Abstract
Purpose
Optimal stroke prevention strategies for patients with atrial fibrillation (AF) who experience a major bleed are poorly defined. We sought to estimate the effectiveness and safety of oral anticoagulation (OAC) represcription after an OAC contraindication.
Methods
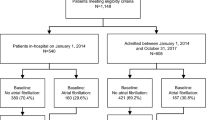
TREAT-AF is a retrospective cohort study of patients with newly diagnosed AF (2004–2012), treated in the Veterans Health Administration. From this cohort, we identified patients with a contraindication to OAC after AF diagnoses, defined as incident intracranial bleeding, non-intracranial bleeding requiring hospitalization, or unrepaired cerebral aneurysm or aortic dissection. We used multivariate Cox proportional hazards to estimate the association of OAC prescription in the 90 days following OAC contraindication to ischemic stroke and rebleeding.
Results
Among 167,190 patients with newly diagnosed AF (70 ± 11 years, 1.7% female, CHA2DS2-VASc 2.7 ± 1.7), 19,285 patients (11.5%) had an incident bleed (n = 18,342) or an unrepaired cerebral aneurysm or aortic dissection (n = 943). For OAC-contraindicated patients with a CHA2DS2-VASc ≥2 (N = 16,194), OAC was represcribed in 4075 patients (25%) and was associated with a higher risk of non-intracranial bleeding (HR 1.49; 95% CI 1.37–1.61; p < 0.0001) but no difference in intracranial bleeding. There was a trend toward decreased stroke risk (HR 0.85; 95% CI 0.71–1.02; p 0.09).
Conclusions
Development of contraindication to OAC after diagnosis of AF is common (11.5%), with most events requiring hospitalization. OAC reinitiation was associated with non-intracranial bleeding risk, with a trend toward reduced stroke risk. These data suggest that stroke prevention approaches after major bleeding events could be beneficial if bleeding risk can be successfully mitigated.

Similar content being viewed by others
Abbreviations
- AF:
-
atrial fibrillation
- DOAC:
-
direct oral anticoagulants
- eGFR:
-
estimated glomerular filtration rate
- GI:
-
gastrointestinal
- OAC:
-
oral anticoagulation
- TIA:
-
transient ischemic attack
- VA:
-
Veteran Affairs
References
Fang MC, Go AS, Chang Y, Borowsky LH, Pomernacki NK, Udaltsova N, et al. A new risk scheme to predict warfarin-associated hemorrhage: the ATRIA (anticoagulation and risk factors in atrial fibrillation) study. J Am Coll Cardiol. 2011;58(4):395–401.
Gage BF, Yan Y, Milligan PE, Waterman AD, Culverhouse R, Rich MW, et al. Clinical classification schemes for predicting hemorrhage: results from the National Registry of atrial fibrillation (NRAF). Am Heart J. 2006;151(3):713–9.
Hijazi Z, Oldgren J, Lindback J, et al. The novel biomarker-based ABC (age, biomarkers, clinical history)-bleeding risk score for patients with atrial fibrillation: a derivation and validation study. Lancet. 2016;387(10035):2302–11.
O'Brien EC, Simon DN, Thomas LE, Hylek EM, Gersh BJ, Ansell JE, et al. The ORBIT bleeding score: a simple bedside score to assess bleeding risk in atrial fibrillation. Eur Heart J. 2015;36(46):3258–64.
Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user-friendly score (HAS-BLED) to assess 1-year risk of major bleeding in patients with atrial fibrillation: the euro heart survey. Chest. 2010;138(5):1093–100.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962.
O'Brien EC, Simon DN, Allen LA, et al. Reasons for warfarin discontinuation in the outcomes registry for better informed treatment of atrial fibrillation (ORBIT-AF). Am Heart J. 2014;168(4):487–94.
Hylek EM, Evans-Molina C, Shea C, Henault LE, Regan S. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation. 2007;115(21):2689–96.
Proietti M, Romiti GF, Romanazzi I, Farcomeni A, Staerk L, Nielsen PB, et al. Restarting oral anticoagulant therapy after major bleeding in atrial fibrillation: a systematic review and meta-analysis. Int J Cardiol. 2018;261:84–91.
Hernandez I, Zhang Y, Brooks MM, Chin PK, Saba S. Anticoagulation use and clinical outcomes after major bleeding on Dabigatran or warfarin in atrial fibrillation. Stroke. 2017;48(1):159–66.
Kuramatsu JB, Gerner ST, Schellinger PD, Glahn J, Endres M, Sobesky J, et al. Anticoagulant reversal, blood pressure levels, and anticoagulant resumption in patients with anticoagulation-related intracerebral hemorrhage. JAMA. 2015;313(8):824–36.
