Abstract
Purpose
To make an in vitro evaluation of the lesion size and depth produced in two different sets of radio frequency energy bipolar delivery: simultaneous biparietal bipolar (SBB) and simultaneous uniparietal bipolar (SUB).
Methods
Two separate prototypes have been built for our purpose: one to be used in SBB mode and the other to be used SUB mode. Forty left atrium samples were taken from the hearts of freshly slaughtered pigs. They were ablated into a simulator ABLABOX, where blood flow, temperature, and contact force were controlled. After being sliced into a cryotome, the samples were digitalized by a flatbed scanner, and the images were analyzed by a computer morphometric software.
Results
Transmural lesions were achieved in 18/20 samples (90%) in SBB, while SUB showed transmurality in 9/20 samples (45%). Overall maximum diameter (DMAX) resulted larger in SUB than in SBB (2.43 ± 0.30 mm, 1.62 ± 0.14 mm, respectively; p < 0.05): Moreover, maximum epicardial and endocardial diameters (DEPI and DENDO, respectively) were wider in SUB group than SBB group (2.28 ± 0.30 mm, 2.26 ± 0.40 and 1.60 ± 0.14 mm, 1.59 ± 0.15 mm, respectively; p < 0.05). We observed the same tendency in lesion depth: The total area and volume (ATOT and VTOT) were broader in SUB group than in SBB one (581.01 ± 65.38 mm/mm2, 58.10 ± 6.53 mm/mm3 and 521.97 ± 73.05 mm/mm2, 52.19 ± 7.30 mm/mm3. respectively; p < 0.05).
Conclusions
In contrast with the smaller lesion sizes, the biparietal bipolar group showed a higher transmurality rate. These findings may suggest a better drive of the energy flow when compared with SUB lesions.
Similar content being viewed by others
1 Introduction
Hybrid ablation (HA) exploits the concomitant effect of epicardial and endocardial procedures performed together by a surgeon and an electrophysiologist. It combines epicardial ablation performed by bilateral thoracotomy to a standard transcatheter endocardial ablation. Apart from joining the advantages of the two procedures, this technique allows the electrophysiologist to test the ablation, to add touch-up ablation if necessary and to reach part of the heart that cannot be ablated by the surgeons [1].
Radio frequency (RF) is the energy source mainly employed, and RF tools are based on unipolar or bipolar technology. Moreover, the endocardium lesions are obtained through the use of unipolar unidirectional punctual catheters, while epicardial ones are achieved through the use of bipolar unidirectional RF implemented in different tools. The goal of all the techniques employed in the treatment of atrial fibrillation (AF) is the achievement of transmural lesions that are considered the indispensable requirement for durable AF-free conditions [2, 3]. HA significantly improved 1-year follow-up in patients [4], but the results are not still acceptable in terms of the rate of freedom from recurrence, particularly in long-standing persistent AF [5].
Nonetheless, bipolar tools used in the hybrid ablation setting may not exploit the entire potential of this new technique, and often, the tissue penetration is limited only to a thin shallow rim [6]. We hypothesize that the settlement of the tissue interposed between the ablating poles (biparietal configuration) may result in a higher rate of transmural lesions. The objective of the present study is to compare in vitro a biparietal bipolar prototype to a uniparietal bipolar catheter in a simultaneous ablation setting.
2 Material and methods
2.1 The in vitro simulator
For the present study, we used a simulator (ABLABOX, IDEE—Instrument Development Engineering and Evaluation, Maastricht University, NL), previously described (Fig. 1) [7].
a The ABLABOX overview. b Particular of the ablation area: (1) catheter holding system, with pressure sensor (2). The holder is free to move over a couple of rails (3) with an adjustable stop system. c Placement of the sample into the simulator: the sample is placed between two plastic holding supports, both with a central open to let the tips of the catheters facing the tissue. The closure is obtained by the use of neodymium magnets embedded into the plastic frame. d Endocardial mimicking chamber: (1) blood flow pump inlet, (2) outlet, (3) adjustable magnetic stirrer motor, (4) magnetic locking tissue sample holder
2.2 The prototypes
2.2.1 Biparietal bipolar
A 3D printed polylactic acid (PLA) cylindrical (30 mm × 0.80 mm external diameter) electrode supports have been printed (Fig. 2(a)). A 2.5-cm length × 0.4 mm in diameter cylindrical metal rods have been placed inside the holders, working as the electrodes (Fig. 2(b, c)). The whole package, including the electric connections, has been included in a hollow aluminum cylinder (20 cm length × 0.95 cm external diameter) (Fig. 2 (d)) to be mounted in the simulator during the experiment.
