Abstract
Background
Conduction disorders and permanent pacemaker (PPM) implantation are common complications in patients undergoing transcatheter aortic valve implantation (TAVI). Previous studies, evaluating small populations, have identified several different predictors of PPM implantation after TAVI. The aim of this study was to assess the incidence rate of conduction disorders and the predictors of postoperative PPM requirement in a large series of patients undergoing TAVI.
Methods
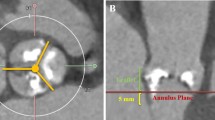
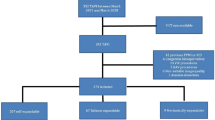
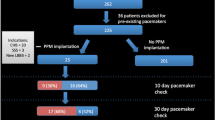
Data were analyzed from 181 consecutive patients at high-risk surgery who underwent TAVI at our institute between July 2007 and April 2011. All patients underwent implantation of the third-generation percutaneous self-expanding CoreValve® prosthesis (CoreValve, Inc., Irvine, CA, USA). In all patients, a 12-lead electrocardiogram and a 24-h holter monitoring was recorded before and after the procedure in order to assess the presence of conduction disorders. Clinical data, preoperative conduction disorders, echocardiographic patterns, and procedural data were tested as predictors of PPM implantation after TAVI.
Results
Left bundle branch block (LBBB) was the most common conduction disorder, with an incidence of 50.3% at discharge. Fifty-two (32.1%) patients developed a persistent complete AVB requiring PPM implantation. PPM implantation was strongly correlated with the presence of preoperative right bundle branch block (RBBB) which was found to be the only independent predictor of PPM implantation (HR 16.5, CI 3.3–82.3, p < 0.001).
Conclusions
LBBB and PPM implantation requirement after TAVI are common occurrences using the self-expanding CoreValve prosthesis. In this large series of consecutive patients, only RBBB was found to be a strong predictor of PPM requirement.

Similar content being viewed by others
References
Leon, M. B., Smith, C. R., Mack, M., Miller, D. C., Moses, J. W., Svensson, L. G., et al. (2010). Transcatheter aortic-valve implantation for aortic stenosis in patients who cannot undergo surgery. The New England Journal of Medicine, 363(17), 1597–1607.
Cribier, A., Eltchaninoff, H., Tron, C., Bauer, F., & Gerber, L. (2006). Percutaneous implantation of aortic valve prosthesis in patients with calcific aortic stenosis: technical advances, clinical results and future strategies. The Journal of Invasive Cardiology, 19, S88–S96.
Lichtenstein, S. V., Cheung, A., Ye, J., Thompson, C. R., Carere, R. G., Pasupati, S., et al. (2006). Transapical transcatheter aortic valve implantation in humans: initial clinical experience. Circulation, 114, 591–596.
Webb, J. G., Pasupati, S. J., Humphries, K., Thompson, C., Altwegg, L., Moss, R., et al. (2007). Percutaneous transarterial aortic valve replacement in selected high risk patients with aortic stenosis. Circulation, 116, 755–763.
Walther, T. F. V., Kempfert, J., Borger, M. A., Fassl, J., Chu, M. W., Schuler, G., et al. (2008). Transapical minimally invasive aortic valve implantation; the initial 50 patients. European Journal of Cardio-Thoracic Surgery, 33, 983–988.
Grube, E., Schuler, G., Buellesfeld, L., Gerckens, U., Linke, A., Wenaweser, P., et al. (2007). Percutaneous aortic valve replacement for severe aortic stenosis in high-risk patients using the second and current third generation self-expanding CoreValve prosthesis: device success and 30 day outcome. Journal of the American College of Cardiology, 50, 69–76.
Yan, T. D., Cao, C., Martens-Nielsen, J., Padang, R., Ng, M., Vallely, M. P., et al. (2010). Transcatheter aortic valve implantation for high-risk patients with severe aortic stenosis: A systematic review. Journal of Thoracic and Cardiovascular Surgery, 139, 1519–1528.
Webb, J. G., Altwegg, L., Boone, R. H., Cheung, A., Ye, J., Lichtenstein, S., et al. (2009). Transcatheter aortic valve implantation: impact on clinical and valve-related outcomes. Circulation, 16(119), 3009–3016.
Calvi, V., Puzzangara, E., Pruiti, G. P., Conti, S., Di Grazia, A., Ussia, G. P., et al. (2009). Early conduction disorders following percutaneous aortic valve replacement. Pacing and Clinical Electrophysiology, 32, S126–S130.
Piazza, N., Onuma, Y., Jesserun, E., Kint, P. P., Maugenest, A. M., Anderson, R. H., et al. (2008). Early and persistent intraventricular conduction abnormalities and requirements for pacemaking after percutaneous replacement of the aortic valve. JACC. Cardiovascular Interventions, 1, 310–316.
Sinhal, A., Altwegg, L., Pasupati, S., Humphries, K. H., Allard, M., Martin, P., et al. (2008). Atrioventricular block after transcatheter balloon expandable aortic valve implantation. JACC. Cardiovascular Interventions, 1, 305–309.
Jilaihawi, H., Chin, D., Vasa-Nicotera, M., Jeilan, M., Spyt, T., Ng, G. A., et al. (2009). Predictors for permanent pacemaker requirement after transcatheter aortic valve implantation with the CoreValve bioprosthesis. American Heart Journal, 157, 860–866.
