Abstract
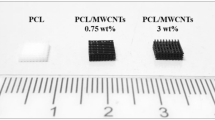
To improve the safety of dura repair in neurological surgeries, a new poly (glycolide-co-lactide)/type I collagen/chitosan artificial composite dura mater was evaluated in a rabbit model with dura mater injury. Eighteen rabbits were randomized to 3 groups: rabbits with unclosed dura mater; rabbits with dura mater repaired by fascia and rabbits with dura mater repaired by the composite membrane. Modified combine behavior score were given at a series of time points and several cytokines were also determined to reflect the inflammatory conditions. Rabbits whose dura mater was repaired by composite membrane showed a similar recovery rate of neurological function and inflammatory condition compared with the rabbits whose dura mater was repaired by fascia. In addition, the rabbits with closed dura mater were better than ones with unclosed dura mater in the restore rate of neurological function as well as inflammatory reactions according to the statistical analysis. The new artificial membrane appears to be safe and efficient in the treatment of dura mater defect.






Similar content being viewed by others
References
Ito H, Kimura T, Sameshima T, Aiyama H, Nishimura K, Ochiai C, et al. Reinforcement of pericranium as a dural substitute by fibrin sealant. Acta Neurochir (Wien). 2011;153(11):2251–4. doi:10.1007/s00701-011-1077-3.
Warren WL, Medary MB, Dureza CD, Bellotte JB, Flannagan PP, Oh MY, et al. Dural repair using acellular human dermis: experience with 200 cases: technique assessment. Neurosurgery. 2000;46(6):1391–6.
Islam S, Ogane K, Ohkuma H, Suzuki S. Usefulness of acellular dermal graft as a dural substitute in experimental model. Surg Neurol. 2004;61(3):297–302. doi:10.1016/S0090-3019(03)00380-XS009030190300380X discussion 3.
Masullo C, Pocchiari M, Macchi G, Alema G, Piazza G, Panzera MA. Transmission of Creutzfeldt–Jakob disease by dural cadaveric graft. J Neurosurg. 1989;71(6):954–5.
Thadani V, Penar PL, Partington J, Kalb R, Janssen R, Schonberger LB, et al. Creutzfeldt–Jakob disease probably acquired from a cadaveric dura mater graft. Case report. J Neurosurg. 1988;69(5):766–9. doi:10.3171/jns.1988.69.5.0766.
Kim HL, Do JY, Cho HJ, Jeon YC, Park SJ, Ma HI, et al. Dura mater graft-associated Creutzfeldt–Jakob disease: the first case in Korea. J Korean Med Sci. 2011;26(11):1515–7. doi:10.3346/jkms.2011.26.11.1515.
Xu BZ, Pan HX, Li KM, Chen XJ, Tian YD, Li YL, et al. Study and clinical application of a porcine biomembrane for the repair of dural defects. J Neurosurg. 1988;69(5):707–11. doi:10.3171/jns.1988.69.5.0707.
von der Brelie C, Soehle M, Clusmann HR. Intraoperative sealing of dura mater defects with a novel, synthetic, self adhesive patch: application experience in 25 patients. Br J Neurosurg. 2012;26(2):231–5. doi:10.3109/02688697.2011.619597.
Kim DW, Eum WS, Jang SH, Park J, Heo DH, Sheen SH, et al. A transparent artificial dura mater made of silk fibroin as an inhibitor of inflammation in craniotomized rats. J Neurosurg. 2011;114(2):485–90. doi:10.3171/2010.9.JNS091764.
Kurpinski K, Patel S. Dura mater regeneration with a novel synthetic, bilayered nanofibrous dural substitute: an experimental study. Nanomedicine (Lond). 2011;6(2):325–37. doi:10.2217/nnm.10.132.
Yamada K, Miyamoto S, Takayama M, Nagata I, Hashimoto N, Ikada Y, et al. Clinical application of a new bioabsorbable artificial dura mater. J Neurosurg. 2002;96(4):731–5. doi:10.3171/jns.2002.96.4.0731.