Catheter assembly sequences in SBB (simultaneous biparietal bipolar) setting and SUB (simultaneous uniparietal bipolar) setting. (a) 3D printed supports, (b) electrode placement into the supports, (c) electric connections, and (d) placement of the system into an aluminum handle ready to be mounted into the simulator, (e) 3D printed supports for uniparietal technique, (f) electrodes placement into the support, (g) electric wiring connections, final assembly into aluminum handle
2.2.2 Uniparietal bipolar
The prototype for the uniparietal bipolar technique has the same external shape and dimensions, except the 3D printed electrode support that is shaped to embrace and leave electrically isolated a couple of electrodes working in bipolar uniparietal way (Fig. 2 (e)). Indeed, the same 4-mm metal rod has been cut on its length with a 1.2-mm-thick cutting disc to respect the external dimensions of the electrode of the biparietal bipolar catheter (Fig. 2 (f)). Likewise, the holder and the electrodes, together with their electric connections, are included in the same shape hollow cylinder of the previously described catheter (Fig. 2 (g, h)). The prototypes were both connected to a standard bipolar radio frequency generator.
2.3 Samples
Samples came from freshly slaughtered pigs, and left atria were isolated to be employed in the present study. Concerning the sections done by the personal of the company while slaughtering the animals, the lesions were performed in the left atrium inferior posterior wall, on the broad junction (difference of species with human left atrium) [8], to the pulmonary venous compartment avoiding when possible the pectinate muscles (Fig. 3).
After being washed to remove the residual blood with NaCl (B. Braun, Melsungen, Hessen, Germany), they were put into a transport medium RPMI 1640 (Sigma-Aldrich, St. Louis, MO, USA). Samples were randomly assigned to two groups of study: (1) simultaneous biparietal bipolar (SBB), where the poles were placed on the opposite sides of the sample and the radio frequency crossing the sample width, and (2) simultaneous uniparietal bipolar (SUB) mode, where the electrodes were placed on only a side of the sample (Fig. 4). Twenty samples of each group were employed for a total of 40 samples.
2.4 Experimental setup
The power console had a fixed RF output (28.5 W at 114 Ω load) that was kept the same for both groups. The control of the delivery and amount of RF was controlled by an internal dynamic monitoring algorithm checking the impedance and stopping the energy delivery after transmurality was reached. In the SBB group, we used two identical consoles for the simultaneous RF application. The simulator settings were fixed in 5 l/min of blood flow to mimic the human cardiac output [9], contact forces of 300 g each side, temperature at 38 °C, and stirrer motor at 400 RPM.
2.5 Morphometric evaluation of myocardial tissue ablation
The samples harvested were put in 10% neutral buffered formalin for 2 days. Hereafter, the specimens were included in the Tissue-Tek® OCT™ medium and sliced by a Leica CM 3050 cryostat (Leica Biosystems, Wetzlar, Germany) at − 20 °C. The thickness of every single slice was fixed to 0.1 mm. Furthermore, the slices so obtained, were laid down on a transparent acetate sheet, left drying at room temperature, and covered with another sheet. Hereafter, a flatbed scanner (Perfection V39 Scanner, Epson America, Inc., 3840 Kilroy Airport Way, Long Beach, CA 90806) was employed for scanning the sheets at 600 dpi of resolution. Furthermore, the digitalized images were imported in an image processing software (ImageJ version 1.48 software; National Institutes of Health, Bethesda, MD, USA) to be measured. In each sample, the following parameters were calculated: the maximum diameter (DMAX), meaning the largest diameter measure within the whole stack of slices, and the maximum epicardial and endocardial diameters (DEPI and DENDO, respectively), indicating the largest measure of the diameter within endocardial and epicardial sides. Also, the total area (ATOT), calculated as the sum of the ablated area of each tissue slice, was determined. The total volume (VTOT) was calculated by multiplying the total area (ATOT) by its fixed thickness value setup in the cryostat (0.1 mm) (Table 1).
