Abstract
Objectives
The ankle-brachial index (ABI) is known to be indicative of sub-clinical peripheral arterial diseases that are correlated with cardiovascular disease risk factors like atherosclerosis or ischemic extremity. Due to its occluding measurement nature, this may not be appealing to less cooperative patients when multiple prolonged screening is required. A simple and non-intrusive approach termed pulse transit time ratio (PTTR) has recently shown to be potential surrogate marker for the prolonged ABI measurement. Other studies have also suggested that subjects with hypertension have stiffer arterial wall and thereby can confound transit time related parameters. Thus, it becomes important to understand the PTTR normality and difference of hypertensive children when␣compared to those measured from normotensive children.
Methods
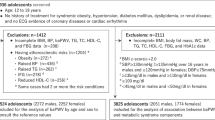
About 55 normotensive (39 male; aged 8.4 ± 2.3 yr) and 4 hypertensive (4 male; aged 5–10 yr) Caucasian children were recruited from the same geographical location. A customized device was used to compute pulse transit time related measurements. Since the PTTR approach produced a delta value that was similar to that of ABI, possible inter-subject physiologic differences had limited confounding effects on the derived PTTR parameter.
Results
The obtained transit time measurements from the hypertensive children had lower pulse transit time value when compared to their normotensive counterparts. However, the statistical analysis indicated that they had insignificant PTTR difference (p > 0.01) from those seen in the normotensive children.
Conclusions
The findings herein suggest that stiffer arterial wall may have confounding effects on the derived transit time related measurements but it is limited on the PTTR parameter. Similar to the ABI approach, PTTR may be only confounded by abnormal local changes in either of the measured peripheral arterial wall. Hence, the PTTR technique shows promise to be an ABI marker from this perspective.
Similar content being viewed by others
References
Selvin E, Erlinger TP. Prevalence of and risk factors for peripheral arterial disease in the United States: results from the National Health and Nutrition Examination Survey, 1999–2000. Circulation 2004; 110: 738–743
Carbayo JA, Divison JA, Escribano J. Using ankle-brachial index to detect peripheral arterial disease: prevalence and associated risk factors in a random population sample. Nutr Metab Cardiovasc Dis 2007; 17: 41–49
Valentine RJ, Guerra R, Stephan P, Scoggins E, Clagett GP, Cohen J. Family history is a major determinant of subclinical peripheral arterial disease in young adults. J Vasc Surg 2004; 39: 351–356
Foo JYA, Lim CS, Wilson SJ, Williams GR, Harris M-A, Cooper DM. Pulse transit time ratio as a potential marker for paediatric crural and brachial blood pressure index. J Hum Hypertens 2007; 21:415–417.
Pollak MH, Obrist PA. Aortic-radial pulse transit time and ECG Q-wave to radial pulse wave interval as indices of beat-by-beat blood pressure change. Psychophysiology 1983; 20: 21–28
Li B, Gao H, Li X, Liu Y, Wang M. Correlation between brachial-ankle pulse wave velocity and arterial compliance and cardiovascular risk factors in elderly patients with arteriosclerosis. Hypertens Res 2006; 29: 309–314
Protogerou AD, Blacher J, Mavrikakis M, Lekakis J, Safar ME. Increased pulse pressure amplification in treated hypertensive subjects with metabolic syndrome. Am J Hypertens 2007; 20: 127–133
O’Sullivan JJ, Derrick G, Griggs P, Foxall R, Aitkin M, Wren C. Ambulatory blood pressure in schoolchildren. Arch Dis Child 1999; 80: 529–532
Foo JYA, Wilson SJ. Normalized peripheral transit time to monitor hypertension in children. J Med Eng Technol (in press, doi: 10.1080/03091900500422253).
Foo JYA, Wilson SJ, Williams GR, Harris M-A, Cooper DM. Age-related factors that confound peripheral pulse timing characteristics in Caucasian children. J Hum Hypertens 2005; 19: 463–466
National high blood pressure education program working group on high blood pressure in children and adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics 2004; 114: 555–576.
Foo JY, Lim CS. Dual-channel photoplethysmography to monitor local changes in vascular stiffness. J Clin Monit Comput 2006; 20: 221–227
Netea RT, Smits P, Lenders JW, Thien T. Does it matter whether blood pressure measurements are taken with subjects sitting or supine? J Hypertens 1998; 16: 263–268
Pitson D, Chhina N, Knijn M, Herwaaden V, Stradling J. Changes in pulse transit time and pulse rate as markers of arousal from sleep in normal subjects. Clin Sci 1994; 87: 269–273
Lane JS, Vittinghoff E, Lane KT, Hiramoto JS, Messina LM. Risk factors for premature peripheral vascular disease: results for the National Health and Nutritional Survey, 1999–2002. J Vasc Surg 2006; 44: 319–324
Lehmann ED, Hopkins KD, Gosling RG. Assessment of arterial distensibility by automatic pulse wave velocity measurement Hypertension 1996; 27: 1188–1190
Nitzan M, Khanokh B, Slovik Y. The difference in pulse transit time to the toe and finger measured by photoplethysmography. Physiol Meas 2002; 23: 85–93
Geddes LA, Baker LE. Principles of applied biomedical instrumentation. 3rd Edition. New York: John Wiley & Sons Inc, 1989: 35.
Acknowledgements
The staff support from the Department of Respiratory and Sleep Medicine of the Mater Misericordiae Children’s Hospital, South Brisbane, Queensland, Australia towards this work is greatly appreciated.
Author information
Authors and Affiliations
Corresponding author
Additional information
Foo JYA. Normality of upper and lower peripheral pulse transit time of normotensive and hypertensive children.
Rights and permissions
About this article
Cite this article
Foo, J.Y.A. Normality of Upper and Lower Peripheral Pulse Transit Time of Normotensive and Hypertensive Children. J Clin Monit Comput 21, 243–248 (2007). https://doi.org/10.1007/s10877-007-9080-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10877-007-9080-1