Abstract
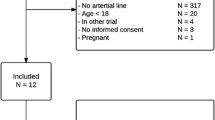
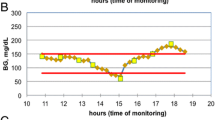
Blood glucose and its variability of is a major prognostic factor associated with morbidity. We hypothesized that intravenous microdialysis incorporated in a central venous catheter (CVC) would be interchangeable with changes in blood glucose measured by the reference method using a blood gas analyzer. Microdialysis and central venous blood glucose measurements were simultaneously recorded in high-risk cardiac surgical patients. The correlation between absolute values was determined by linear regression and the Bland–Altman test for repeated measurements was used to compare bias, precision, and limits of agreement. Changes in blood glucose measurement were evaluated by four-quadrant plot and trend interchangeability methods (TIM). In the 23 patients analyzed, the CVC was used as part of standard care with no complications. The correlation coefficient for absolute values (N = 99) was R = 0.91 (P < 0.001). The bias, precision and limits of agreement were − 9.1, 17.4 and − 43.2 to 24.9 mg/dL, respectively. The concordance rate for changes in blood glucose measurements (N = 77) was 85% with the four-quadrant plot. The TIM showed that 14 (18%) changes of blood glucose measurements were uninterpretable. Among the remaining 63 (82%) interpretable changes, 23 (37%) were interchangeable, 13 (20%) were in the gray zone, and 27 (43%) were not interchangeable. Microdialysis using a CVC appears to provide imprecise absolute blood glucose values with risk of insulin misuse. Moreover, only one third of changes in blood glucose measurements were interchangeable with the reference method using the TIM.





Similar content being viewed by others
References
NICE-SUGAR Study Investigators, Finfer S, Chittock DR, Su SY-S, et al. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–97.
van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in critically ill patients. N Engl J Med. 2001;345:1359–67.
Critchell CD, Savarese V, Callahan A, Aboud C, Jabbour S, Marik P. Accuracy of bedside capillary blood glucose measurements in critically ill patients. Intensive Care Med. 2007;33:2079–84.
Yatabe T, Yamazaki R, Kitagawa H, et al. The evaluation of the ability of closed-loop glycemic control device to maintain the blood glucose concentration in intensive care unit patients. Crit Care Med. 2011;39:575–8.
Leelarathna L, English SW, Thabit H, et al. Feasibility of fully automated closed-loop glucose control using continuous subcutaneous glucose measurements in critical illness: a randomized controlled trial. Crit Care 2013;17:R159.
Wollersheim T, Engelhardt LJ, Pachulla J, et al. Accuracy, reliability, feasibility and nurse acceptance of a subcutaneous continuous glucose management system in critically ill patients: a prospective clinical trial. Ann Intensive Care 2016;6:70.
van Hooijdonk RTM, Leopold JH, Winters T, et al. Point accuracy and reliability of an interstitial continuous glucose-monitoring device in critically ill patients: a prospective study. Crit Care 2015;19:34.
Boom DT, Sechterberger MK, Rijkenberg S, et al. Insulin treatment guided by subcutaneous continuous glucose monitoring compared to frequent point-of-care measurement in critically ill patients: a randomized controlled trial. Crit Care 2014;18:453.
Smith JL, Rice MJ. Why have so many intravascular glucose monitoring devices failed? J Diabetes Sci Technol. 2015;9:782–91.
Schierenbeck F, Owall A, Franco-Cereceda A, Liska J. Evaluation of continuous blood glucose monitoring system using a central venous catheter with an integrated microdialysis function. Diabetes Technol Ther. 2013;15:26–31.
Schierenbeck F, Franco-Cereceda A, Liska J. Evaluation of continuous blood glucose monitoring system using central venous microdialysis. J Diabetes Sci Technol. 2012;6:1365–71.
Blixt C, Rooyackers O, Isaksson B, Wererman J. Continuous on-line glucose measurement by microdialysis in a central vein. A pilot study. Crit Care 2013;17:R87.
