Abstract
Purpose
The EVOCAVDS trial aimed to quantify the paradoxal atrioventricular (AV) conduction time lengthening in sinus node (SD) patients (pts) paced in AAIR-based pacing mode.
Methods
SD pts, implanted with dual-chamber pacemaker programmed in AAIR-based pacing mode, were randomized in two arms for a 1-month period: the low atrial pacing (LAP; basic rate at 60 bpm, dual sensor with minimal slope) and the high atrial pacing (HAP; basic rate at 70 bpm, dual sensor with optimized slope, overdrive pacing) arm. At 1 month, crossover was performed for an additional 1-month period. AV conduction time, AV block occurrence and AV conduction time adaptation during exercise were ascertained from device memories at each follow-up.
Results
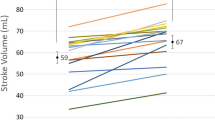
Seventy-nine pts participated to the analysis (75 ± 8 years; 32 male; PR = 184 ± 38 ms; bundle branch block n = 12; AF history n = 36; antiarrhythmic treatment n = 53; beta-blockers n = 27; class III/Ic n = 18; both n = 8). The mean AV conduction time was significantly greater during the HAP (275 ± 51 ms) vs. LAP (263 ± 49 ms) period (p < 0.0001). Class III/Ic drugs were the only predictors of this abnormal behaviour. Degree II/III AV blocks occurred in 49 % of pts in the HAP vs. 19 % in the LAP period (p < 0.0001). Fifty-two patients (66 %) presented a lengthening of AV conduction time during exercise.
Conclusion
AAIR-based pacing in SD pts may induce a significant lengthening of pts’ AV conduction time, including frequent abnormal adaptation of AV conduction time during exercise.



Similar content being viewed by others
References
Andersen, H. R., Thuesen, L., Bagger, J. P., Vesterlund, T., & Thomsen, P. E. (1994). Prospective randomized trial of atrial versus ventricular pacing in sick sinus syndrome. Lancet, 344, 1523–1528.
Andersen, H. R., Nielsen, J. C., Thomsen, P. E., Thuesen, L., Mortensen, P. T., Vesterlund, T., et al. (1997). Long term follow up of patients from a randomized trial of atrial versus ventricular pacing in sick sinus syndrome. Lancet, 350, 1210–1216.
Connolly, S. J., Kerr, C. R., Gent, M., Roberts, R. S., Yusuf, S., Gillis, A. M., et al. (2000). Effects of physiologic pacing versus ventricular pacing on the risk of stroke and death due to cardiovascular causes. Canadian Trial of Physiological Pacing Investigators. The New England Journal of Medicine, 342, 1385–1391.
Lamas, G. A., Lee, K. L., Sweeney, M. O., Silverman, R., Leon, A., Yee, R., et al. (2002). Mode selection trial in sinus dysfunction. Ventricular pacing or dual chamber pacing for sinus node dysfunction. The New England Journal of Medicine, 346, 1854–1862.
Toff, W. D., Camm, A. J., Skehan, J. D., & United Kingdom Pacing and Cardiovascular Events Trial Investigators. (2005). Single chamber versus dual chamber pacing for high grade atrioventricular block. The New England Journal of Medicine, 353, 145–155.
Brandt, J., Anderson, H., Fahraeus, T., & Schuller, H. (1992). Natural history of sinus node disease treated with atrial pacing in 213 patients: Implications for selection of stimulation mode. Journal of the American College of Cardiology, 20, 633–639.
Blanc, J. J., De Roy, L., Mansourati, J., Poezevara, Y., Marcon, J. J., Schoels, W., et al. (2004). Atrial pacing for prevention of atrial fibrillation: Assessment of simultaneously implemented algorithms. Europace, 6, 371–379.
Nielsen, J. C., Kristensen, L., Andersen, H. R., Mortensen, P. T., Pedersen, O. L., & Pedersen, A. K. (2003). A randomized comparison of atrial and dual-chamber pacing in 177 consecutive patients with sick sinus syndrome: Echocardiographic and clinical outcome. Journal of the American Colledge of Cardiology, 42, 614–623.
Sweeney, M. O., Hellkamp, A. S., Ellenbogen, K. A., Greenspon, A. J., Freedman, R. A., Lee, K. L., et al. (2003). Adverse effect of ventricular pacing on heart failure and atrial fibrillation among patients with normal baseline QRS duration in a clinical trial of pacemaker therapy for sinus node dysfunction. Circulation, 107, 2932–2937.
Andersen, H. R., Nielsen, J. C., Thomsen, P. E., Thuesen, L., Vesterlund, T., Pedersen, A. K., et al. (1998). Atrioventricular conduction during long-term follow-up of patients with sick sinus syndrome. Circulation, 98, 1315–1321.
Fröhlig, G., Gras, D., Victor, J., Mabo, P., Galley, D., Savoure, A., et al. (2006). Use of a new cardiac pacing mode designed to eliminate unnecessary ventricular pacing. Europace, 8, 96–101.