Li N, Zhao WG, Pu CH, Shen JK. Clinical application of artificial dura mater to avoid cerebrospinal fluid leaks after microvascular decompression surgery. Minim Invasive Neurosurg. 2005;48(6):369–72. doi:10.1055/s-2005-915629.
Luciano RM, Zavaglia CA, Duek EA, Alberto-Rincon MC. Synthesis and characterization of poly(l-lactic acid) membranes: studies in vivo and in vitro. J Mater Sci Mater Med. 2003;14(1):87–94. doi:5114036.
Mooney DJ, Mazzoni CL, Breuer C, McNamara K, Hern D, Vacanti JP, et al. Stabilized polyglycolic acid fibre-based tubes for tissue engineering. Biomaterials. 1996;17(2):115–24. doi:0142961296857565.
Kim EJ, Yoon SJ, Yeo GD, Pai CM, Kang IK. Preparation of biodegradable PLA/PLGA membranes with PGA mesh and their application for periodontal guided tissue regeneration. Biomed Mater. 2009;4(5):055001. doi:10.1088/1748-6041/4/5/055001.
Petrie C, Tholpady S, Ogle R, Botchwey E. Proliferative capacity and osteogenic potential of novel dura mater stem cells on poly-lactic-co-glycolic acid. J Biomed Mater Res A. 2008;85(1):61–71. doi:10.1002/jbm.a.31367.
Chen G, Sato T, Ohgushi H, Ushida T, Tateishi T, Tanaka J. Culturing of skin fibroblasts in a thin PLGA-collagen hybrid mesh. Biomaterials. 2005;26(15):2559–66. doi:10.1016/j.biomaterials.2004.07.034.
Kuo Y-C, Yeh C-F. Effect of surface-modified collagen on the adhesion, biocompatibility and differentiation of bone marrow stromal cells in poly(lactide-co-glycolide)/chitosan scaffolds. Colloids Surf B. 2011;82(2):624–31.
Wang XG, Li QY, Ma L, You C, YuRong Z, HuaFeng S, et al. Fabrication and characterization of poly(l-lactide-co-glycolide) knitted mesh-reinforced collagen–chitosan hybrid scaffolds for dermal tissue engineering. J Mech Behav Biomed Mater. 2012;8:204–15.
Zhang WH, Wang XW, Wang CF. Experimental research on the biocompatibility and mechanical properties of PLGA/Type-I collagen/chitosan composite membrane as artificial spinal dural mater. Acta Univ Med NanJing (Nat Sci). 2009;29:836–9.
Bai WS, Wang XW, Yuan W, Wang ZC, Liang L, Wang HX. Effects of poly (lactic-co-glycolic acid)/type-I collagen/chitosan composite membrane in rabbit models of spinal cord injury. Chin J Tissue Eng Res. 2012;16(3):471–4.
Kontogeorgakos VA, Voulgaris S, Korompilias AV, Vekris M, Polyzoidis KS, Bourantas K et al. The efficacy of erythropoietin on acute spinal cord injury. An experimental study on a rat model. Arch Orthop Trauma Surg. 2009;129(2):189–94. doi:10.1007/s00402-008-0594-x.
Hara M, Takayasu M, Watanabe K, Noda A, Takagi T, Suzuki Y, et al. Protein kinase inhibition by fasudil hydrochloride promotes neurological recovery after spinal cord injury in rats. J Neurosurg. 2000;93(1 Suppl):94–101.
Jackson N, Muthuswamy J. Artificial dural sealant that allows multiple penetrations of implantable brain probes. J Neurosci Methods. 2008;171(1):147–52. doi:10.1016/j.jneumeth.2008.02.018.
Hollister SJ. Scaffold design and manufacturing: from concept to clinic. Adv Mater. 2009;21(32–33):3330–42. doi:10.1002/adma.200802977.