Schierenbeck F, Franco-Cereceda A, Liska J. Accuracy of 2 different continuous glucose monitoring systems in patients undergoing cardiac surgery: intravascular microdialysis versus subcutaneous tissue monitoring. J Diabetes Sci Technol. 2017;11:108–16.
Leopold JH, van Hooijdonk RTM, Boshuizen M, et al. Point and trend accuracy of continuous intravenous microdialysis-based glucose-monitoring device in critically ill patients: a prospective study. Ann Intensive Care 2016;6:68.
Klonoff DC, Lias C, Vigersky R, et al. The surveillance error grid. J Diabetes Sci Technol. 2014;8:658–72.
Fischer MO, Diouf M, de Wilde RBP, Dupont H, Hanouz JL, Lorne E. Evaluation of cardiac output by 5 arterial pulse contour techniques using trend interchangeability method. Medicine (Baltim) 2016;95:e3530.
von Elm E, Altman DG, Egger M, et al. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147:573–7.
Kottner J, Audigé L, Brorson S, et al. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64:96–106.
Roques F, Nashef SA, Michel P, et al. Risk factors and outcome in European cardiac surgery: analysis of the EuroSCORE multinational database of 19030 patients. Eur J Cardiothorac Surg. 1999;15:816–22–23.
Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–82.
Perrino AC, Harris SN, Luther M. Intraoperative determination of cardiac output using multiplane transoesophageal echocardiography. A comparison to thermodilution. Anesthesiology 1998;89:350–7.
Ouattara A, Lecomte P, Le Manach Y, et al. Poor intraoperative blood glucose control is associated with a worsened hospital outcome after cardiac surgery in diabetic patients. Anesthesiology 2005;103:687–94.
Thiele RH, Hucklenbruch C, Ma JZ, et al. Admission hyperglycemia is associated with poor outcome after emergent coronary bypass grafting surgery. J Crit Care 2015;30:1210–6.
SFAR, SRLF. Formal recommendations by the experts. Glycemic control in intensive care unit and during anaesthesia. Ann Fr Anesth Reanim. 2009;28:410–5.
Wentholt IM, Hoekstra JB, Devries JH. A critical appraisal of the continuous glucose-error grid analysis. Diabetes Care 2006;29:1805–11.
Krinsley JS, Chase JG, Gunst J, et al. Continuous glucose monitoring in the ICU: clinical considerations and consensus. Crit Care 2017;21:197.
Bansal B, Carvalho P, Mehta Y, et al. Prognostic significance of glycemic variability after cardiac surgery. J Diabetes Complicat. 2016;30:613–7.
Skjaervold NK, Aadahl P. Comparison of arterial and mixed venous blood glucose levels in hemodynamically unstable pigs: implications for location of a continuous glucose sensor. Acta Diabetol. 2012;49:489–91.
Acknowledgements
The authors would like to thank Maquet Critical Care AB (Solna, Sweden) and especially Emmanuel Cheyron for providing all devices and monitoring equipment. The manufacturer provided no input to the design or conduct of the study or in the decision to submit the manuscript for publication.
Funding
This study was a standard care study and was not funded by any institution. All furniture (monitoring device and single-use material) was provided free of charge by Maquet Critical Care AB. The authors performed the present work in the course of their normal duties as full-time employees of public-sector healthcare institutions.
Author information
Authors and Affiliations
Contributions
Conception and design: MOF, JLF, SF, JLH, JLG; Data collection: CG, MOF; Data analysis: MOF, VS; Drafting the manuscript: CG, MOF, JLF and Revision of the manuscript after critical review: all authors.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Fischer, MO., Gouëzel, C., Fradin, S. et al. Assessment of changes in blood glucose concentration with intravascular microdialysis. J Clin Monit Comput 32, 1135–1142 (2018). https://doi.org/10.1007/s10877-018-0111-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-018-0111-x