Qureshi W, Mittal C, Patsias I, Garikapati K, Kuchipudi A, Cheema G, et al. Restarting anticoagulation and outcomes after major gastrointestinal bleeding in atrial fibrillation. Am J Cardiol. 2014;113(4):662–8.
Nielsen PB, Larsen TB, Skjoth F, Gorst-Rasmussen A, Rasmussen LH, Lip GY. Restarting anticoagulant treatment after intracranial hemorrhage in patients with atrial fibrillation and the impact on recurrent stroke, mortality, and bleeding: a Nationwide cohort study. Circulation. 2015;132(6):517–25.
Nielsen PB, Larsen TB, Skjoth F, Lip GY. Outcomes associated with resuming warfarin treatment after hemorrhagic stroke or traumatic intracranial hemorrhage in patients with atrial fibrillation. JAMA Intern Med. 2017;177(4):563–70.
Staerk L, Lip GY, Olesen JB, et al. Stroke and recurrent haemorrhage associated with antithrombotic treatment after gastrointestinal bleeding in patients with atrial fibrillation: nationwide cohort study. BMJ. 2015;351:h5876.
Nielsen PB, Lundbye-Christensen S, Rasmussen LH, Larsen TB. Improvement of anticoagulant treatment using a dynamic decision support algorithm: a Danish cohort study. Thromb Res. 2014;133(3):375–9.
Cowper DC, Hynes DM, Kubal JD, Murphy PA. Using administrative databases for outcomes research: select examples from VA Health Services Research and Development. J Med Syst. 1999;23(3):249–59.
Smith MW, Joseph GJ. Pharmacy data in the VA health care system. Med Care Res Rev. 2003;60(3 Suppl):92S–123S.
VA Information Resource Center. VIReC research user guide: VHA decision support system clinical National Data Extracts. 2nd ed. U.S. Dept. of Veterans Affairs, Health Services Research and Development Service, VA Information Resource Center: Hines; 2009.
Sohn MW, Arnold N, Maynard C, Hynes DM. Accuracy and completeness of mortality data in the Department of Veterans Affairs. Popul Health Metrics. 2006;4:2.
Turakhia MP, Hoang DD, Xu X, Frayne S, Schmitt S, Yang F, et al. Differences and trends in stroke prevention anticoagulation in primary care vs cardiology specialty management of new atrial fibrillation: the retrospective evaluation and assessment of therapies in AF (TREAT-AF) study. Am Heart J. 2013;165(1):93–101 e101.
Turakhia MP, Santangeli P, Winkelmayer WC, Xu X, Ullal AJ, Than CT, et al. Increased mortality associated with digoxin in contemporary patients with atrial fibrillation: findings from the TREAT-AF study. J Am Coll Cardiol. 2014;64(7):660–8.
Piccini JP, Sinner MF, Greiner MA, Hammill BG, Fontes JD, Daubert JP, et al. Outcomes of Medicare beneficiaries undergoing catheter ablation for atrial fibrillation. Circulation. 2012;126(18):2200–7.
Turakhia MP, Solomon MD, Jhaveri M, Davis P, Eber MR, Conrad R, et al. Burden, timing, and relationship of cardiovascular hospitalization to mortality among Medicare beneficiaries with newly diagnosed atrial fibrillation. Am Heart J. 2013;166(3):573–80.
Steinberg BA, Greiner MA, Hammill BG, Curtis LH, Benjamin EJ, Heckbert SR, et al. Contraindications to anticoagulation therapy and eligibility for novel anticoagulants in older patients with atrial fibrillation. Cardiovasc Ther. 2015;33(4):177–83.
Perino AC, Fan J, Schmitt SK, Askari M, Kaiser DW, Deshmukh A, et al. Treating specialty and outcomes in newly diagnosed atrial fibrillation: from the TREAT-AF study. J Am Coll Cardiol. 2017;70(1):78–86.
Yao X, Gersh BJ, Sangaralingham LR, Kent DM, Shah ND, Abraham NS, et al. Comparison of the CHA2DS2-VASc, CHADS2, HAS-BLED, ORBIT, and ATRIA risk scores in predicting non-vitamin K antagonist oral anticoagulants-associated bleeding in patients with atrial fibrillation. Am J Cardiol. 2017;120(9):1549–56.
Holmes DR, Reddy VY, Turi ZG, Doshi SK, Sievert H, Buchbinder M, et al. Percutaneous closure of the left atrial appendage versus warfarin therapy for prevention of stroke in patients with atrial fibrillation: a randomised non-inferiority trial. Lancet. 2009;374(9689):534–42.