Ma Z, Gao C, Gong Y, Ji J, Shen J. Immobilization of natural macromolecules on poly-l-lactic acid membrane surface in order to improve its cytocompatibility. J Biomed Mater Res. 2002;63(6):838–47. doi:10.1002/jbm.10470.
Muzzarelli R, Baldassarre V, Conti F, Ferrara P, Biagini G, Gazzanelli G, et al. Biological activity of chitosan: ultrastructural study. Biomaterials. 1988;9(3):247–52.
Shin SY, Park HN, Kim KH, Lee MH, Choi YS, Park YJ, et al. Biological evaluation of chitosan nanofiber membrane for guided bone regeneration. J Periodontol. 2005;76(10):1778–84. doi:10.1902/jop.2005.76.10.1778.
Rivlin AS, Tator CH. Effect of duration of acute spinal cord compression in a new acute cord injury model in the rat. Surg Neurol. 1978;10(1):38–43.
Fehlings MG, Tator CH. The relationships among the severity of spinal cord injury, residual neurological function, axon counts, and counts of retrogradely labeled neurons after experimental spinal cord injury. Exp Neurol. 1995;132(2):220–8.
Joshi M, Fehlings MG. Development and characterization of a novel, graded model of clip compressive spinal cord injury in the mouse: part 1. Clip design, behavioral outcomes, and histopathology. J Neurotrauma. 2002;19(2):175–90. doi:10.1089/08977150252806947.
Faulkner JR, Herrmann JE, Woo MJ, Tansey KE, Doan NB, Sofroniew MV. Reactive astrocytes protect tissue and preserve function after spinal cord injury. J Neurosci. 2004;24(9):2143–55. doi:10.1523/JNEUROSCI.3547-03.200424/9/2143.
Streit WJ, Semple-Rowland SL, Hurley SD, Miller RC, Popovich PG, Stokes BT. Cytokine mRNA profiles in contused spinal cord and axotomized facial nucleus suggest a beneficial role for inflammation and gliosis. Exp Neurol. 1998;152(1):74–87. doi:10.1006/exnr.1998.6835.
Mukaino M, Nakamura M, Okada S, Toyama Y, Liu M, Okano H. Role of IL-6 in regulation of inflammation and stem cell differentiation in CNS trauma. Nihon Rinsho Meneki Gakkai Kaishi. 2008;31(2):93–8.
Wang CX, Reece C, Wrathall JR, Shuaib A, Olschowka JA, Hao C. Expression of tumor necrosis factor alpha and its mRNA in the spinal cord following a weight-drop injury. Neuroreport. 2002;13(11):1391–3.
Plunkett JA, Yu CG, Easton JM, Bethea JR, Yezierski RP. Effects of interleukin-10 (IL-10) on pain behavior and gene expression following excitotoxic spinal cord injury in the rat. Exp Neurol. 2001;168(1):144–54. doi:10.1006/exnr.2000.7604S0014-4886(00)97604-0.
Preul MC, Bichard WD, Spetzler RF. Toward optimal tissue sealants for neurosurgery: use of a novel hydrogel sealant in a canine durotomy repair model. Neurosurgery. 2003;53(5):1189–98 discussion 98–9.
Rémi P-B, Robert G, François B. Collagen-based biomaterials for tissue engineering applications. Materials. 2010;3(3):1863–87.
Parlato C, di Nuzzo G, Luongo M, Parlato RS, Accardo M, Cuccurullo L, et al. Use of a collagen biomatrix (TissuDura) for dura repair: a long-term neuroradiological and neuropathological evaluation. Acta Neurochir (Wien). 2011;153(1):142–7. doi:10.1007/s00701-010-0718-2.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bai, W., Wang, X., Yuan, W. et al. Application of PLGA/type I collagen/chitosan artificial composite dura mater in the treatment of dural injury. J Mater Sci: Mater Med 24, 2247–2254 (2013). https://doi.org/10.1007/s10856-013-4964-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10856-013-4964-8