Davy, J. M., Hoffmann, E., Frey, A., Jocham, K., Rossi, S., Dupuis, J. M., et al. (2012). Near elimination of ventricular pacing in SafeR mode compared to DDD modes: A randomized study on 422 patients. Pacing and Clinical Electrophysiology. doi:10.1111/j.1540-8159.2011.03327.x
Gregoratos, G., Abrams, J., Epstein, A. E., Freedman, R. A., Hayes, D. L., Hlatky, M. A., et al. (2002). Guidelines update for implantation of cardiac pacemakers and arrhythmias devices: Summary article: A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines (ACC/AHA/NASPE Committee to update the 1998 pacemaker guidelines). Circulation, 106, 2145–2161.
Savouré, A., Fröhlig, G., Galley, D., Defaye, P., Reuter, S., Mabo, P., et al. (2005). A new dual-chamber pacing mode to minimize ventricular pacing. Pacing and Clinical Electrophysiology, 28(Suppl 1), S43–S46.
Davy, J. M., Hoffmann, E., Frey, A., Jocham, K., Rossi, S., Dupuis, J. M., et al. (2012). Near elimination of ventricular pacing in SafeR mode compared to DDD modes: A randomized study of 422 patients. Pacing and Clinical Electrophysiology, 35, 392–402.
Page, E., Bonnet, J. L., & Durand, C. (2000). Comparison of metabolic expenditure during CAEP versus test adapted to aerobic capacity (Harbor test) in elderly healthy individuals. Pacing and Clinical Electrophysiology, 2, 1772–1777.
Bonnet, J. L., Géroux, L., & Cazeau, S. (1998). Evaluation of a dual sensor rate responsive pacing system based on a new concept. PACE, 21, 2198–2203.
Barbieri, D., Percoco, G. F., Toselli, T., Guardigli, G., Ansani, I., & Antonioli, G. E. (1990). AV delay and exercise stress tests: Behavior in normal subjects. Pacing and Clinical Electrophysiology, 13, 1724–1727.
Daubert, C., Ritter, P., Mabo, P., Ollitrault, J., Descaves, C., & Gouffault, J. (1986). Physiological relationship between AV interval and heart rate in healthy subjects: Applications to dual chamber pacing. Pacing and Clinical Electrophysiology, 9(6), 1032–1039.
Kui, C. T., Wu, J. M., Lin, K. H., & Young, M. L. (2001). The effect of aging on AV nodal recovery properties. Pacing and Clinical Electrophysiology, 24(2), 194–198.
Taneja, T., Mahnert, B. W., Passman, R., Goldberger, J., & Kadish, A. (2001). Effects of sex and age on electrocardiographic and cardiac electrophysiological properties in adults. Pacing and Clinical Electrophysiology, 24(1), 16–21.
Ishikawa, T., Kimura, K., Miyazaki, N., Tochikubo, O., Usui, T., Kashiwagi, M., et al. (1992). Diastolic mitral regurgitation in patients with first degree atrioventricular block. Pacing and Clinical Electrophysiology, 15, 1927–1931.
Cheng, S., Keyes, M. J., Larson, M. G., McCabe, E. L., Newton-Cheh, C., et al. (2009). Long term outcomes in individuals with prolonged PR interval or first degree atrioventricular block. Journal of the American Medical Association, 301, 2571–2577.
Kristensen, L., Nielsen, J. C., Pedersen, A. K., Mortensen, P. T., & Andersen, H. R. (2001). AV block and changes in pacing mode during long term follow-up of 399 consecutive patients with sick sinus syndrome treated with an AAIR pacemaker. Pacing and Clinical Electrophysiology, 24, 358–365.
Veasey, R. A., Arya, A., Silberbauer, J., Sharma, V., Lloyd, G. W., Patel, N. R., et al. (2011). The relationship between right ventricular pacing and atrial fibrillation burden and disease progression in patients with paroxysmal atrial fibrillation: The long-MinVPACE study. Europace. doi:10.1093/europace/eud463
Sweeney, M. O., Bank, A. J., Nsah, E., Koullick, M., Zeng, Q. C., Hettrick, D., et al. (2007). Minimizing ventricular pacing to reduce atrial fibrillation in sinus node disease. The New England Journal of Medicine, 357, 1000–1008.
Vardas, P. A., Auricchio, A., Blanc, J. J., Daubert, J. C., Drexler, H., Ector, H., et al. (2007). Guidelines for cardiac pacing and cardiac resynchronization therapy. European Heart Journal, 28, 2256–2295.
Nielsen, J. C., Thomsen, P. E. B., Hojberg, S., Moller, M., Vesterlund, T., Dalsgaard, D., et al. (2011). A comparison of single-lead atrial pacing with dual-chamber pacing in sick sinus syndrome. European Heart Journal, 32, 686–696.