Baan, J., Jr., Yong, Z. Y., Koch, K. T., Henriques, J. P., Bouma, B. J., Vis, M. M., et al. (2010). Factors associated with cardiac conduction disorders and permanent pacemaker implantation after percutaneous aortic valve implantation with the CoreValve prosthesis. American Heart Journal, 159(3), 497–503.
Bleiziffer, S., Ruge, H., Horer, J., Hutter, A., Geisbüsch, S., Brockmann, G., et al. (2010). Predictors for new-onset complete heart block after transcatheter aortic valve implantation. JACC. Cardiovascular Interventions, 3(5), 524–530.
Ferreira, N. D., Caeiro, D., Adao, L., Oliveira, M., Gonçalves, H., Ribeiro, J., et al. (2010). Incidence and predictors of permanent pacemaker requirement after transcatheter aortic valve implantation with self-expanding bioprosthesis. Pacing and Clinical Electrophysiology, 33(11), 1364–1372.
Zahn, R., Gerckens, U., Grube, E., Linke, A., Sievert, H., Eggebrecht, H., et al. (2011). Transcatheter aortic valve implantation: first results from a multi-centre real-world registry. European Heart Journal, 32(2), 198–204.
Tamburino, C., Capodanno, D., Mulè, M., Scarabelli, M., Cammalleri, V., Barbanti, M., et al. (2009). Procedural success and 30-day clinical outcomes after percutaneous aortic valve replacement using current third-generation self-expanding CoreValve prosthesis. The Journal of Invasive Cardiology, 21(3), 93–98.
Vardas, E. A., Auricchio, A., Blanc, J. J., Daubert, J. C., Drexler, H., Ector, H., et al. (2007). Guidelines for cardiac pacing and cardiac resynchronization therapy. Europace, 9, 959–998.
Cribier, A., Eltchaninoff, H., Tron, C., Bauer, F., Agatiello, C., Nercolini, D., et al. (2006). Treatment of calcific aortic stenosis with the percutaneous heart valve: mid-term follow-up from the initial feasibility studies: the French Experience. Journal of the American College of Cardiology, 47, 1214–1223.
Masson, J. B., Kovac, J., Schuler, G., Ye, J., Cheung, A., Kapadia, S., et al. (2009). Transcatheter aortic valve implantation: review of the nature, management, and avoidance of procedural complications. JACC. Cardiovascular Interventions, 2, 811–820.
Thomas, J. L., Dickstein, R. A., Parker, F. B., Jr., Potts, J. L., Poirier, R. A., Fruehan, C. T., et al. (1982). Prognostic significance of the development of left bundle conduction defects following aortic valve replacement. The Journal of Thoracic and Cardiovascular Surgery, 84, 382–386.
Del Rizzo, D. F., Nishimura, S., Lau, C., Sever, J., & Goldman, B. S. (1996). Cardiac pacing following surgery for acquired heart disease. Journal of Cardiac Surgery, 11, 332–340.
Limongelli, G., Ducceschi, V., D’Andrea, A., Renzulli, A., Sarubbi, B., De Feo, M., et al. (2003). Risk factors for pacemaker implantation following aortic valve replacement: a single centre experience. Heart, 89, 901–904.
Dawkins, S., Hobson, A. R., Kalra, P. R., Tang, A. T., Monro, J. L., & Dawkins, K. D. (2008). Permanent pacemaker implantation after isolated aortic valve replacement: incidence, indications, and predictors. The Annals of Thoracic Surgery, 85, 108–112.
Erdogan, H. B., Kayalar, N., Ardal, H., Omeroglu, S. N., Kirali, K., Guler, M., et al. (2006). Risk factors for requirement of permanent pacemaker implantation after aortic valve replacement. The Journal of Cardiac Surgery, 21, 211–215.
Merin, O., Ilan, M., Oren, A., Fink, D., Deeb, M., Bitran, D., et al. (2009). Permanent pacemaker implantation following cardiac surgery: indications and long-term follow-up. Pacing and Clinical Electrophysiology, 32, 7–12.
Fukuda, T., Hawley, R. L., & Edwards, J. E. (1976). Lesions of conduction tissue complicating aortic valvular replacement. Chest, 69, 605–614.
Koplan, A. B., Stevenson, W. G., Epstein, L. M., Aranki, S. F., & Maisel, W. H. (2003). Development and validation of a simple risk score to predict the need for permanent pacing after cardiac valve surgery. Journal of the American College of Cardiology, 41, 795–801.
Godin, M., Eltchaninoff, H., Furuta, A., Tron, C., Anselme, F., Bejar, K., et al. (2010). Frequency of conduction disturbances after transcatheter implantation of an Edwards Sapien aortic valve prosthesis. The American Journal of Cardiology, 106(5), 707–712.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Calvi, V., Conti, S., Pruiti, G.P. et al. Incidence rate and predictors of permanent pacemaker implantation after transcatheter aortic valve implantation with self-expanding CoreValve prosthesis. J Interv Card Electrophysiol 34, 189–195 (2012). https://doi.org/10.1007/s10840-011-9634-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10840-011-9634-5