The replicability and objectiveness assessment of the measurements was completed by interobserver (GP) and intraobserver evaluation (FM).
2.6 Statistical analysis
The distribution of data was evaluated by using the Shapiro-Wilk normality test (StatsDirect Ltd., 9 Mountwood Road, Birkenhead, Merseyside CH42 8NQ, UK). If from normal distribution, data were expressed as mean plus/minus standard deviation. If not, the median (lower-upper quartile) was expressed. The comparison of the measurements of the groups was tested through the unpaired t test or Mann-Whitney test. The measurements were indexed by the thickness (average) of all the samples. Linear dimensions (DMAX, DEPI, DENDO) were expressed in millimeters per millimeter, while surface (ATOT) and volume (VTOT) dimensions were expressed as square millimeters per millimeter and cubic millimeters per millimeter. The intraobserver (FM) and interobserver variabilities (GP) were tested for ATOT and DEPI in ten casually sorted specimen using κ-statistics. The value stands between κ 0 (no agreement) and 1 (perfect agreement).
3 Results
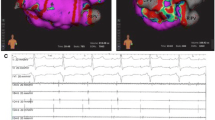
No audible steam pops were encountered during the procedure, and no perforations were observed. The slices obtained formed a progressive sequence where modification of the shape of the lesion was appreciated (Fig. 5).
Progressive slice sequence. Ablation lesion formation progression while slicing the samples perpendicular to the direction of the catheters. The numbers show the lesion shape and dimensions in the study groups at that particular number of the slice pack. The SBB group shows a continuity of the lesions throughout the thickness of the sample. The SUB group shows a discontinuity in the progression of the lesion
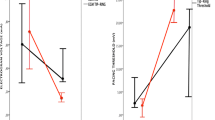
Both the intra- and interobserver variabilities for the measurement of DEPI (k = 0.97, k = 0.91, respectively) and ATOT (k = 0.95, k = 0.89, respectively) were low, indicating an excellent repeatability and reproducibility of the measurements. Samples showed a thickness of 4.36 ± 0.20 mm in SBB and 4.20 ± 0.20 mm in SUB, with no significant difference (p > 0.05). Transmural lesions were detected in 18 samples over 20 (90%) in SBB group, while in SUB, transmural lesions were present in 9 samples over 20 (45%) (Fig. 6).
The overall DMAX was significantly smaller in SBB than in SUB (1.62 ± 0.14 mm and 2.43 ± 0.30 mm, respectively; p < 0.05). Moreover, the DEPI and DENDO in SBB group (1.60 ± 0.14 mm and 1.59 ± 0.15, respectively) were smaller than DEPI and DENDO of SUB (2.28 ± 0.30 and 2.26 ± 0.40, respectively; all p < 0.05).
The ATOT in SBB was smaller than ATOT in SUB (521.97 ± 73.05 mm/mm2 and 581.01 ± 65.38 mm/mm2, respectively; p < 0.05). Likewise, the VTOT was smaller in SBB compared with SUB (52.19 ± 7.30 mm/mm3 and 58.10 ± 6.53 mm/mm3, respectively; p < 0.05).
4 Discussion
In the present study, we tested in vitro two different approaches of bipolar application: simultaneous biparietal bipolar and uniparietal bipolar settings. The results we obtained show a high rate of transmurality in the biparietal bipolar group and smaller sizes of the lesions induced in comparison with the uniparietal bipolar group. These aspects may suggest that the RF spreads broad mainly over the first few layers of the tissue, but it does not penetrate deeply. Only the bipolar biparietal setting seems to ensure a better propagation along the whole thickness of the tissue.
