administration and covariates on the pharmacokinetics of propofol in adult volunteers. Anesthesiology. 1998;88:1170–82.
Babadi B, Brown EN. A review of multitaper spectral analysis. IEEE Trans Biomed Eng. 2014;61:1555–64.
Bojak I, Day HC, Liley DTJ. Ketamine, propofol, and the EEG: a neural field analysis of HCN1-mediated interactions. Front Comput Neurosci. 2013;7:1–14.
Acknowledgements
The authors would like to thank the anesthesiologists, surgeons, operating room staff, post-anesthetic care unit nurses, and surgical day care nurses at the Eagle Ridge Hospital for their interest and willingness to support study procedures, and the patients for their participation in the study.
Funding
This study was supported by internal funds. NeuroWave Systems Inc. provided loan equipment and sensors for this study.
Author information
Authors and Affiliations
Contributions
KvH contributed to study design and data analysis. EC contributed to study design, patient recruitment, data collection, and data analysis. SB contributed to study design and data analysis. NW contributed to data analysis. MG contributed to study design and data analysis. GAD contributed to study design. JMA contributed to study design. RNM contributed to study design and data collection. All authors contribution to manuscript preparation.
Corresponding author
Ethics declarations
Conflict of interest
GAD is a co-inventor of the NeuroSENSE monitor (NeuroWave Systems Inc., Cleveland, OH), GAD and JMA have consulted for NeuroWave Systems Inc. KvH, MG, GAD, JMA, and RNM are party to a licensing agreement between UBC and NeuroWave Systems Inc. for control technology. GAD, JMA, and RNM have received funds for research sponsored by NeuroWave Systems Inc. The remaining authors have no interests to declare.
Informed consent
Written informed consent was obtained from all individual participants in this study.
Research involving Human Participants
This study was conducted with research ethics board approval (Fraser Health Research Ethics Board, FHREB 2016-054).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
van Heusden, K., Cooke, E., Brodie, S. et al. Effect of ketamine on the NeuroSENSE WAVCNS during propofol anesthesia; a randomized feasibility trial. J Clin Monit Comput 35, 557–567 (2021). https://doi.org/10.1007/s10877-020-00511-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-020-00511-0