Abstract
Background
Posterior wall isolation (PWI) added to pulmonary vein isolation (PVI) is increasingly used in ablation for persistent atrial fibrillation (PeAF) despite limited evidence of clinical benefit. We investigated the 5-year outcomes of a PVI + PWI ablation strategy with mandatory repeat procedures in PeAF.
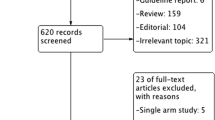
Methods
Twenty-four patients with PeAF participated in this single-arm prospective study and underwent radiofrequency ablation (RFA) with wide area circumferential ablation (WACA), roof, and inferior lines for PVI + PWI which was reinforced if required during mandated repeat procedures after 6 months. Then, patients were followed for 60 months using continuous heart rhythm monitoring by implanted cardiac monitors (ICM) and atrial fibrillation effect on quality-of-life scoring (AFEQT; range: 20–100 points) for the initial 30 months.
Results
ICM-verified cumulated AF recurrence was 54% after 30 months but the ensuing AF burden was only median 0‰ [0 to 4.8‰] overall and 1‰ [0 to 8 ‰] among patients with any recurrence. AFEQT scores increased from baseline 60 points [48 to 72] to 93 points [84 to 96] at repeat procedures P < 0.0001 and further to 96 points [93 to 99] P = 0.03 after 30 months. After 60 months, at least one episode of AF had been documented in 63% and two patients (8%) were in permanent AF.
Conclusion
Reinforced PVI + PWI was associated with low long-term AF burden and corresponding improvements in quality-of-life. Reinforced (or durable) PVI + PWI appears to be a promising strategy to treat PeAF.
Trial registration
ClinicalTrials.gov. Identifier: NCT05045131




Similar content being viewed by others
Data availability
All source data and calculations forming the basis of the conclusions in this work are available in anonymized form and will be provided by reasonable request to the corresponding author.
Abbreviations
- PeAF:
-
Persistent atrial fibrillation
- PVI :
-
Pulmonary vein isolation
- PWI:
-
Left atrial posterior wall isolation
- LA:
-
Left atrium
- WACA:
-
Wide area circumferential ablation
- ICM:
-
Implantable cardiac monitor
- AI:
-
Ablation index
- CRZ:
-
Center-right zone of the LA posterior wall
- IQR :
-
Interquartile range
References
Bai R, Di BL, Mohanty P, et al. Proven isolation of the pulmonary vein antrum with or without left atrial posterior wall isolation in patients with persistent atrial fibrillation. Heart Rhythm. 2016;13(1547–5271 (Linking)):132–140. https://doi.org/10.1016/j.hrthm.2015.08.019
Barbhaiya CR, Knotts RJ, Beccarino N, et al. Multiple procedure outcomes for nonparoxysmal atrial fibrillation: left atrial posterior wall isolation versus stepwise ablation. J Cardiovasc Electrophysiol. 2020;31(12):3117–23. https://doi.org/10.1111/jce.14771.
Jiang X, Liao J, Ling Z, et al. Adjunctive left atrial posterior wall isolation in treating atrial fibrillation. JACC: Clinical Electrophysiol. 2022;8(5):605–18. https://doi.org/10.1016/j.jacep.2022.02.001.
Worck R, Sørensen SK, Johannessen A, Ruwald M, Haugdal M, Hansen J. Posterior wall isolation in persistent atrial fibrillation feasibility, safety, durability, and efficacy. J Cardiovasc Electrophysiol. 2022;33(8):1667–74. https://doi.org/10.1111/jce.15556.
Verma A (2022) Strategies for catheter ablation of persistent atrial fibrillation: a randomized, comparative study. Clin Trials.gov; 2022. Accessed 4 Jul 2022. https://clinicaltrials.gov/ct2/show/NCT04428944
Chieng D, Sugumar H, Ling LH, et al. Catheter ablation for persistent atrial fibrillation: a multicenter randomized trial of pulmonary vein isolation (PVI) versus PVI with posterior left atrial wall isolation (PWI) - The CAPLA study. Am Heart J. 2022;243:210–20. https://doi.org/10.1016/j.ahj.2021.09.015.
Spertus J, Dorian P, Bubien R, et al. Development and validation of the atrial fibrillation effect on QualiTy-of-Life (AFEQT) Questionnaire in patients with atrial fibrillation. Circ Arrhythm Electrophysiol. 2011;4(1):15–25. https://doi.org/10.1161/CIRCEP.110.958033.
Andrade JG, Deyell MW, Verma A, Macle L, Khairy P. The cryoballoon vs irrigated radiofrequency catheter ablation (CIRCA-DOSE) study results in context. Arrhythm Electrophysiol Rev. 2020;9(1):34–9. https://doi.org/10.15420/aer.2019.13.
Sørensen SK, Johannessen A, Worck R, Hansen ML, Hansen J. Radiofrequency versus cryoballoon catheter ablation for paroxysmal atrial fibrillation: durability of pulmonary vein isolation and effect on atrial fibrillation burden: the RACE-AF randomized controlled trial. Circ Arrhythm Electrophysiol. 2021;14(5):e009573. https://doi.org/10.1161/CIRCEP.120.009573.