The difference in unipolar and bipolar settings resides in the different placements of the electric poles. Indeed, in unipolar mode, the energy flows from an emitter placed at the top of the catheter and an indifferent (ground) pole represented by the large electrode placed generally on the back of the patient. Contrarily, in bipolar mode, the positive and negative poles are placed side by side at the end of the catheter. In uniparietal setting, both unipolar and bipolar settings provide the poles to be displaced only from one side of the tissue (radio frequency catheter ablation or epicardial tools). In contrast, the biparietal mode provides the electrodes facing the tissue from the opposite side, resulting in the tissue being interposed between the poles (biparietal bipolar clamp).
Also, the behavior of the energy differs significantly. Indeed, in unipolar mode, RF spreads centrifugally from the emitter to the indifferent pole, while in bipolar technique, the RF diffuses from the close poles placed on the top of the catheter [10, 11].
From the clinical point of view, most ablation procedures are performed through catheter ablation, and apart from the use of cryogenic energy for ablating the pulmonary veins in the early onset of paroxysmal AF [12], RF energy is widely used for the treatment of AF. The application of RF catheter ablation is limited to unipolar uniparietal delivery. In contrast, in the epicardial thoracoscopic approach, cardiac surgeons can use both uniparietal and biparietal bipolar settings. The goal of all the ablation procedures is the achievement of transmural lesions [3, 13] leading to electric block. Remarkably, lesion gaps, even smaller than 1 mm, either lead to an incomplete electric isolation of the atrium or represent themselves a pro-arrhythmic element [14, 15].
The bipolar setting in ablation procedures seems to offer a higher rate of transmurality [16, 17] in comparison with unipolar technique. Especially, the use of biparietal bipolar clamp in either open chest surgery or mini-invasive thoracoscopic approach seems to represent the gold standard in AF, creating transmural, long-lasting, and reliable lesions [3, 18]. Another important aspect is represented by the lacking of the cooling circulating blood flow effect. Indeed, in bipolar setting, the electrodes are side by side and very closed to each other. Thus, the energy flow results in a very focused and narrow path between the poles. The significant consequence is a faster, useful ablation temperature reach with reducing over thermal risks of neighbor tissues [16].
Nonetheless, it must be addressed that bipolar tools used in the clinic, except biparietal bipolar clamp, do not include the interposition of the tissue between the electrodes. Remarkably, the biparietal setting in the bipolar clamps seems to represent the fastest and reliable tool to obtain transmural lesions in open-chest procedure [3, 19, 20]. The use of the clamp in this latter procedure provides a cardiopulmonary bypass followed by the insertion of one jaw of the clamp inside the atrium, thus a biparietal bipolar setting. Nonetheless, while with this setup, the clamp is a true biparietal; when it is employed only epicardically, it surrounds the pulmonary veins, interposing only the epicardium between the jaws. Therefore, this setting cannot be considered as genuinely biparietal.
The findings of the present study confirm that the biparietal bipolar setting shows a higher transmural lesions rate in comparison with the uniparietal technique. Contrarily, compared with the biparietal setting, the linear dimension of the lesions obtained (DMAX, DEPI, DENDO) resulted broader in the uniparietal group. Likewise, the lesion depth (ATOT, VTOT) resulted wider in uniparietal setting than the biparietal one. These results may be clarified with the evidence that the RF current density is inversely proportional to the square of the distance between the electrodes, and the density is higher along the shortest distance between the electrodes [21,22,23]. As a consequence, the closeness of the poles when in the biparietal setting may result in a better spread through the wall tissue instead of uniparietal bipolar mode. Likewise, the same results may suggest that the diffusion of the energy in the uniparietal bipolar setting group is more randomly driven, causing a broader lesion in size and depth, but not reaching high transmurality.
However, our findings confirm that for tissue thickness lower than 4.2 mm, the result with the SUB is comparable with SBB. Indeed, these devices are widely used in clinical practice. Nonetheless, multiple simultaneous applications, long ablation times, and high contact force pressures are necessary to reach reliable lesions [24, 25].