Reddy VY, Doshi SK, Sievert H, Buchbinder M, Neuzil P, Huber K, et al. Percutaneous left atrial appendage closure for stroke prophylaxis in patients with atrial fibrillation: 2.3-year follow-up of the PROTECT AF (watchman left atrial appendage system for embolic protection in patients with atrial fibrillation) trial. Circulation. 2013;127(6):720–9.
Connolly SJ, Eikelboom J, Joyner C, Diener HC, Hart R, Golitsyn S, et al. Apixaban in patients with atrial fibrillation. N Engl J Med. 2011;364(9):806–17.
Lakkireddy D, Afzal MR, Lee RJ, Nagaraj H, Tschopp D, Gidney B, et al. Short and long-term outcomes of percutaneous left atrial appendage suture ligation: results from a US multicenter evaluation. Heart Rhythm. 2016;13(5):1030–6.
Price MJ, Gibson DN, Yakubov SJ, Schultz JC, di Biase L, Natale A, et al. Early safety and efficacy of percutaneous left atrial appendage suture ligation: results from the U.S. transcatheter LAA ligation consortium. J Am Coll Cardiol. 2014;64(6):565–72.
Sievert H, Rasekh A, Bartus K, Morelli RL, Fang Q, Kuropka J, et al. Left atrial appendage ligation in nonvalvular atrial fibrillation patients at high risk for embolic events with inel- igibility for oral anticoagulation: initial report of clinical outcomes. JACC Clin Electrophysiol. 2015;1:465–74.
Passman R, Leong-Sit P, Andrei AC, et al. Targeted anticoagulation for atrial fibrillation guided by continuous rhythm assessment with an insertable cardiac monitor: the rhythm evaluation for anticoagulation with continuous monitoring (REACT.COM) pilot study. J Cardiovasc Electrophysiol. 2016;27(3):264–70.
Waks JW, Passman RS, Matos J, et al. Intermittent anticoagulation guided by continuous atrial fibrillation burden monitoring using dual-chamber pacemakers and implantable cardioverter-defibrillators: results from the tailored anticoagulation for non-continuous atrial fibrillation (TACTIC-AF) pilot study. Heart Rhythm. 2018;15(11):1601–7.
Brambatti M, Connolly SJ, Gold MR, Morillo CA, Capucci A, Muto C, et al. Temporal relationship between subclinical atrial fibrillation and embolic events. Circulation. 2014;129(21):2094–9.
Boriani G, Glotzer TV, Santini M, West TM, de Melis M, Sepsi M, et al. Device-detected atrial fibrillation and risk for stroke: an analysis of >10,000 patients from the SOS AF project (stroke preventiOn strategies based on atrial fibrillation information from implanted devices). Eur Heart J. 2014;35(8):508–16.
Turakhia MP, Ziegler PD, Schmitt SK, Chang Y, Fan J, Than CT, et al. Atrial fibrillation burden and short-term risk of stroke: case-crossover analysis of continuously recorded heart rhythm from cardiac electronic implanted devices. Circ Arrhythm Electrophysiol. 2015;8(5):1040–7.
Funding
Support for VA/CMS data is provided by the Department of Veterans Affairs, Veterans Health Administration, Office of Research and Development, Health Services Research and Development, VA Information Resource Center (Project Numbers SDR 02–237 and 98–004). SentreHeart, Inc. (Redwood City, CA) sponsored the study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclosures
A.C. Perino: Research support from the American Heart Association and Bristol-Myers Squibb/Pfizer. D.W. Kaiser: None. R.J. Lee: consultant to and equity holder for SentreHeart, Inc., Apama Medical (Boston Scientific, Inc), HMicro, Inc. J. Fan: None. M. Askari: None. S.S. Schmitt: None. M.P. Turakhia: Research Grant; Significant; Janssen Pharmaceuticals, Medtronic Inc., AstraZeneca, Veterans Health Administration, Cardiva Medical Inc. Other Research Support; Modest; AliveCor Inc., Amazon, Zipline Medical Inc., iBeat Inc., iRhythm Technologies Inc. Honoraria; Significant; Abbott. Honoraria; Modest; Medtronic Inc., Boehringer Ingelheim, Precision Health Economics, iBeat Inc., Akebia, Cardiva Medical Inc., Medscape/theheart.org.
Disclaimer
The content and opinions expressed are solely the responsibility of the authors and do not necessarily represent the views or policies of the Department of Veterans Affairs.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 35 kb).
Rights and permissions
About this article
Cite this article
Perino, A.C., Kaiser, D.W., Lee, R.J. et al. Incidence and outcomes of patients with atrial fibrillation and major bleeding complications: from the TREAT-AF study. J Interv Card Electrophysiol 62, 133–142 (2021). https://doi.org/10.1007/s10840-020-00873-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00873-0