Sulke N, Dulai R, Freemantle N, et al. Long term outcomes of percutaneous atrial fibrillation ablation in patients with continuous monitoring. Pacing Clin Electrophysiol. 2021;44(7):1176–84. https://doi.org/10.1111/pace.14282.
Valderrábano M, Peterson LE, Swarup V, et al. Effect of catheter ablation with vein of Marshall ethanol infusion vs catheter ablation alone on persistent atrial fibrillation: the VENUS randomized clinical trial. JAMA. 2020;324(16):1620–8. https://doi.org/10.1001/jama.2020.16195.
Reddy VY, Anic A, Koruth J, et al. Pulsed field ablation in patients with persistent atrial fibrillation. J Am Coll Cardiol. 2020;76(9):1068–80. https://doi.org/10.1016/j.jacc.2020.07.007.
Gupta D, Vijgen J, Potter TD, et al. Quality of life and healthcare utilisation improvements after atrial fibrillation ablation. Heart. 2021;107(16):1296–302. https://doi.org/10.1136/heartjnl-2020-318676.
Wechselberger S, Kronborg M, Huo Y, et al. Continuous monitoring after atrial fibrillation ablation: the LINQ AF study. Europace. 2018;20(FI_3):f312–20. https://doi.org/10.1093/europace/euy038.
Diederichsen SZ, Haugan KJ, Kronborg C, et al. Comprehensive evaluation of rhythm monitoring strategies in screening for atrial fibrillation: insights from patients at risk monitored long term with an implantable loop recorder. Circulation. 2020;141(19):1510–22. https://doi.org/10.1161/CIRCULATIONAHA.119.044407.
Balabanski T, Brugada J, Arbelo E, et al. Impact of monitoring on detection of arrhythmia recurrences in the ESC-EHRA EORP atrial fibrillation ablation long-term registry. EP Europace. 2019;21(12):1802–8. https://doi.org/10.1093/europace/euz216.
Sanders P, Pürerfellner H, Pokushalov E, et al. Performance of a new atrial fibrillation detection algorithm in a miniaturized insertable cardiac monitor: results from the Reveal LINQ Usability Study. Heart Rhythm. 2016;13(7):1425–30. https://doi.org/10.1016/j.hrthm.2016.03.005.
Pothineni NVK, Amankwah N, Santangeli P, et al. Continuous rhythm monitoring-guided anticoagulation after atrial fibrillation ablation. J Cardiovasc Electrophysiol. 2021;32(2):345–53. https://doi.org/10.1111/jce.14864.
Sawhney N, Anousheh R, Chen W, Feld GK. Circumferential pulmonary vein ablation with additional linear ablation results in an increased incidence of left atrial flutter compared with segmental pulmonary vein isolation as an initial approach to ablation of paroxysmal atrial fibrillation. Circ Arrhythm Electrophysiol. 2010;3(3):243–8. https://doi.org/10.1161/CIRCEP.109.924878.
Calkins H, Hindricks G, Cappato R, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Europace. 2018;20(1):e1–160. https://doi.org/10.1093/europace/eux274.
Pambrun T, Duchateau J, Delgove A, et al. Epicardial course of the septopulmonary bundle: Anatomical considerations and clinical implications for roof line completion. Heart Rhythm. 2021;18(3):349–57. https://doi.org/10.1016/j.hrthm.2020.11.008.
Takigawa M, Derval N, Frontera A, et al. Revisiting anatomic macroreentrant tachycardia after atrial fibrillation ablation using ultrahigh-resolution mapping: Implications for ablation. Heart Rhythm. 2018;15(3):326–33. https://doi.org/10.1016/j.hrthm.2017.10.029.
Pottegård A, Schmidt SAJ, Wallach-Kildemoes H, Sørensen HT, Hallas J, Schmidt M. Data resource profile: The Danish National Prescription Registry. Int J Epidemiol. 2017;46(3):798–798f. https://doi.org/10.1093/ije/dyw213.
Funding
The study was mainly supported by the internal research fund of the department of cardiology, Gentofte Hospital. A grant from Biosense Webster Inc. covered a minor share of the required funding.
Author information
Authors and Affiliations
Contributions
All authors contributed to the manuscript, approved the final version, and agreed to be co-authors.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Danish National Science Ethics Committee (H15015153) and posted in a clinical trial database, www.clinicaltrials.gov (NCT05045131). All participants provided written informed consent.
Conflict of interests
Dr. Worck has received research grants and speaker honoraria from Biosense Webster. Dr. Sørensen has received research grants from Medtronic and Biosense Webster. Dr. Lock Hansen has received research grants from the Novo Nordisk Foundation and Dr. Hansen has received research grants and speaker honoraria from Medtronic, Biosense Webster, and Boston Scientific. Dr Johannesen, Dr. Ruwald, and Mr. Haugdal have nothing to disclose. There are no other potentially competing interests to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Worck, R., Sørensen, S.K., Johannessen, A. et al. Posterior wall isolation in persistent atrial fibrillation. Long-term outcomes of a repeat procedure strategy. J Interv Card Electrophysiol 66, 971–979 (2023). https://doi.org/10.1007/s10840-022-01402-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-022-01402-x