Since AF patients have been reported to have thinner atrial walls, tissue perforation might be an issue when a transmural lesion is obtained. We have neither observed signs of damage macroscopically (carbonization) nor have we experienced steam pops. It has been previously demonstrated in ex vivo experiments that the perforation forces are higher in atria compared with swine [26], and the contact forces employed by these authors forces were, however, significantly lower than those applied in our experiments. Therefore, this might suggest that our setup was safe. Nonetheless, this warrants further research.
4.1 Clinical repercussions
The two-stage hybrid results in an AF freedom of 56% without the use of anti-arrhythmic drugs [27]. Experts agree that new, improved tools are necessary to a complete isolation o the left atrium [28]. One of the main drawbacks of the tools in use is the incompleteness of linear lesion leading to gaps and failing a complete LA isolation [19]. With the magnetic coupling and with a biparietal design, it would be possible to make a complete one-stage LA isolation. The magnetic force should also allow to squeeze the tissue between the poles theoretically, making the thickness of the atrial wall and the epicardial fat to not influence the effectiveness of the lesion.
Long-lasting transmural PV isolation is obtained with bipolar clamps that use bipolar bidirectional radio frequency [20], and our approach implements the use of such bipolar bidirectional clamps that can be offered to patients with or long-standing persistent AF that is more difficult to treat. Our findings suggest that bipolar biparietal setting might represent a promising technique to achieve reliable endo-epicardial lesions. A key issue to obtain optimal results is the perfect alignment and stability of the poles, and the use of (electro)magnetism might represent a possible solution.
The clinical application of true biparietal bipolar HA is far for being established. Research on a custom-made bipolar HA prototype is ongoing, keeping into consideration different approach strategies.
4.2 Limitations
This study has some limitations that need to be mentioned. First, we used ex vivo tissue, and the absence of microcirculation, acting like a heat sink, could have led to an overestimation of our results. Second, the RF generator used in the study has not been built to be employed in the biparietal bipolar setting. Hence, the property algorithm of the manufacturer controlling RF delivery could have driven higher/lower output based on registered impedance, and so in the reading of our findings, it must be taken into account. Third, the prototype tips had a different shape from the catheters commonly used for this purpose. This evidence, due to the fixed energy output of the generator, could have led to a decreased/increased power distribution along the electrodes. Fourth, we evaluated the necrosis only from a visual observation; we did not include a histological evaluation such as the TUNEL (terminal deoxynucleotidyl transferase [TdT] dUTP nick end labeling) because of the number of layers produced. Fifth, we did not measure the temperatures reached during the ablation. This might have given more insights since the physics of lesion formation between the catheters can be different.
Finally, the tissue employed for this study came from 1-year-old healthy pig breed for human consumption. Clearly, these hearts did not show pathological conditions typical of AF, like the fibrosis development.
5 Conclusion
In our in vitro experiment, the biparietal technique results in better tissue penetration, leading to higher transmurality lesions rate. In the uniparietal mode, lesions are broader in size and depth, but they do not reach the same transmurality rate of the first group, suggesting a more random drive of energy through the wall tissue. These findings might be a call for the use of this setting in the clinical practice. Nonetheless, the complexity of the clinical scenario makes this application very challenging, requiring further research to test its real clinical feasibility and applicability.
Data availability
The authors declare to have data available.
References
La Meir M, Gelsomino S, Lorusso R, Luca F, Pison L, Parise O, et al. The hybrid approach for the surgical treatment of lone atrial fibrillation: one-year results employing a monopolar radiofrequency source. J Cardiothorac Surg. 2012;7:71. https://doi.org/10.1186/1749-8090-7-71.
Cabrera JA, Pizarro G, Sánchez-Quintana D. Transmural ablation of all the pulmonary veins: is it the Holy Grail for cure of atrial fibrillation? Eur Heart J. 2010;31(22):2708–11. https://doi.org/10.1093/eurheartj/ehq241 European Heart Journal.