Schwaab, B., Fröhlig, G., Pistorius, C., Schwerdt, H., & Schieffer, H. (1999). AV conduction with atrial rate adaptative pacing in the bradycardia tachycardia syndrome. Pacing and Clinical Electrophysiology, 22(10), 1502–1509.
Mabo, P., Pouillot, C., Kermarrec, A., Lelong, B., Lebreton, H., & Daubert, J. C. (1991). Lack of physiological adaptation of the atrioventricular interval to heart rate in patients chronically paced in the AAIR mode. Pacing and Clinical Electrophysiology, 14(12), 2133–2142.
Gallik, D. M., Guidry, G. W., Mahmarian, J. J., Verani, M. S., & Spencer, W. H., III. (1994). Comparison of ventricular function in atrial rate adaptative versus dual chamber rate adaptative pacing during exercise. Pacing and Clinical Electrophysiology, 17(2), 179–185.
Vardas, P. E., Simantirakis, E. N., Parthenakis, F. I., Chrysostomakis, S. I., Skalidis, E. I., & Zuridakis, E. G. (1997). AAIR versus DDDR pacing in patients with impaired sinus node chronotropy: An echocardiographic and cardiopulmonary study. Pacing and Clinical Electrophysiology, 20(7), 1762–1768.
Dulk, K. D., Lindemans, F. W., Brugada, P., Smeets, J. L. R. M., & Wellens, H. J. J. (1998). Pacemaker syndrome with AAI rate variable pacing: Importance of atrioventricular conduction properties, medication, and pacemaker programmability. Pacing and Clinical Electrophysiology, 11(8), 1226–1233.
Acknowledgments
This study was sponsored by Sorin CRM SAS, Clamart, France. The authors thank Pierre-Henri Siot for his contribution to statistical analysis, and Pelle Stolt, PhD and Anne Rousseau-Plasse, PhD, for their assistance in the preparation of the manuscript.
Conflicts of interest
Philippe Mabo, MD, Jean-Pierre Cebron, MD, Aude Solnon, MD, Aude Tassin, MD, and Daniel Gras, MD, received research grant from Sorin CRM SAS for their participation to the EVOCAV DS study. Philippe Mabo, MD, received consulting fees from Sorin CRM SAS. Laurence Graindorge received a salary from Sorin CRM SAS as employee.
Participating investigators and institutions
The participating investigators and institutions are the following: for CHU Rennes—Christophe Leclercq, MD, PhD, Philippe Mabo, MD and Aude Solnon, MD; Nouvelles Cliniques Nantaises—Marc Burban, MD, Jean-Pierre Cebron, MD and Daniel Gras; CHU Nantes—Selim Abbey, MD and Gilles Landes, MD; and CHU Angers: Jean-Marc Dupuis, MD and Aude Tassin, MD.
Author information
Authors and Affiliations
Corresponding author
Additional information
Editor’s note
This study examines the behaviour of the PR interval in patients with sinus node dysfunction who have functional AAIR pacing. The study has particular relevance at this time because of the current emphasis on avoidance of (right) ventricular pacing in dual-chamber pacing systems. The investigators randomized 79 patients to lower rate atrial pacing (60 bpm) with dual sensors (accelerometer and minute ventilation), minimal slope and higher rate atrial pacing (70 bpm) with dual sensor, optimized slope. Follow-up was at 1 month after which the patients were crossed over and followed for another month. Stored data within the device regarding AV conduction time, AV block point and AV conduction time adaptation during exercise were the parameters analyzed in a new mode (SafeR™, Sorin CRM SAS, Clamart, France) that allows AV conduction assessment through continuous analysis, with DDDR pacing programmed only after specific, but programmable, PR/AR durations and/or P waves not followed by QRS complexes. Patients in the higher atrial pacing arm had longer AV conduction times as well as greater incidence of development of AV blocks. The actual mechanism is not always immediately clear in any given patient, although there is an effect of beta-blockers, intra-atrial conduction delays, and AV nodal-His conduction abnormalities on the development of AV blocks at the higher atrial pacing rates.
The potential deleterious effects of AAIR pacing during exercise have been recognized previously and consist not only of the development of second and higher degrees of AV block but also inappropriately long AR conduction times, which could be hemodynamically detrimental if not actually destabilizing. The authors, by means of the algorithm described in this study have added data to existing literature and lead one to conclude that AAIR-based pacing can be detrimental in patients with sinus node dysfunction. The importance of this work is the revisiting of the “goal” of minimizing ventricular pacing at all costs, indicating that this may well not be universally warranted.
This investigation was not designed to determine clinical outcomes over time, and was quite small. Nonetheless, the data are highly provocative and warrant a larger study.
Rights and permissions
About this article
Cite this article
Mabo, P., Cebron, JP., Solnon, A. et al. Non-physiological increase of AV conduction time in sinus disease patients programmed in AAIR-based pacing mode. J Interv Card Electrophysiol 35, 219–226 (2012). https://doi.org/10.1007/s10840-012-9703-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-012-9703-4