Melby SJ, Schuessler RB, Damiano RJ Jr. Ablation technology for the surgical treatment of atrial fibrillation. ASAIO J. 2013;59(5):461–8. https://doi.org/10.1097/MAT.0b013e3182a394f1.
van der Heijden CAJ, Vroomen M, Luermans JG, Vos R, Crijns HJGM, Gelsomino S, et al. Hybrid versus catheter ablation in patients with persistent and longstanding persistent atrial fibrillation: a systematic review and meta-analysis†. Eur J Cardiothorac Surg. 2019;56(3):433–43. https://doi.org/10.1093/ejcts/ezy475 European Journal of Cardio-Thoracic Surgery.
Pison L, La Meir M, van Opstal J, Blaauw Y, Maessen J, Crijns HJ. Hybrid thoracoscopic surgical and transvenous catheter ablation of atrial fibrillation. J Am Coll Cardiol. 2012;60(1):54–61. https://doi.org/10.1016/j.jacc.2011.12.055.
Issa ZF, Miller JM, Zipes DP. Chapter 7 - ablation energy sources. In: Issa ZF, Miller JM, Zipes DP, editors. Clinical arrhythmology and electrophysiology: a companion to Braunwald’s heart disease. 2nd ed. Philadelphia: W.B. Saunders; 2012. p. 144–63.
Lozekoot PW, de Jong MM, Parise O, Matteucci F, Luca F, Kumar N, et al. The ABLA-BOX: an in vitro module of hybrid atrial fibrillation ablation. Innovations (Phila). 2016;11(3):201–9. https://doi.org/10.1097/IMI.0000000000000256.
Crick SJ, Sheppard MN, Ho SY, Gebstein L, Anderson RH. Anatomy of the pig heart: comparisons with normal human cardiac structure. J Anat. 1998;193(Pt 1):105–19. https://doi.org/10.1046/j.1469-7580.1998.19310105.x.
Parfitt JM. Clinical practice: Essentials of oxygenation: implications for clinical practice. 1993;58(6):1198. https://doi.org/10.1016/s0001-2092(07)64924-2.
Chang W, Lee JM, Lee SM, Han JK. No-touch radiofrequency ablation: a comparison of switching bipolar and switching monopolar ablation in ex vivo bovine liver. Korean J Radiol. 2017;18(2):279–88. https://doi.org/10.3348/kjr.2017.18.2.279.
Saint LL, Lawrance CP, Okada S, Kazui T, Robertson JO, Schuessler RB, et al. Performance of a novel bipolar/monopolar radiofrequency ablation device on the beating heart in an acute porcine model. Innovations (Phila). 2013;8(4):276–83. https://doi.org/10.1097/IMI.0b013e3182a77f2b.
Packer DL, Kowal RC, Wheelan KR, Irwin JM, Champagne J, Guerra PG, et al. Cryoballoon ablation of pulmonary veins for paroxysmal atrial fibrillation. J Am Coll Cardiol. 2013;61(16):1713–23. https://doi.org/10.1016/j.jacc.2012.11.064.
Bugge E, Nicholson IA, Thomas SP. Comparison of bipolar and unipolar radiofrequency ablation in an in vivo experimental model. Eur J Cardiothorac Surg. 2005;28(1):76–80. https://doi.org/10.1016/j.ejcts.2005.02.028 European Journal of Cardio-Thoracic Surgery.
Melby SJ, Lee AM, Zierer A, Kaiser SP, Livhits MJ, Boineau JP, et al. Atrial fibrillation propagates through gaps in ablation lines: implications for ablative treatment of atrial fibrillation. Heart Rhythm. 2008;5(9):1296–301. https://doi.org/10.1016/j.hrthm.2008.06.009.
Saksena S, Damiano RJ, Estes NAM III, Marchlinski FE. Interventional cardiac electrophysiology: a multidisciplinary approach. Minneapolis, Minnesota: Cardiotext Publishing; 2015.
Melby SJ, Gaynor SL, Lubahn JG, Lee AM, Rahgozar P, Caruthers SD, et al. Efficacy and safety of right and left atrial ablations on the beating heart with irrigated bipolar radiofrequency energy: a long-term animal study. J Thorac Cardiovasc Surg. 2006;132(4):853–60. https://doi.org/10.1016/j.jtcvs.2006.05.048.
Voeller RK, Zierer A, Lall SC, Sakamoto S-I, Schuessler RB, Damiano RJ Jr. Efficacy of a novel bipolar radiofrequency ablation device on the beating heart for atrial fibrillation ablation: a long-term porcine study. J Thorac Cardiovasc Surg. 2010;140(1):203–8. https://doi.org/10.1016/j.jtcvs.2009.06.034.
Lawrance CP, Henn MC, Damiano RJ Jr. Surgical ablation for atrial fibrillation: techniques, indications, and results. Curr Opin Cardiol. 2015;30(1):58–64. https://doi.org/10.1097/HCO.0000000000000125.
Maesen B, Weberndörfer V, Bidar E, Linz D. The importance of bipolar bidirectional radiofrequency in surgical AF ablation. Int J Cardiol Heart Vasc. 2020;26:100478. https://doi.org/10.1016/j.ijcha.2020.100478.
Velagic V, Asmundis CDE, Mugnai G, Irfan G, Hunuk B, Stroker E, et al. Repeat procedures after hybrid thoracoscopic ablation in the setting of longstanding persistent atrial fibrillation: electrophysiological findings and 2-year clinical outcome. J Cardiovasc Electrophysiol. 2016;27(1):41–50. https://doi.org/10.1111/jce.12837.
Zipes DP, Jalife J. Cardiac electrophysiology: from cell to bedside. 4th ed. Philadelphia: Saunders; 2004.
Kovoor P, Daly M, Pouliopoulos J, Dewsnap MB, Eipper V, Ross DL. Effect of inter-electrode distance on bipolar intramural radiofrequency ablation. 2005;28(6):514–20. https://doi.org/10.1111/j.1540-8159.2005.09446.x.
Duncan DI, Kreindel M. Basic radiofrequency: physics and safety and application to aesthetic medicine. Aesthet Dermatol. 2015;2:1–22. https://doi.org/10.1159/000362747.
Wood MA, Ellenbogen AL, Pathak V, Ellenbogen KA, Kasarajan V. Efficacy of a cooled bipolar epicardial radiofrequency ablation probe for creating transmural myocardial lesions. J Thorac Cardiovasc Surg. 2010;139(2):453–8. https://doi.org/10.1016/j.jtcvs.2009.06.028.
Lee AM, Aziz A, Clark KL, Schuessler RB, Damiano RJ. Chronic performance of a novel radiofrequency ablation device on the beating heart: limitations of conduction delay to assess transmurality. J Thorac Cardiovasc Surg. 2012;144(4):859–65. https://doi.org/10.1016/j.jtcvs.2012.01.001.
Quallich SG, Van Heel M, Iaizzo PA. Optimal contact forces to minimize cardiac perforations before, during, and/or after radiofrequency or cryothermal ablations. Heart Rhythm. 2015;12(2):291–6. https://doi.org/10.1016/j.hrthm.2014.11.028.
Haywood GA, Varini R, Osmancik P, Cireddu M, Caldwell J, Chaudhry MA, et al. European multicentre experience of staged hybrid atrial fibrillation ablation for the treatment of persistent and long-standing persistent atrial fibrillation. Int J Cardiol Heart Vasc. 2020;26:100459. https://doi.org/10.1016/j.ijcha.2019.100459.
Cox JL. Having seen it all: my vision of atrial fibrillation treatment in 2022. Eur J Cardiothorac Surg. 2018;53(suppl_1):i39–40. https://doi.org/10.1093/ejcts/ezx499 European Journal of Cardio-Thoracic Surgery.
Code availability
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors actively contributed to the paper in the following domains: conception or design of the work, data collection, data analysis, interpretation, drafting the article, critical revision of the article, and final approval of the version to be published.
Corresponding author
Ethics declarations
Conflict of interest
MLM is a consultant for Atricure. BM has a speaking contract with Atricure. All the other authors have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Matteucci, F., Maesen, B., De Asmundis, C. et al. Comparison between biparietal bipolar and uniparietal bipolar radio frequency ablation techniques in a simultaneous procedural setting. J Interv Card Electrophysiol 61, 567–575 (2021). https://doi.org/10.1007/s10840-020-00852-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-020-00852-5